207620Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pediatric Suprasellar Germ Cell Tumors: a Clinical and Radiographic Review of Solitary Vs
cancers Article Pediatric Suprasellar Germ Cell Tumors: A Clinical and Radiographic Review of Solitary vs. Bifocal Tumors and Its Therapeutic Implications Darian R. Esfahani 1 , Tord Alden 1,2, Arthur DiPatri 1,2, Guifa Xi 1,2, Stewart Goldman 3 and Tadanori Tomita 1,2,* 1 Division of Pediatric Neurosurgery, Ann & Robert H. Lurie Children’s Hospital, Chicago, IL 60611, USA; [email protected] (D.R.E.); [email protected] (T.A.); [email protected] (A.D.); [email protected] (G.X.) 2 Department of Neurosurgery, Northwestern University Feinberg School of Medicine, Chicago, IL 60611, USA 3 Division of Hematology, Oncology, Neuro-Oncology & Stem Cell Transplantation, Ann & Robert H. Lurie Children’s Hospital, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-312-2274220 Received: 7 August 2020; Accepted: 10 September 2020; Published: 14 September 2020 Simple Summary: Bifocal suprasellar germ cell tumors are a unique type of an uncommon brain tumor in children. Compared to other germ cell tumors in the brain, bifocal tumors are poorly understood and have a bad prognosis. In this paper we explore features that predict which children will have good outcomes and which will not. This is important for the research community because it can help physicians decide what type of radiation treatment is best to treat these children. Our study shows that bifocal tumors have a unique appearance on magnetic resonance imaging (MRI) compared to other germ cell tumors. Children with bifocal tumors are more likely to be male, have tumors that come back sooner, and cause death sooner. -

Drug Class Review Antianginal Agents
Drug Class Review Antianginal Agents 24:12.08 Nitrates and Nitrites 24:04.92 Cardiac Drugs, Miscellaneous Amyl Nitrite Isosorbide Dinitrate (IsoDitrate ER®, others) Isosorbide Mononitrate (Imdur®) Nitroglycerin (Minitran®, Nitrostat®, others) Ranolazine (Ranexa®) Final Report May 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Antianginal Therapies .............................................................................................. 4 Table 2. Summary of Agents .................................................................................................. 5 Disease Overview ........................................................................................................................ 8 Table 3. Summary of Current Clinical Practice Guidelines .................................................... 9 Pharmacology ............................................................................................................................... 10 Table 4. Pharmacokinetic Properties -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Hospital Medical School.)
THE CONTROL OF THE SUPRARENAL GLANDS BY THE SPLANCHNIC NERVES'. BY T. R. ELLIOTT, M.D. (From the Research Laboratories of University College, Hospital Medical School.) THERE is no clear knowledge2 at present with regard to the share taken by the suprarenal glands in resisting various processes that are harmful to the body. For the last two years I have tried to gain some light on this question by analysing the state of exhaustion to which the human suprarenals are reduced in the different conditions leading to death in Hospital cases. Attention was paid chiefly to the loss of the normal load of cortical " lipoid " substance and of the adrenalin in the medulla, the gross total of the latter being measured quantitatively by physio- logical assay. Unfortunately the conditions of fatal disease in man were found to be too complex to permit of simple atialysis. Broadly summarising the results, it appeared that the glands suffered rapid eyhaustion in cases of any microbic fever, of repeated simple hawmorrhage, and of surgical shock: but to distinguish clearly the value and nature of each of these factors was impossible. I therefore tried to reproduce each separately on experimental animals, in which the relationship of the nervous system to the glands could at the same time be studied. Method. Cats were used in all the experiments. The lipoid in the cortex of the cat3 is never so abundant as in the human gland: changes in its distribution were observed histologically, but they did not seem to follow any special cause, and they will be referred to only incidentally in this paper. -

Case Reports
CASE REPORTS NONCHROMAFFIN PARAGANGLIOMA OF THE JUGULAR FORAMEN Jos~ G. ALBERNAZ,M.D.,* A:N'D PAUL C. BucY, M.D. Chicago Memorial Hospital and Department of Neurology and Neurological Surgery, University of Illinois, College of Medicine, Chicago, Illinois (Received for publication April 7, 1953) This paper deals with a carotid-body-like tumor found in the jugular foramen, similar to the tumors recently described by Lattes 12 as nouchromaffin paraganglio- mas. Kohn, 1~ in 1900, classified the carotid body as a paraganglion, in the belief that it was of sympathetic origin and part of the chromaffin system. Small masses of similar paraganglionic tissue have since been described in the following locations: 1) At the level of the middle ear. As early as 1840, Valentin 26 described a gangliolum tympanicum, associated with the tympanic branch of the 9th cranial nerve. Later, in 1879, Krause H showed that this structure resembles the carotid body and this has been confirmed recently by the studies of Guild s and Lattes and WaltnerY In addi- tion to the paraganglion tympanicum, Guild s described what he called the glomus jugularis "in the adventitia of the dome of the jugular bulb, immediately below the bony floor of the middle ear." ~) At the aortic-pulmonary region. Paraganglia related to the major vessels at the base of the heart were mentioned in 190~ by Biedl and Wiesel. 2 In the middle thirties, Palme, 2~ Seto, 24 Muratori ~9 and Nonidez 2~ described these structures in detail. From their contributions, well summarized by Boyd, 4 we learn that these "aortic bodies" are similar to the carotid bodies and that they can be found in four different locations: a) above the ductus arteriosus; b) on the trunk of the pulmonary artery, near the origin of the left coronary artery; c) near the root of the innominate artery; d) on the left part of the aortic arch. -

Clinical Radiation Oncology Review
Clinical Radiation Oncology Review Daniel M. Trifiletti University of Virginia Disclaimer: The following is meant to serve as a brief review of information in preparation for board examinations in Radiation Oncology and allow for an open-access, printable, updatable resource for trainees. Recommendations are briefly summarized, vary by institution, and there may be errors. NCCN guidelines are taken from 2014 and may be out-dated. This should be taken into consideration when reading. 1 Table of Contents 1) Pediatrics 6) Gastrointestinal a) Rhabdomyosarcoma a) Esophageal Cancer b) Ewings Sarcoma b) Gastric Cancer c) Wilms Tumor c) Pancreatic Cancer d) Neuroblastoma d) Hepatocellular Carcinoma e) Retinoblastoma e) Colorectal cancer f) Medulloblastoma f) Anal Cancer g) Epndymoma h) Germ cell, Non-Germ cell tumors, Pineal tumors 7) Genitourinary i) Craniopharyngioma a) Prostate Cancer j) Brainstem Glioma i) Low Risk Prostate Cancer & Brachytherapy ii) Intermediate/High Risk Prostate Cancer 2) Central Nervous System iii) Adjuvant/Salvage & Metastatic Prostate Cancer a) Low Grade Glioma b) Bladder Cancer b) High Grade Glioma c) Renal Cell Cancer c) Primary CNS lymphoma d) Urethral Cancer d) Meningioma e) Testicular Cancer e) Pituitary Tumor f) Penile Cancer 3) Head and Neck 8) Gynecologic a) Ocular Melanoma a) Cervical Cancer b) Nasopharyngeal Cancer b) Endometrial Cancer c) Paranasal Sinus Cancer c) Uterine Sarcoma d) Oral Cavity Cancer d) Vulvar Cancer e) Oropharyngeal Cancer e) Vaginal Cancer f) Salivary Gland Cancer f) Ovarian Cancer & Fallopian -

The Diagnosis and Pathological Value of Combined Detection of HE4 and CA125 for Patients with Ovarian Cancer
Open Med. 2016; 11:125-132 Research Article Open Access Li-e Zheng*, Jun-ying Qu, Fei He The diagnosis and pathological value of combined detection of HE4 and CA125 for patients with ovarian cancer DOI 10.1515/med-2016-0024 other. Conclusion HE4 can be used as a novel clinical bio- received January 28, 2016; accepted March 9, 2016 marker for predicting malignant ovarian tumors and its expression was closely related with the clinical pathologi- Abstract: Objective To evaluate the value of individual and cal features of malignant ovarian tumors. combined measurement of human epididymis protein 4 (HE4) and cancer antigen 125 (CA-125) in the diagnosis Keywords: HE4; CA125; diagnosis; ovarian tumor of ovarian cancer. Methods A clinical case-control study was performed in which the levels of serum HE4 and CA-125 of subjects with malignant, borderline, benign ovarian tumors and healthy women were measured before 1 Introduction surgery. An immunohistochemistry method was used In the female reproductive system, ovarian cancer ranks to measure the expression of HE4 in different tissues. third in incidence and 1st in mortality in gynecological Statistical analysis was performed to determine the rela- malignancies [1]. Nearly 70% of patients with ovarian tionship between the level of HE4 and the pathologic cancer are diagnosed at an advanced stage, and the 5 year type as well as the stage of the ovarian tumors. Results survival rate for patients with ovarian cancer rises up to The level of HE4 in the serum was significantly elevated in 90% through early effective treatment [2]. Hence, diag- the malignant ovarian cancer group compared with other nosing at early stage is crucial to improve the prognosis of groups. -
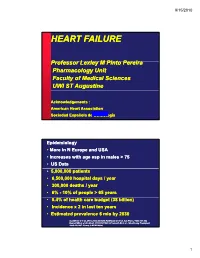
Heart Failure
9/15/2010 HEART FAILURE PfProfessor LlLexley M MPitP Pinto Perei ra Pharmacology Unit Faculty of Medical Sciences UWI ST Augustine Acknowledgements : American Heart Association Sociedad Española de CardiologíaJune, 1999 Epidemiology • More in N Europe and USA • Increases with age esp in males > 75 • US Data • 5,000,000 patients • 6,500,000 hospital days/ year • 300,000 deaths / year • 6% --10%10% of people > 65 years • 5.4%f% of health care budget (38 billion) • Incidence x 2 in last ten years • Estimated prevalence 6 mio by 2030 Gottdiener J et al. JACC 2000;35:1628, Haldeman GA et al. Am Heart J 1999;137:352 Kannel WB et al. Am Heart J 1991;121:951, O’Connell JB et al. J Heart Lung Transplant 1993;13:S107, Young J, MCNA 2004; 1 9/15/2010 Definition of heart failure Clinical syyyndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood AHA / ACC HF guidelines 2001 Clinical symptoms / signs secondary to abnormal ventricular function ESC HF guidelines 2001 “Heart Failure” vs. “Congestive Heart Failure” All patients may NOT have volume overload at the time of initial or subsequent evaluation. Therefore the term “heart failure” is preferred over the older term “ihfil”“congestive heart failure.” CHF is a significant cause of morbidity and mortality Important cause of hospitalizations among elderly 2 9/15/2010 Causes of HF For a substantial proportion of patients, the causes of HF are: 1. Coronary artery disease 2. Hypertension 3. Dilated cardiomyopathy And there are other causes 1. -

A Xenograft and Cell Line Model of SDH-Deficient Pheochromocytoma Derived from Sdhb+/− Rats
27 6 Endocrine-Related J F Powers et al. Rat model for Sdhb-mutated 27:6 337–354 Cancer paraganglioma RESEARCH A xenograft and cell line model of SDH-deficient pheochromocytoma derived from Sdhb+/− rats James F Powers1, Brent Cochran2, James D Baleja2, Hadley D Sikes3, Andrew D Pattison4, Xue Zhang2, Inna Lomakin1, Annette Shepard-Barry1, Karel Pacak5, Sun Jin Moon3, Troy F Langford3, Kassi Taylor Stein3, Richard W Tothill4,6, Yingbin Ouyang7 and Arthur S Tischler1 1Department of Pathology and Laboratory Medicine, Tufts Medical Center, Tufts University School of Medicine, Boston, Massachusetts, USA 2Department of Developmental, Molecular and Chemical Biology, Tufts University School of Medicine, Boston, Massachusetts, USA 3Department of Chemical Engineering, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA 4Department of Clinical Pathology, University of Melbourne, Melbourne, Victoria, Australia 5Section on Medical Neuroendocrinology, Eunice Kennedy Shriver Division National Institute of Child Health and Human Development, Bethesda, Maryland, USA 6Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia 7Cyagen US Inc, Santa Clara, California, USA Correspondence should be addressed to J F Powers: [email protected] Abstract Tumors caused by loss-of-function mutations in genes encoding TCA cycle enzymes Key Words have been recently discovered and are now of great interest. Mutations in succinate f succinate dehydrogenase B dehydrogenase (SDH) subunits cause pheochromocytoma/paraganglioma (PCPG) and f paraganglioma syndromically associated tumors, which differ phenotypically and clinically from more f pheochromocytoma common SDH-intact tumors of the same types. Consequences of SDH deficiency include f cluster 1 rewired metabolism, pseudohypoxic signaling and altered redox balance. PCPG with f xenograft SDHB mutations are particularly aggressive, and development of treatments has been f cell culture hampered by lack of valid experimental models. -

Opmaak 1 15/06/12 08:52 Pagina 124
arain-_Opmaak 1 15/06/12 08:52 Pagina 124 JBR–BTR, 2012, 95: 124-125. PARAGANGLIOMA OF THE CAVERNOUS SINUS A. Arain, J. Vandevenne, B. Depeuter, J. Smits, F. Weyns, Y. Palmers 1 Key-word: Paraganglioma Background : A 15-year-old girl presented in a Dutch hospital with right-sided trigeminal neuralgia. MR-imaging showed a mass lesion in the right cavernous sinus. Differential diagnosis in this hospital was a meningioma or a schwannoma. The patient was referred to the neurosurgery department of our hospital, and resection of the lesion was planned. At surgery, the lesion pre - sented as a subdural bulge surrounded by swollen venous structures. The incision of the dura resulted in profuse hemorrhage of arterial origin, and hemostasis was obtained with difficulty. The tumor showed a fibrillar structure and a strong arterial vascularization which was not con - cordant with schwannoma. No further exploration of the lesion was performed, and no biopsy was obtained. To clarify the unexpected surgical findings and to reach a diagnosis without biopsy , pre-operative MR-images were reviewed. Digital subtraction angio graphy (DSA) was performed postoperatively. The lesion did not take up FDG on PET scan. Laboratory results showed increased catecholamines in the urine. AB CD E 1A 1B Fig. 1C 1D 1. Department of Medical Imaging, Campus Sint-Jan, Ziekenhuis Oost-Limburg, Genk, Belgium. 1E 2 arain-_Opmaak 1 15/06/12 08:52 Pagina 125 PARAGANGLIOMA OF THE CAVERNOUS SINUS — ARAIN et al 125 Work-up ly show a hyperintense signal on T2-weighted MR- images and a distinct contrast enhancement on T1- MRI of the brain (Fig. -

Genitourinary Advanced Pca and Its Efficacy As a Therapeutic Agent Is Presently Being Studied in Clinical Trials
ANNUAL MEETING ABSTRACTS 133A because they were over age 80 and as such, the IHC results were likely due to acquired 599 Anterior Predominant Prostate Tumors: A Contemporary methylation of the MLH1 promoter. The remaining 4 patients with absent staining have Look at Zone of Origin been referred to Cancer Genetics for possible further work-up. The reimbursement rate HA Al-Ahmadie, SK Tickoo, A Gopalan, S Olgac, VE Reuter, SW Fine. Memorial Sloan and turn-around time for the IHC stains were similar to that for other IHC stains used Kettering Cancer Center, NY, NY. in clinical practice. Background: Aggressive PSA screening and prostate needle biopsy protocols have Conclusions: IHC stains for the MMR proteins are fast and relatively easy to institute in successfully detected low-volume posterior tumors, with a concurrent increase in routine evaluation of CRC, and we have not had difficulty interpreting the stains leading anterior-predominant prostate cancer (AT). Zone of origin, patterns of spread, and to additional testing. Furthermore, reimbursement was obtained at a level similar to extraprostatic extension of these tumors have not been well studied. other IHC stains used in clinical practice. The surgeons and oncologists welcomed the Design: We greatly expanded and refined our previous studies to include pathologic prognostic information. Further study is warranted to confirm these initial findings. features of 197 patients with largest tumors anterior to the urethra in whole-mounted radical prostatectomy specimens. 597 High Fidelity Image Cytometry in Neoplastic Lesions in Barrett’s Results: Of 197 AT, 97 (49.2%) were predominantly located in the peripheral zone Esophagus, Including Basal Crypt Dysplasia-Like Atypia with Surface (PZ-D), 70 (35.5%) in the transition zone (TZ-D), 16 (8.1%) were of indeterminate Maturation zone (IND), and 14 (7.1%) in both PZ and TZ (PZ+TZ). -

In February 2013, Glaxosmithkline (GSK) Announced a Commitment To
In February 2013, GlaxoSmithKline (GSK) announced a commitment to further clinical transparency through the public disclosure of GSK Clinical Study Reports (CSRs) on the GSK Clinical Study Register. The following guiding principles have been applied to the disclosure: Information will be excluded in order to protect the privacy of patients and all named persons associated with the study Patient data listings will be completely removed* to protect patient privacy. Anonymized data from each patient may be made available subject to an approved research proposal. For further information please see the Patient Level Data section of the GSK Clincal Study Register. Aggregate data will be included; with any direct reference to individual patients excluded *Complete removal of patient data listings may mean that page numbers are no longer consecutively numbered CONFIDENTIAL GM2004/00056/00GM2004/00056/00 SAM40040SAM40040 The GlaxoSmithKline group of companies A twenty-four week, randomised, double-dummy, double-blind, parallel group study to compare the occurrence of exacerbations between SERETIDE DISKUS 50/250µg 1 inhalation bd and formoterol/budesonide Breath-Actuated Dry Powder Inhaler 4.5/160µg 2 inhalations bd in subjects with moderate to severe asthma. Clinical Study Report for Study SAM40040 (Development Phase IV) Document Number: GM2004/00056/00 Compound Number: CCI18781/ GR33343 Investigational Product: SERETIDE Generic Drug Name: salmeterol/fluticasone propionate combination Indication Studied: Asthma Initiation Date: 26 Nov 2001 Completion Date: 13 Jan 2003 Early Termination Date: N/A Date of Report: August 2004 Sponsor Signatory: (and Medical Officer) Vice President European Clinical Respiratory Medicines Development Centre This study was performed in compliance with Good Clinical Practices including the archiving of essential documents.