Resistance to Hepatitis C Virus: Potential Genetic and Immunological Determinants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sample Lab Report
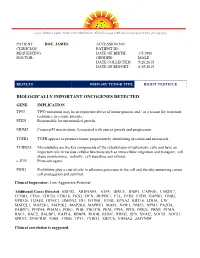
3030 Venture Lane, Suite 108 ● Melbourne, Florida 32934 ● Phone 321-253-5197 ● Fax 321-253-5199 PATIENT: DOE, JAMES ACCESSION NO: CLINICIAN/ PATIENT ID: REQUESTING DATE OF BIRTH: 1/5/1986 DOCTOR: GENDER: MALE DATE COLLECTED: 5/26/2015 DATE OF REPORT: 6/15/2015 RESULTS PRIMARY TUMOR TYPE RIGHT TESTICLE BIOLOGICALLY IMPORTANT ONCOGENES DETECTED GENE IMPLICATION TP53 TP53 mutations may be an important driver of tumorigenesis and / or a reason for treatment resistance in a some patients. PTEN Responsible for uncontrolled growth. MDM2 Causes p53 inactivation. Associated with cancer growth and progression. TGFB1 TGFB appears to promote tumor progession by stimulating invasion and metastasis. TUBB2A Microtubules are the key components of the cytoskeleton of eukaryotic cells and have an important role in various cellular functions such as intracellular migration and transport, cell shape maintenance, polarity, cell signaling and mitosis. c-JUN Proto-oncogene PHB2 Prohibitins play a crucial role in adhesion processes in the cell and thereby sustaining cancer cell propagation and survival. Clinical Impression: Low Aggressive Potential Additional Genes Detected: ABCG2, ARHGAP5, ATF4, BIRC5, BNIP3, CAPNS1, CARD17, CCNB1, CD24, CDC20, CDK18, CKS2, DCN, DEPDC1, FTL, FZD5, FZD9, GAPDH, GNB2, GPR126, H2AFZ, HDAC1, HMGN2, ID1, IFITM1, JUNB, KPNA2, KRT18, LDHA, LTF, MAD2L1, MAP2K1, MAP2K2, MAP2K4, MAPRE1, MAS1, NME1, NME3, NPM1, PA2G4, PABPC1, PFDN4, PGAM1, PGK1, PHB, PIK3CB, PKM, PPIA, PPIH, PRKX, PRNP, PTMA, RAC1, RAC2, RALBP1, RAP1A, RBBP4, RHOB, RHOC, -
Conditional Ablation of P130cas/BCAR1 Adaptor Protein
Camacho Leal et al. Cell Communication and Signaling (2018) 16:73 https://doi.org/10.1186/s12964-018-0289-z RESEARCH Open Access Conditional ablation of p130Cas/BCAR1 adaptor protein impairs epidermal homeostasis by altering cell adhesion and differentiation Maria del Pilar Camacho Leal†, Andrea Costamagna†, Beatrice Tassone, Stefania Saoncella, Matilde Simoni, Dora Natalini, Aurora Dadone, Marianna Sciortino, Emilia Turco, Paola Defilippi, Enzo Calautti‡ and Sara Cabodi*‡ Abstract Background: p130 Crk-associated substrate (p130CAS; also known as BCAR1) is a scaffold protein that modulates many essential cellular processes such as cell adhesion, proliferation, survival, cell migration, and intracellular signaling. p130Cas has been shown to be highly expressed in a variety of human cancers of epithelial origin. However, few data are available regarding the role of p130Cas during normal epithelial development and homeostasis. Methods: To this end, we have generated a genetically modified mouse in which p130Cas protein was specifically ablated in the epidermal tissue. Results: By using this murine model, we show that p130Cas loss results in increased cell proliferation and reduction of cell adhesion to extracellular matrix. In addition, epidermal deletion of p130Cas protein leads to premature expression of “late” epidermal differentiation markers, altered membrane E-cadherin/catenin proteins localization and aberrant tyrosine phosphorylation of E-cadherin/catenin complexes. Interestingly, these alterations in adhesive properties in absence -

Expression Profiling of KLF4
Expression Profiling of KLF4 AJCR0000006 Supplemental Data Figure S1. Snapshot of enriched gene sets identified by GSEA in Klf4-null MEFs. Figure S2. Snapshot of enriched gene sets identified by GSEA in wild type MEFs. 98 Am J Cancer Res 2011;1(1):85-97 Table S1: Functional Annotation Clustering of Genes Up-Regulated in Klf4 -Null MEFs ILLUMINA_ID Gene Symbol Gene Name (Description) P -value Fold-Change Cell Cycle 8.00E-03 ILMN_1217331 Mcm6 MINICHROMOSOME MAINTENANCE DEFICIENT 6 40.36 ILMN_2723931 E2f6 E2F TRANSCRIPTION FACTOR 6 26.8 ILMN_2724570 Mapk12 MITOGEN-ACTIVATED PROTEIN KINASE 12 22.19 ILMN_1218470 Cdk2 CYCLIN-DEPENDENT KINASE 2 9.32 ILMN_1234909 Tipin TIMELESS INTERACTING PROTEIN 5.3 ILMN_1212692 Mapk13 SAPK/ERK/KINASE 4 4.96 ILMN_2666690 Cul7 CULLIN 7 2.23 ILMN_2681776 Mapk6 MITOGEN ACTIVATED PROTEIN KINASE 4 2.11 ILMN_2652909 Ddit3 DNA-DAMAGE INDUCIBLE TRANSCRIPT 3 2.07 ILMN_2742152 Gadd45a GROWTH ARREST AND DNA-DAMAGE-INDUCIBLE 45 ALPHA 1.92 ILMN_1212787 Pttg1 PITUITARY TUMOR-TRANSFORMING 1 1.8 ILMN_1216721 Cdk5 CYCLIN-DEPENDENT KINASE 5 1.78 ILMN_1227009 Gas2l1 GROWTH ARREST-SPECIFIC 2 LIKE 1 1.74 ILMN_2663009 Rassf5 RAS ASSOCIATION (RALGDS/AF-6) DOMAIN FAMILY 5 1.64 ILMN_1220454 Anapc13 ANAPHASE PROMOTING COMPLEX SUBUNIT 13 1.61 ILMN_1216213 Incenp INNER CENTROMERE PROTEIN 1.56 ILMN_1256301 Rcc2 REGULATOR OF CHROMOSOME CONDENSATION 2 1.53 Extracellular Matrix 5.80E-06 ILMN_2735184 Col18a1 PROCOLLAGEN, TYPE XVIII, ALPHA 1 51.5 ILMN_1223997 Crtap CARTILAGE ASSOCIATED PROTEIN 32.74 ILMN_2753809 Mmp3 MATRIX METALLOPEPTIDASE -

Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration Through Promotion of P130cas Membrane Localization Andmembrane Ruffling
Research Article Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration through Promotion of p130Cas Membrane Localization andMembrane Ruffling Randy S. Schrecengost,1 Rebecca B. Riggins,2 Keena S. Thomas,1 Michael S. Guerrero,1 and Amy H. Bouton1 1Department of Microbiology, University of Virginia Health System, Charlottesville, Virginia and 2Department of Oncology, Lombardi Comprehensive Cancer Center, Georgetown University, Washington, District of Columbia Abstract antiestrogen resistance-1 (BCAR1; also known as p130Cas; refs. 2, 3). Antiestrogens such as tamoxifen are widely used in the clinic A second protein, BCAR3 (the human homologue of the murine to treat estrogen receptor–positive breast tumors. Resistance protein AND-34), was identified in a genetic screen along with to tamoxifen can occur either de novo or develop over time in BCAR1 as a gene product whose overexpression conferred tamoxifen resistance in vitro (4). BCAR3 is a member of the novel a large proportion of these tumors. Additionally, resistance is S p associated with enhanced motility and invasiveness in vitro. rc homology 2 (SH2)–containing rotein (NSP) family that One molecule that has been implicated in tamoxifen resis- includes two other members, Chat/SHEP1 and NSP1. These tance, breast cancer antiestrogen resistance-3 (BCAR3), has proteins share a common domain structure consisting of an also been shown to regulate migration of fibroblasts. In this amino-terminal SH2 domain and a carboxyl-terminal domain with study, we investigated the role of BCAR3 in breast cancer cell sequence homology to the Cdc25-family of guanine nucleotide exchange factors (GEF). Several studies have shown that BCAR3 migration and invasion. -

High BCAR1 Expression Is Associated with Early PSA Recurrence in ERG Negative Prostate Cancer Asmus Heumann1†, Nina Heinemann1†, Claudia Hube-Magg1, Dagmar S
Heumann et al. BMC Cancer (2018) 18:37 DOI 10.1186/s12885-017-3956-3 RESEARCHARTICLE Open Access High BCAR1 expression is associated with early PSA recurrence in ERG negative prostate cancer Asmus Heumann1†, Nina Heinemann1†, Claudia Hube-Magg1, Dagmar S. Lang1, Katharina Grupp2, Martina Kluth1, Sarah Minner1, Christina Möller-Koop1,MarkusGraefen3, Hans Heinzer3, Maria Christina Tsourlakis1, Waldemar Wilczak1, Corinna Wittmer1,FrankJacobsen1,HartwigHuland3, Ronald Simon1* ,ThorstenSchlomm3,4, Guido Sauter1, Stefan Steurer1,PatrickLebok1 and Andrea Hinsch1 Abstract Background: Breast cancer anti-estrogen resistance 1 (BCAR1/p130cas) is a hub for diverse oncogenic signaling cascades and promotes tumor development and progression. Methods: To understand the effect of BCAR1 in prostate cancer, we analyzed its expression on more than 11,000 prostate cancer samples. BCAR1 expression levels were compared with clinical characteristics, PSA recurrence, molecular subtype defined by ERG status and 3p, 5q, 6q and PTEN deletion. Results: BCAR1 staining was barely detectable in normal prostate glands but seen in 77.6% of 9472 interpretable cancers, including strong expression in 38.5%, moderate in 23.2% and weak in 15.9% of cases. BCAR1 up regulation was associated with positive ERG status (p < 0.0001), high Gleason score (p < 0.0001), advanced pathological tumor stage (p = 0.0082), lower preoperative PSA level (p < 0.0001), increased cell proliferation (p < 0.0001), early PSA recurrence (p = 0.0008), and predicted prognosis independently from clinico-pathological parameters available at the time of the initial biopsy. However, subset analyses revealed that the prognostic impact of BCAR1 expression was limited to ERG-negative cancer. That BCAR1 up regulation was linked to almost all analyzed deletions (p < 0.0001 each for PTEN, 5q, 6q deletion) may suggest a functional link to genomic instability. -

PTK2 Antibody (Center) Blocking Peptide Synthetic Peptide Catalog # Bp8614c
10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 PTK2 Antibody (Center) Blocking Peptide Synthetic peptide Catalog # BP8614c Specification PTK2 Antibody (Center) Blocking Peptide - PTK2 Antibody (Center) Blocking Peptide - Background Product Information PTK2 is a cytoplasmic protein tyrosine kinase Primary Accession Q05397 which is found concentrated in the focal adhesions that form between cells growing in the presence of extracellular matrix PTK2 Antibody (Center) Blocking Peptide - Additional Information constituents. This protein is a member of the FAK subfamily of protein tyrosine kinases but lacks significant sequence similarity to kinases Gene ID 5747 from other subfamilies. Other Names PTK2 Antibody (Center) Blocking Peptide - Focal adhesion kinase 1, FADK 1, Focal References adhesion kinase-related nonkinase, FRNK, Protein phosphatase 1 regulatory subunit Calalb,M.B., et.al., Mol. Cell. Biol. 15 (2), 71, PPP1R71, Protein-tyrosine kinase 2, 954-963 (1995)Polte,T.R. et.al., Proc. Natl. p125FAK, pp125FAK, PTK2, FAK, FAK1 Acad. Sci. U.S.A. 92 (23), 10678-10682 Target/Specificity (1995)Gervais,F.G., et.al., J. Biol. Chem. 273 The synthetic peptide sequence used to (27), 17102-17108 (1998) generate the antibody <a href=/products/AP8614c>AP8614c</a> was selected from the Center region of human PTK2. A 10 to 100 fold molar excess to antibody is recommended. Precise conditions should be optimized for a particular assay. Format Peptides are lyophilized in a solid powder format. Peptides can be reconstituted in solution using the appropriate buffer as needed. Storage Maintain refrigerated at 2-8°C for up to 6 months. -

The Human Gene Connectome As a Map of Short Cuts for Morbid Allele Discovery
The human gene connectome as a map of short cuts for morbid allele discovery Yuval Itana,1, Shen-Ying Zhanga,b, Guillaume Vogta,b, Avinash Abhyankara, Melina Hermana, Patrick Nitschkec, Dror Friedd, Lluis Quintana-Murcie, Laurent Abela,b, and Jean-Laurent Casanovaa,b,f aSt. Giles Laboratory of Human Genetics of Infectious Diseases, Rockefeller Branch, The Rockefeller University, New York, NY 10065; bLaboratory of Human Genetics of Infectious Diseases, Necker Branch, Paris Descartes University, Institut National de la Santé et de la Recherche Médicale U980, Necker Medical School, 75015 Paris, France; cPlateforme Bioinformatique, Université Paris Descartes, 75116 Paris, France; dDepartment of Computer Science, Ben-Gurion University of the Negev, Beer-Sheva 84105, Israel; eUnit of Human Evolutionary Genetics, Centre National de la Recherche Scientifique, Unité de Recherche Associée 3012, Institut Pasteur, F-75015 Paris, France; and fPediatric Immunology-Hematology Unit, Necker Hospital for Sick Children, 75015 Paris, France Edited* by Bruce Beutler, University of Texas Southwestern Medical Center, Dallas, TX, and approved February 15, 2013 (received for review October 19, 2012) High-throughput genomic data reveal thousands of gene variants to detect a single mutated gene, with the other polymorphic genes per patient, and it is often difficult to determine which of these being of less interest. This goes some way to explaining why, variants underlies disease in a given individual. However, at the despite the abundance of NGS data, the discovery of disease- population level, there may be some degree of phenotypic homo- causing alleles from such data remains somewhat limited. geneity, with alterations of specific physiological pathways under- We developed the human gene connectome (HGC) to over- come this problem. -

NEDD9 Depletion Leads to MMP14 Inactivation by TIMP2 and Prevents Invasion and Metastasis
Published OnlineFirst November 7, 2013; DOI: 10.1158/1541-7786.MCR-13-0300 Molecular Cancer Cell Death and Survival Research NEDD9 Depletion Leads to MMP14 Inactivation by TIMP2 and Prevents Invasion and Metastasis Sarah L. McLaughlin1, Ryan J. Ice1, Anuradha Rajulapati1, Polina Y. Kozyulina2, Ryan H. Livengood5, Varvara K. Kozyreva1, Yuriy V. Loskutov1, Mark V. Culp4, Scott A. Weed1,3, Alexey V. Ivanov1,2 and Elena N. Pugacheva1,2 Abstract The scaffolding protein NEDD9 is an established prometastatic marker in several cancers. Nevertheless, the molecular mechanisms of NEDD9-drivenmetastasisincancersremainill-defined. Here, using a compre- hensive breast cancer tissue microarray, it was shown that increased levels of NEDD9 protein significantly correlated with the transition from carcinoma in situ to invasive carcinoma. Similarly, it was shown that NEDD9 overexpression is a hallmark of highly invasive breast cancer cells. Moreover, NEDD9 expression is crucial for the protease-dependent mesenchymal invasion of cancer cells at the primary site but not at the metastatic site. Depletion of NEDD9 is sufficient to suppress invasion of tumor cells in vitro and in vivo, leading to decreased circulating tumor cells and lung metastases in xenograft models. Mechanistically, NEDD9 localized to invasive pseudopods and was required for local matrix degradation. Depletion of NEDD9 impaired invasion of cancer cells through inactivation of membrane-bound matrix metalloproteinase MMP14 by excess TIMP2 on the cell surface. Inactivation of MMP14 is accompanied by reduced collagenolytic activity of soluble metalloproteinases MMP2 and MMP9. Reexpression of NEDD9 is sufficient to restore the activity of MMP14 and the invasive properties of breast cancer cells in vitro and in vivo. -

Rabbit Anti-Phospho-BCAR1-SL12575R
SunLong Biotech Co.,LTD Tel: 0086-571- 56623320 Fax:0086-571- 56623318 E-mail:[email protected] www.sunlongbiotech.com Rabbit Anti-phospho-BCAR1 SL12575R-FITC Product Name: Anti-phospho-BCAR1 (Tyr751)/FITC Chinese Name: FITC标记的磷酸化乳腺癌抗雌激素耐药蛋白1抗体 BCAR1 (phospho Y751); BCAR1(phospho Y751); p-BCAR1(p-Tyr751); Breast cancer anti estrogen resistance 1 protein; BCAR 1; Bcar1; BCAR1_HUMAN; Breast cancer Alias: anti estrogen resistance 1; Breast cancer anti-estrogen resistance protein 1; CAS; Cas scaffolding protein family member 1; Crk associated substrate; Crk associated substrate p130Cas; CRK-associated substrate; CRKAS; P130CAS. Organism Species: Rabbit Clonality: Polyclonal React Species: Human,Mouse,Rat, ICC=1:50-200IF=1:50-200 Applications: not yet tested in other applications. optimal dilutions/concentrations should be determined by the end user. Molecular weight: 93kDa Cellular localization: The cell membrane Form: Lyophilized or Liquid Concentration: 1mg/mlwww.sunlongbiotech.com KLH conjugated synthesised phosphopeptide derived from human BCAR1 around the immunogen: phosphorylation site of Tyr751 Lsotype: IgG Purification: affinity purified by Protein A Storage Buffer: 0.01M TBS(pH7.4) with 1% BSA, 0.03% Proclin300 and 50% Glycerol. Store at -20 °C for one year. Avoid repeated freeze/thaw cycles. The lyophilized antibody is stable at room temperature for at least one month and for greater than a year Storage: when kept at -20°C. When reconstituted in sterile pH 7.4 0.01M PBS or diluent of antibody the antibody is stable for at least two weeks at 2-4 °C. background: Product Detail: p130 represents one of several known substrates for v-Crk encoded p47. p130 Cas (for Crk-associated substrate) exhibits a high level of tyrosine phosphorylation and is tightly associated with v-Crk, suggesting a role in v-Crk-mediated cell signaling. -

Carlos Souza Do Nascimento
CARLOS SOUZA DO NASCIMENTO EXPRESSÃO GÊNICA EM BIBLIOTECAS DE cDNA DE PELE DE BOVINOS F2 (HOLANDÊS × GIR) INFESTADOS COM O CARRAPATO RIPHICEPHALUS (BOOPHILUS) MICROPLUS Tese apresentada à Universidade Federal de Viçosa, como parte das exigências do Programa de Pós- Graduação em Zootecnia, para obtenção do título de Doctor Scientiae. VIÇOSA MINAS GERAIS - BRASIL 2009 CARLOS SOUZA DO NASCIMENTO EXPRESSÃO GÊNICAEM BIBLIOTECAS DE cDNA DE PELE DE BOVINOS F2 (HOLANDÊS x GIR) INFESTEDOS COM O CARRAPATO RIPHICEPHALUS (BOOPHILUS) MICROPLUS Tese apresentada à Universidade Federal de Viçosa, como parte das exigências do Programa de Pós- Graduação em Zootecnia, para obtenção do título de Doctor Scientiae. APROVADA: 19 de fevereiro de 2009. Dr. Marco Antonio Machado Dra. Marta Fonseca Martins (Co-Orientador) Guimarães Prof. Jose Bracini Neto Prof. Paulo Luiz Souza Carneiro Profª. Simone E. F. Guimarães (Orientadora) Para ser grande, sê inteiro: nada Teu exagera ou exclui. Sê todo em cada coisa. Põe quanto és No mínimo que fazes. Assim em cada coisa a Lua toda Brilha, porque alta vive. Ricardo Reis (heterônimo de Fernando Pessoa) ii AGRADECIMENTOS Agradeço a todos que, de forma direta ou indireta, estiveram presentes durante essa longa caminhada. À Universidade Federal de Viçosa (UFV) e ao Departamento de Zootecnia (DZO), pela oportunidade de realização do curso. Ao Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), pela concessão da bolsa de estudos. À Embrapa Gado de Leite (Juiz de fora, Minas Gerais), pela imprescindível contribuição na realização deste trabalho. Agradeço à minha orientadora, Profa. Simone E.F. Guimarães, pela oportunidade de aprendizado e pela confiança demonstrada na realização desta pesquisa. -
Phosphotyrosine Profiling of Curcumin-Induced Signaling
Sathe et al. Clin Proteom (2016) 13:13 DOI 10.1186/s12014-016-9114-0 Clinical Proteomics RESEARCH Open Access Phosphotyrosine profiling of curcumin‑induced signaling Gajanan Sathe1,2†, Sneha M. Pinto1,3†, Nazia Syed1,4, Vishalakshi Nanjappa1,5, Hitendra S. Solanki1,6, Santosh Renuse1,5, Sandip Chavan1,2, Aafaque Ahmad Khan1,6, Arun H. Patil1,6, Raja Sekhar Nirujogi1,7, Bipin Nair5, Premendu Prakash Mathur6, T. S. Keshava Prasad1,3,8, Harsha Gowda1,3* and Aditi Chatterjee1,3* Abstract Background: Curcumin, derived from the rhizome Curcuma longa, is a natural anti-cancer agent and has been shown to inhibit proliferation and survival of tumor cells. Although the anti-cancer effects of curcumin are well estab- lished, detailed understanding of the signaling pathways altered by curcumin is still lacking. In this study, we carried out SILAC-based quantitative proteomic analysis of a HNSCC cell line (CAL 27) to investigate tyrosine signaling in response to curcumin. Results: Using high resolution Orbitrap Fusion Tribrid Fourier transform mass spectrometer, we identified 627 phos- photyrosine sites mapping to 359 proteins. We observed alterations in the level of phosphorylation of 304 sites cor- responding to 197 proteins upon curcumin treatment. We report here for the first time, curcumin-induced alterations in the phosphorylation of several kinases including TNK2, FRK, AXL, MAPK12 and phosphatases such as PTPN6, PTPRK, and INPPL1 among others. Pathway analysis revealed that the proteins differentially phosphorylated in response to curcumin are known to be involved in focal adhesion kinase signaling and actin cytoskeleton reorganization. Conclusions: The study indicates that curcumin may regulate cellular processes such as proliferation and migration through perturbation of the focal adhesion kinase pathway. -

Significance of Serum Neural Precursor Cell‑Expressed Developmentally Downregulated Protein 9 in Melanoma
204 MOLECULAR AND CLINICAL ONCOLOGY 8: 204-208, 2018 Significance of serum neural precursor cell‑expressed developmentally downregulated protein 9 in melanoma KAYHAN ERTURK, FARUK TAS, MURAT SERILMEZ, ELIF BILGIN and DERYA DURANYILDIZ Department of Medical Oncology, Institute of Oncology, University of Istanbul, Istanbul 34093, Turkey Received July 26, 2017; Accepted October 27, 2017 DOI: 10.3892/mco.2017.1493 Abstract. Neural precursor cell-expressed developmentally with other non-malignant conditions, including polycystic downregulated protein 9 (NEDD9) is a promoter for various kidney disease (7). cellular functions that result in tumorigenesis. The aim of Neural precursor cell-expressed developmentally downreg- the present study was to analyse the serum levels of NEDD9 ulated protein (NEDD9) interacts with novel SH2-containing in melanoma patients in order to evaluate its prognostic, protein family scaffold proteins and the adaptor proteins predictive and diagnostic value. Data from 112 melanoma SHC and GRB2 via its C-terminal domain, and mediates patients were retrospectively analyzed and ELISA assays the communication between receptor tyrosine kinases and were used to measure serum NEDD9 concentration. The integrins, so that receptors, such as T-cell, B-cell and integrin median serum NEDD9 levels of the patients were significantly receptors, send upstream activation signals. Subsequently, higher compared with those of the controls. Serum NEDD9 focal adhesion kinase (FAK) and the Src and ABL families of was not found to be associated with any of the clinicopatho- kinases are activated and they, in turn, phosphorylate NEDD9 logical parameters, and was also not found to be prognostic substrate domain even more extensively, which provides for survival in melanoma.