Long-Term Safety and Efficacy of Ozanimod in Relapsing Multiple Sclerosis: Results from the DAYBREAK Open-Label Extension Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

11 November 2020 31. Jahrgang Neurologie Und Psychiatrie
11 November 2020 _ 31. Jahrgang November 2020 _ 31. Jahrgang_www.BVDN.de NeuroTransmitter 2020;31(11) NeuroTransmitter 11 Neurologie und Psychiatrie – Berufspolitik und Fortbildung Offizielles Organ des Berufsverbandes Deutscher Nervenärzte, des Berufsverbandes BVDN BDN BVDP Deutscher Neurologen und des Berufsverbandes Deutscher Psychiater Mitgliederbeilage zeigt diesesWas Bild? Seite 70 NEUROTRANSMITTER- TELEGRAMM Gute Zahlen für die ZNS-Fächer 16 Telekonsil im EBM Honorarbericht der KBV COVID-19-Pandemie 28 Nehmen psychische Erkrankungen zu? Therapie mit Psychedelika 32 BVDP-Ausgabe Die Rolle der Psychotherapie zum 15016 DGPPN-Kongress Bullycide 48 2020 Suizide nach Cybermobbing www.springermedizin.de/neurotransmitter »Der Alltag ist auch für uns Fachärzte für Psychiatrie und Psychotherapie nicht mehr derselbe.« Dr. med. Christa Roth-Sackenheim, Andernach Vorsitzende des BVDP Wir haben uns verändert! Liebe und sehr verehrte Kolleginnen und Kollegen, Wir haben gesehen, welche seelischen Folgen ein Lockdown und die soziale Isolation auf psychisch belastbare und gut es freut mich, Ihnen hiermit wieder die DGPPN-Kongressaus- resiliente Menschen haben kann, aber auch, wie dies unseren gabe des NeuroTransmitter präsentieren zu dürfen. Das dies- Patienten eine zusätzliche Bürde auferlegte. jährige Motto der Veranstaltung wurde schon vor über einem Wir haben Sie mit den Webinaren unserer Berusverbände Jahr festgelegt und lautet: „Psychiatrie und Psychotherapie in zur Praxisführung in der COVID-19-Pandemie und zur Heim- der sozialen Lebenswelt“. Genau genommen bekommt dieses versorgung, um nur zwei Temen zu nennen, zahlreich er- Motto jetzt auch noch einen Untertitel: „Wie hat Corona die reicht. Ihre Fragen an uns haben uns gezeigt, wie sehr Sie um soziale Lebenswelt verändert?“ eine verlässliche Versorgung, aber ebenso um Ihren eigenen Wie sehr hat sich in der Tat die gesamte Welt seit dem letz- Schutz gerungen haben und das teilweise noch immer tun. -

Emerging Therapies Are Interesting and Exciting! But…
Goodbye Needles! M. Anthony Sofia, MD Assistant Professor of Medicine Division of Gastroenterology and Hepatology Oregon Health and Science University @AnthonySofiaMD Tuesday February 26 th, 2019 Disclosures • None 2 Disclaimer Emerging therapies are interesting and exciting! But… Many of the medications I will discuss are still in early clinical development. They are not FDA approved for these indications and studies are ongoing. Safety and efficacy still needs to be clarified and ultimately judged according to pivotal trial data prior to broad application in IBD. Clinical trials are enrolling and require informed consent with a knowledgeable physician in the field. 3 Outline • Review currently available therapies • Introduce investigational treatments • FDA drug development pathway – Example development histories • Small molecule inhibitors – New and developing therapeutics • Fecal microbiota transplant – Promises, concerns, and (many) unresolved questions 4 Current Medications for IBD (Circa 1/1/2018) Sulfasalazine 5-ASA Mesalamine Oral/Enema/Suppository Prednisone Corticosteroids Budesonide Foams/Enemas/Suppository Azathioprine/6MP Immunomodulators Cyclosporine Tacrolimus Infliximab Adalimumab Certolizumab pegol Biologics Golimumab Vedolizumab 5 Ustekinumab Therapies in Development (Circa 3/1/2019) Tofacitinib* Filgotinib Upadacitinib Janus Kinase (JAK) Itacitinib Inhibition PF-06700841 BMS-986165 TD-1473 PF-6651600 Sphingosine-1-phosphate (S1P) Ozanimod Etrasimod Modulation Amiselimod Selective Integrin AJM300 Therapy Enemas Fecal -

Helsana Arzneimittelreport 2020
Aussgabe 2020 Helsana- Arzneimittel- Report Ausgabe 2020 Helsana-Arzneimittelreport Geduld ist eine gute Eigenschaft. Aber nicht, wenn es um die Beseitigung von Missständen geht. Margaret Thatcher, ehem. Premierministerin des Vereinigten Königreichs (1925 – 2013) Der Helsana-Arzneimittelreport wird im Auftrag von Helsana vom Universitätsspital Basel (USB) und dem Institut für Pharmazeutische Medizin (ECPM) der Universität Basel erstellt. Unser Dank gilt den Mitarbeiterinnen und Mitarbeitern des USB und des ECPM für alle vorgenommenen Auswertungen und für die Erstellung des Reports. Helsana-Arzneimittelreport 2020 3 November 2020 Helsana-Arzneimittelreport für die Schweiz 2020 Auswertungsergebnisse der Helsana Arzneimitteldaten aus den Jahren 2016 bis 2019 Nadine Schur 1 Sibylle Twerenbold 2,3 Daphne Reinau 2,3 Matthias Schwenkglenks 1 Christoph R. Meier 2,3,4 1 Institut für Pharmazeutische Medizin (ECPM) Universität Basel & 2 Basel Pharmacoepidemiology Unit Abteilung Klinische Pharmazie und Epidemiologie Departement Pharmazeutische Wissenschaften Universität Basel & 3 Spital-Pharmazie Universitätsspital Basel & 4 Boston Collaborative Drug Surveillance Program (BCSDP) Lexington, MA, USA Helsana-Arzneimittelreport 2020 4 Helsana-Arzneimittelreport 2020 5 Inhaltsverzeichnis Vorwort .............................................................................................................................................................. 7 Préface ............................................................................................................................................................. -

Ozanimod to Treat Relapsing Forms of Multiple Sclerosis: a Comprehensive Review of Disease, Drug Efficacy and Side Effects
Review Ozanimod to Treat Relapsing Forms of Multiple Sclerosis: A Comprehensive Review of Disease, Drug Efficacy and Side Effects Grace Lassiter 1,*, Carlie Melancon 2, Tyler Rooney 2 , Anne-Marie Murat 2, Jessica S. Kaye 3, Adam M. Kaye 3 , Rachel J. Kaye 4, Elyse M. Cornett 5, Alan D. Kaye 5, Rutvij J. Shah 5,6, Omar Viswanath 5,7,8,9 and Ivan Urits 5,10 1 School of Medicine, Georgetown University, Washington, DC 20007, USA 2 School of Medicine, Louisiana State University Shreveport, Shreveport, LA 71103, USA; [email protected] (C.M.); [email protected] (T.R.); [email protected] (A.-M.M.) 3 Department of Pharmacy Practice, Thomas J. Long School of Pharmacy and Health Sciences, University of the Pacific, Stockton, CA 95211, USA; [email protected]fic.edu (J.S.K.); akaye@pacific.edu (A.M.K.) 4 School of Medicine, Medical University of South Carolina, Charleston, SC 29425, USA; [email protected] 5 Department of Anesthesiology, Louisiana State University Shreveport, Shreveport, LA 71103, USA; [email protected] (E.M.C.); [email protected] (A.D.K.); [email protected] (R.J.S.); [email protected] (O.V.); [email protected] (I.U.) 6 Department of Neurology, Louisiana State University Shreveport, Shreveport, LA 71103, USA 7 College of Medicine-Phoenix, University of Arizona, Phoenix, AZ 85724, USA 8 Department of Anesthesiology, School of Medicine, Creighton University, Omaha, NE 68124, USA 9 Valley Anesthesiology and Pain Consultants—Envision Physician Services, Phoenix, AZ 85004, USA 10 Southcoast Health, Southcoast Physicians Group Pain Medicine, Wareham, MA 02571, USA * Correspondence: [email protected] Received: 23 October 2020; Accepted: 1 December 2020; Published: 3 December 2020 Abstract: Multiple sclerosis (MS) is a prevalent and debilitating neurologic condition characterized by widespread neurodegeneration and the formation of focal demyelinating plaques in the central nervous system. -

Application Number
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209899Orig1s000 OTHER REVIEW(S) Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research | Office of Surveillance and Epidemiology (OSE) Epidemiology: ARIA Sufficiency Date: March 25, 2020 Reviewer: Silvia Perez-Vilar, PharmD, PhD Division of Epidemiology I Team Leader: Catherine Callahan, PhD, MA Division of Epidemiology I Deputy Division Director: CAPT Sukhminder K. Sandhu, PhD, MPH, MS Division of Epidemiology I Subject: ARIA Sufficiency Memo for Pregnancy Safety Concerns Drug Name: ZEPOSIA (Ozanimod) Application Type/Number: NDA 209899 Applicant/sponsor: Celgene Corporation OSE RCM #: 2020-308 Page 1 of 7 Reference ID: 4580671 Expedited ARIA Sufficiency for Pregnancy Safety Concerns 1. BACKGROUND INFORMATION 1.1. Medical Product Ozanimod (ZEPOSIA, Celgene Corporation) is a sphingosine-1-phosphate (S1P) receptor agonist, which binds selectively to S1P subtypes 1 (S1P1) and 5 (S1P5). It is a new molecular entity (NME) and is currently not approved or marketed in any country. The proposed indication is the treatment of relapsing forms of multiple sclerosis (MS). The mechanism by which ozanimod exerts therapeutic effects in relapsing MS may involve reduction of lymphocyte migration into the central nervous system. Ozanimod is administered orally. The proposed maintenance dose of ozanimod is 1 mg per day after a seven-day dose escalation (0.25 mg per day on days 1 to 4, 0.5 mg per day on days 5 to 7). 1 Ozanimod is extensively metabolized in humans to several circulating active metabolites, including CC112273 and CC1084037. 2 The half-life of ozanimod is approximately 20 hours, while the half-life of CC112273 and CC1084037 is about 280 hours, leading to accumulation of these active metabolites (relative to the parent) after multiple dosing. -

Safety of Newer Disease Modifying Therapies in Multiple Sclerosis
Review Safety of Newer Disease Modifying Therapies in Multiple Sclerosis Georges Jalkh 1,2 , Rachelle Abi Nahed 1,2, Gabrielle Macaron 1,2,3 and Mary Rensel 3,* 1 Department of Neurology, Faculty of Medicine, Université Saint Joseph, Beirut B.P. 11-5076, Lebanon; [email protected] (G.J.); [email protected] (R.A.N.); [email protected] (G.M.) 2 Department of Neurology, Hotel-Dieu de France Hospital, Beirut 16-6830, Lebanon 3 Mellen Center for Multiple Sclerosis, Neurological Institute, Cleveland Clinic Foundation, Cleveland, OH 44195, USA * Correspondence: [email protected]; Tel.: +1-216-312-4219 Abstract: In the past decade, the therapeutic arsenal for multiple sclerosis has expanded greatly. Newer more potent disease modifying therapies (DMTs) with varying mechanisms of actions are increasingly used early in the disease course. These newer DMTs include oral therapies (terifluno- mide, dimethyl fumarate, fingolimod, siponimod, ozanimod, and cladribine) and infusion therapies (natalizumab, alemtuzumab, and ocrelizumab), and are associated with better control of disease ac- tivity and long-term outcomes in patients with MS compared to older injectable therapies (interferon beta and glatiramer acetate). However, they are associated with safety concerns and subsequent monitoring requirements. Adverse events are initially observed in phase 2 and 3 clinical trials, and further long-term data are collected in phase 3 extension studies, case series, and post-marketing reports, which highlight the need to periodically re-evaluate and adjust monitoring strategies to optimize treatment safety in an individualized approach. Keywords: multiple sclerosis; disease modifying therapies; safety; long-term outcomes Citation: Jalkh, G.; Abi Nahed, R.; 1. -

Celgene Bets Big on Scripps-Originated Autoimmunity Candidate
NEWS & ANALYSIS BIOBUSINESS BRIEFS DEAL WATCH Celgene bets big on Scripps-originated autoimmunity candidate In its third major acquisition in 3 months, relapsing–remitting multiple sclerosis — Celgene is buying the biotech company fingolimod (Novartis) — and by two others Receptos for US$7.2 billion. In doing so, that are in Phase III trials, siponimod Celgene adds two clinical-stage drug (Novartis) and ponesimod (Actelion). candidates for treating autoimmune diseases to In Europe, fingolimod is only approved for its portfolio, including one — ozanimod — that patients with active disease for whom originated from the US National Institutes of interferon‑β and glatiramer acetate are not Health (NIH) Molecular Libraries Program (MLP). effective. Safety issues with fingolimod — “This is a very rare example of a compound that most notably, fatal infections with varicella Ryan McVay/Photodisc was discovered in academia and has made it zoster virus and decreases in heart rate, into Phase III,” says Hugh Rosen, a professor both of which were observed in clinical trials at The Scripps Research Institute (TSRI) in San — mean there is room for improvement Diego, USA, who co‑discovered ozanimod. among S1PR-targeting compounds. “It looks In 2009, Receptos licensed a series of to me like the cardiac side effects are a bit compounds identified in the laboratories of less with ozanimod,” says Bernhard Hemmer, Rosen and his colleague, Edward Roberts, a professor at Technische Universität from TSRI. The researchers had screened München, Munich, Germany, and an expert the NIH MLP collection to identify allosteric in multiple sclerosis. However, he cautions, agonists of the sphingosine-1-phosphate “one has to see how the drug performs in receptor 1 (S1PR1). -

Public Assessment Report
Amsterdam, 9 April 2020 EMA/CHMP/199869/2020 Rev 2 Committee for Medicinal Products for Human Use (CHMP) Assessment report Zeposia International non-proprietary name: ozanimod Procedure No. EMEA/H/C/004835/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 9 1.1. Submission of the dossier ...................................................................................... 9 1.2. Steps taken for the assessment of the product ....................................................... 10 2. Scientific discussion .............................................................................. 12 2.1. Problem statement ............................................................................................. 12 2.1.1. Disease or condition ......................................................................................... 12 2.1.2. Epidemiology .................................................................................................. 12 2.1.3. Aetiology and pathogenesis ............................................................................. -
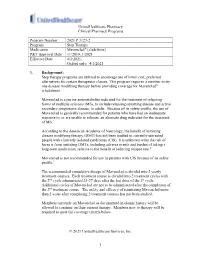
Mavenclad® (Cladribine) P&T Approval Date 11/2019, 1/2021 Effective Date 4/1/2021; Oxford Only: 4/1/2021
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2021 P 3123-2 Program Step Therapy Medication Mavenclad® (cladribine) P&T Approval Date 11/2019, 1/2021 Effective Date 4/1/2021; Oxford only: 4/1/2021 1. Background: Step therapy programs are utilized to encourage use of lower cost, preferred alternatives for certain therapeutic classes. This program requires a member to try one disease modifying therapy before providing coverage for Mavenclad® (cladribine). Mavenclad is a purine antimetabolite indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include relapsing-remitting disease and active secondary progressive disease, in adults. Because of its safety profile, the use of Mavenclad is generally recommended for patients who have had an inadequate response to, or are unable to tolerate, an alternate drug indicated for the treatment of MS.1 According to the American Academy of Neurology, the benefit of initiating disease modifying therapy (DMT) has not been studied in currently untreated people with clinically isolated syndromes (CIS). It is unknown what the risk of harm is from initiating DMTs, including adverse events and burden of taking a long-term medication, relative to the benefit of reducing relapse rate.2 Mavenclad is not recommended for use in patients with CIS because of its safety profile.1 The recommended cumulative dosage of Mavenclad is divided into 2 yearly treatment courses. Each treatment course is divided into 2 treatment cycles with the 2nd cycle administered 23-27 days after the last dose of the 1st cycle. Additional cycles of Mavenclad are not to be administered after the completion of the 2nd treatment course. -

PDL DRUG REVIEW Proprietary Name: Zeposia® Common Name: Ozanimod PDL Category: Multiple Sclerosis Agents
PDL DRUG REVIEW Proprietary Name: Zeposia® Common Name: ozanimod PDL Category: Multiple Sclerosis Agents Comparable Products Preferred Drug List Status Gilenya Preferred with Conditions Mayzent Non‐Preferred with Conditions Summary Pharmacology/Usage: Ozanimod, the active ingredient of Zeposia®, is a sphingosine 1‐phosphate (S1P) receptor modulator that binds with high affinity to S1P receptors 1 and 5. It blocks the capacity of lymphocytes to egress from lymph nodes, reducing the number of lymphocytes in peripheral blood. The mechanism by which it exerts its therapeutic effects in multiple sclerosis is not known but may involve the reduction of lymphocyte migration into the CNS. Indication: For the treatment of relapsing forms of multiple sclerosis (MS) to include clinically isolated syndrome, relapsing‐ remitting disease, and active secondary progressive disease, in adults. There is no pregnancy category for this medication; however, the risk summary indicates that there are no adequate data on the developmental risk associated with use in pregnant women. In animal studies, use during pregnancy produced adverse effects on development, in the absence of maternal toxicity. Before initiation of Zeposia®, women of childbearing potential should be counseled on the potential for a serious risk to the fetus and the need for contraception during treatment with Zeposia®. Because of the time it takes to eliminate the drug from the body after stopping treatment, the potential risk to the fetus may persist and women of childbearing age should also use effective contraception for 3 months after stopping Zeposia®. The safety and efficacy of use in the pediatric population have not been established. Dosage Form: Capsules: 0.23mg, 0.46mg, and 0.92mg Recommended Dosage: Before initiation of treatment, assess the following: Complete blood count: obtain a recent (i.e. -

Nebraska Medicaid Preferred Drug List with Prior Authorization Criteria
Nebraska Medicaid Preferred Drug List with Prior Authorization Criteria PDL Updated August 2, 2021 Highlights indicated change from previous posting For the most up to date list of covered drugs consult the Drug Lookup on the Nebraska Medicaid Website at https://druglookup.fhsc.com/druglookupweb/?client=nestate • Opioids- The maximum opioid dose covered will decrease from 120 Morphine Milligram Equivalents (MME) per day to 90 Morphine Milligram Equivalents (MME) per day. (beginning December 1, 2020) Non-Preferred Drug Coverage Class and drug-specific therapeutic trial and failure requirements are found within this document. Examples of non-preferred exception criteria include: . Adverse reaction to preferred drugs . Allergy to preferred drugs . Contraindication to preferred drugs . Documentation of inability to swallow solid dosage forms Specific Class Prior Authorization forms can be found within the PDL class listings and at: https://nebraska.fhsc.com/priorauth/paforms.asp . Buprenorphine Products PA Form . Buprenorphine Products Informed Consent . Growth Hormone PA Form . HAE Treatments PA Form . Hepatitis C PA Form For all other class medically-necessary coverage, quantity, and high dose requests use the following: . Documentation of Medical Necessity PA Form For a complete list of Claims Limitations visit: https://nebraska.fhsc.com/Downloads/neclaimlimitations.pdf Nebraska Medicaid Preferred Drug List with Prior Authorization Criteria PDL Updated August 2, 2021 Highlights indicated change from previous posting ACNE AGENTS, TOPICAL -

Ozanimod 0.5 Mg Or 1 Mg Ozanimod Daily, Or Weekly Injections of Interferon Beta-1A
VOLUME 44 : NUMBER 2 : APRIL 2021 NEW DRUGS randomised to receive oral ozanimod 0.5 mg or 1 mg Ozanimod daily, or weekly injections of interferon beta‑1a. The primary outcome of the trials was the annualised rate Approved indication: multiple sclerosis of relapse. Brain lesions were evaluated by MRI and Aust Prescr 2021;44:65–6 Zeposia (Celgene) disability was assessed using the Expanded Disability https://doi.org/10.18773/ 230, 460 and 920 microgram capsules Status Scale.1,2 austprescr.2021.013 First published In the SUNBEAM trial, 1346 patients were randomised The pathophysiology of multiple sclerosis is thought to 10 March 2021 involve the migration of lymphocytes into the central and treated for an average of about 13.5 months. nervous system. This has led to drugs that alter the Approximately 93% of the patients completed the Related article: study. The annualised relapse rate was 0.24 with immune system being used in the management of Siponimod for multiple patients with multiple sclerosis. In the 1990s interferons ozanimod 0.5 mg and 0.18 with ozanimod 1 mg. These sclerosis were used, followed by injectable monoclonal rates were lower than the rate of 0.35 with interferon antibodies, such as alemtuzumab, in the 2000s. Later, beta‑1a. The number of new or enlarging lesions seen 1 oral drugs such as fingolimod were developed. on MRI was also lower with ozanimod. Like fingolimod, ozanimod is aimed at the sphingosine The RADIANCE trial randomised 1320 patients and 1‑phosphate (S1P) receptors on the surface of treated them for two years.