An Emerging Role for the Unfolded Protein Response in Pancreatic Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Potent and Selective Inhibitor of Cdc42 Gtpase Zurab Surviladze University of New Mexico
Cedarville University DigitalCommons@Cedarville Pharmacy Faculty Publications School of Pharmacy 2010 A Potent and Selective Inhibitor of Cdc42 GTPase Zurab Surviladze University of New Mexico Anna Waller University of New Mexico J. Jacob Strouse University of New Mexico Cristian G. Bologa University of New Mexico Oleg Ursu University of New Mexico See next page for additional authors Follow this and additional works at: http://digitalcommons.cedarville.edu/pharmacy_publications Part of the Medicinal and Pharmaceutical Chemistry Commons Recommended Citation 2010: Surviladze, Z., Waller A., Strouse, J., Bologa, C., & Ursu, O., A Potent and Selective Inhibitor of Cdc42 GTPase, submitted to National Institutes of Health. This Web Publication is brought to you for free and open access by DigitalCommons@Cedarville, a service of the Centennial Library. It has been accepted for inclusion in Pharmacy Faculty Publications by an authorized administrator of DigitalCommons@Cedarville. For more information, please contact [email protected]. Authors Zurab Surviladze, Anna Waller, J. Jacob Strouse, Cristian G. Bologa, Oleg Ursu, Virginia M. Salas, Genevieve K. Phillips, John F. Parkinson, Elsa Romero, Angela Wandinger-Ness, Larry A. Sklar, Chad E. Schroeder, Denise S. Simpson, Julica Nöth, Jenna Wang, Jennifer E. Golden, and Jeffrey Aubé This web publication is available at DigitalCommons@Cedarville: http://digitalcommons.cedarville.edu/pharmacy_publications/19 Probe Report Title: A Potent and Selective Inhibitor of Cdc42 GTPase Authors: UNM Center for Molecular Discovery: Zurab Surviladze, Anna Waller, J. Jacob Strouse, Cristian Bologa, Oleg Ursu, Virginia Salas, John F. Parkinson, Genevieve K. Phillips, Elsa Romero, Angela Wandinger-Ness and Larry A. Sklar. Kansas University Specialized Chemistry Center: Chad Schroeder, Denise Simpson, Julica Nöth, Jenna Wang, Jennifer Golden, and Jeffrey Aubé. -

Brefeldin A, a Cytotoxin Produced by Paecilomyces Sp. and Aspergillus Clavatus Isolated from Taxus Mairei and Torreya Grandis
FEMS Immunology and Medical Microbiology 34 (2002) 51^57 www.fems-microbiology.org Brefeldin A, a cytotoxin produced by Paecilomyces sp. and Aspergillus clavatus isolated from Taxus mairei and Torreya grandis Jianfeng Wang a;b;Ã, Yaojian Huang a, Meijuan Fang b, Yongjie Zhang a, Zhonghui Zheng a, Yufen Zhao b, Wenjin Su a;c a The Key Laboratory of Ministry of Education for Cell Biology and Tumor Cell Engineering, School of Life Sciences, Xiamen University, P.O. Box 958, Xiamen 361005, PR China b Bioorganic Phosphorus Chemistry Lab., Department of Chemistry, Xiamen University, Xiamen 361005, PR China c School of Biotechnology, Jimei University, Xiamen 361021, PR China Received 24 April 2002; received in revised form 29 May 2002; accepted 30 May 2002 First published online 3 August 2002 Abstract Paecilomyces sp. and Aspergillus clavatus, which were isolated from Taxus mairei and Torreya grandis from southeast China, produced toxic metabolites when grown in liquid culture. Nuclear magnetic resonance techniques, infrared spectrometry, electrospray ionization mass spectroscopy and X-ray analysis identified brefeldin A, a bioactive metabolite produced by a number of fungal species belonging to the genera Alternaria, Ascochyta, Penicillium, Curvularia, Cercospora and Phyllosticta. This is the first report of the isolation of the cytotoxin from Paecilomyces sp. and A. clavatus. The relevance of brefeldin A to the association between these fungi and their host plants is discussed. ß 2002 Federation of European Microbiological Societies. Published by Elsevier Science B.V. All rights reserved. Keywords: Brefeldin A; Endophytic fungi; Paecilomyces sp.; Aspergillus clavatus; Taxus mairei; Torreya grandis 1. Introduction showed antitumor and antifungal activity, respectively, demonstrating that endophytic fungi are to be a promising Fungi are fundamental to the health and prosperity of source of bene¢cial bioactive products [5]. -

Brefeldin a | CAS 20350-15-6 | GEF Inhibitor
Produktinformation Diagnostik & molekulare Diagnostik Laborgeräte & Service Zellkultur & Verbrauchsmaterial Forschungsprodukte & Biochemikalien Weitere Information auf den folgenden Seiten! See the following pages for more information! Lieferung & Zahlungsart Lieferung: frei Haus Bestellung auf Rechnung SZABO-SCANDIC Lieferung: € 10,- HandelsgmbH & Co KG Erstbestellung Vorauskassa Quellenstraße 110, A-1100 Wien T. +43(0)1 489 3961-0 Zuschläge F. +43(0)1 489 3961-7 [email protected] • Mindermengenzuschlag www.szabo-scandic.com • Trockeneiszuschlag • Gefahrgutzuschlag linkedin.com/company/szaboscandic • Expressversand facebook.com/szaboscandic Brefeldin A GEF inhibitor Catalog No. SIH-225 Discovery through partnership | Excellence through quality Overview Product Name Brefeldin A Description GEF inhibitor Purity >98% CAS No. 20350-15-6 Molecular Formula C H O Molecular Weight 280.36 Properties Storage Temperature -20ºC Shipping Temperature Shipped Ambient Product Type Inhibitor Solubility Soluble to 10 mM in ethanol and to 50 mM in DMSO Source Synthetic Appearance White Crystalline Solid SMILES C[C@H]1CCC/C=C/[C@@H]2C[C@@H](C[C@H]2[C@@H](/C=C/C(=O)O1)O)O InChI InChI=1S/C16H24O4/c1-11-5-3-2-4-6-12-9-13(17)10-14(12)15(18)7-8-16(19)20-11/h4,6-8,11-15,17-18H,2-3,5,9-10H2,1H3/b6-4+, InChIKey KQNZDYYTLMIZCT-PNFJWZTBSA-N Safety Phrases Classification: Harmful. May be harmful if inhaled, swallowed or absorbed through skin. Safety Phrases: S22 - Do not breathe dust S24/25 - Avoid contact with skin and eyes S36/37/39 - Wear suitable protective clothing, gloves and eye/face protection Risk Phrases: R68- Possible risk of irreversible effects Hazard Phrases: H301 Precautionary Phrases: P301 + P310 Cite This Product Brefeldin A (StressMarq Biosciences Inc., Victoria BC CANADA, Catalog # SIH-225) Biological Description Alternative Names Cyanaein Research Areas Cancer, Apoptosis PubChem ID 5287620 Scientific Background Brefeldin A is a reversible inhibitor of proteins from the endoplasmic reticulum (ER) to the golgi. -

Unfolded Protein Response and Cell Death After Depletion of Brefeldin A-Inhibited Guanine Nucleotide-Exchange Protein GBF1
Unfolded protein response and cell death after depletion of brefeldin A-inhibited guanine nucleotide-exchange protein GBF1 Carmen Citterio*, Alessandro Vichi*, Gustavo Pacheco-Rodriguez*, Angel M. Aponte†, Joel Moss*, and Martha Vaughan*‡ *Translational Medicine Branch and †Proteomics Core Facility, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD 20892 Contributed by Martha Vaughan, December 31, 2007 (sent for review December 4, 2007) Guanine nucleotide-exchange factors (GEFs) activate ADP- with both class II ARFs. GBF1, which promoted COPI recruit- ribosylation factor (ARF) GTPases that recruit coat proteins to ment to membranes both in vitro and in vivo (12, 13), was membranes to initiate transport vesicle formation. Three mamma- dynamically associated with elements termed vesicular tubular lian GEFs are inhibited by brefeldin A (BFA). GBF1, predominantly clusters (VTCs) and cis-Golgi membranes (14, 15). The GBF1 associated with cis-Golgi membranes, functions early in the secre- molecule contains a dimerization motif, first identified in its tory pathway, whereas BIG1 and BIG2 act in trans-Golgi or later plant homolog GNOM (16), and likely exists as homodimer. sites. Perturbation of endoplasmic reticulum (ER) functions can GBF1 is the BFA-sensitive ARF GEF responsible for membrane result in accumulation of unfolded or misfolded proteins that association of COPI early in the secretory pathway (17), where causes ER stress and unfolded protein response (UPR), with accu- it is essential to the translocation of pre-Golgi intermediates and mulation of ER stress response element (ERSE) gene products. BFA the maintenance of Golgi integrity (18). treatment of cells causes accumulation of proteins in the ER, ER The complex system of ER membranes is the site of synthesis stress, and ultimately apoptosis. -
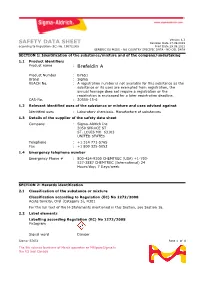
SAFETY DATA SHEET Revision Date 17.09.2019 According to Regulation (EC) No
Version 6.3 SAFETY DATA SHEET Revision Date 17.09.2019 according to Regulation (EC) No. 1907/2006 Print Date 29.09.2021 GENERIC EU MSDS - NO COUNTRY SPECIFIC DATA - NO OEL DATA SECTION 1: Identification of the substance/mixture and of the company/undertaking 1.1 Product identifiers Product name : Brefeldin A Product Number : B7651 Brand : Sigma REACH No. : A registration number is not available for this substance as the substance or its uses are exempted from registration, the annual tonnage does not require a registration or the registration is envisaged for a later registration deadline. CAS-No. : 20350-15-6 1.2 Relevant identified uses of the substance or mixture and uses advised against Identified uses : Laboratory chemicals, Manufacture of substances 1.3 Details of the supplier of the safety data sheet Company : Sigma-Aldrich Inc. 3050 SPRUCE ST ST. LOUIS MO 63103 UNITED STATES Telephone : +1 314 771-5765 Fax : +1 800 325-5052 1.4 Emergency telephone number Emergency Phone # : 800-424-9300 CHEMTREC (USA) +1-703- 527-3887 CHEMTREC (International) 24 Hours/day; 7 Days/week SECTION 2: Hazards identification 2.1 Classification of the substance or mixture Classification according to Regulation (EC) No 1272/2008 Acute toxicity, Oral (Category 3), H301 For the full text of the H-Statements mentioned in this Section, see Section 16. 2.2 Label elements Labelling according Regulation (EC) No 1272/2008 Pictogram Signal word Danger Sigma- B7651 Page 1 of 8 The life science business of Merck operates as MilliporeSigma in the US and Canada Hazard statement(s) H301 Toxic if swallowed. -

Sec22b Regulates Inflammatory Responses by Controlling The
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.20.305383; this version posted September 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Sec22b regulates in0lammatory responses by controlling the nuclear translocation of NF-κB Guillermo ARANGO DUQUE1‡, Renaud DION1‡, Aymeric FABIÉ1, Julien DESCOTEAUX1, Simona STÄGER1 and AlBert DESCOTEAUX1* 1 INRS – Centre Armand-Frappier Santé BiotecHnologie, Université du QuéBec, Laval, QC, H7V 1B7, Canada ‡ THese autHors Have contriButed eQually to tHis manuscript * Corresponding autHor: AlBert Descoteaux E-mail: [email protected] Running title: Sec22B mediates NF-κB translocation KeyworDs: Cytokine, intracellular trafZicking, nuclear translocation, soluBle NSF attacHment protein receptor (SNARE), NF-kappa B (NF-KB) 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.09.20.305383; this version posted September 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract secretory patHway, a dynamic group of organelles through which proteins and lipids Soluble NSF attachment receptor (SNARE) are synthesized, processed and transported proteins regulate the vesicle transport (3,4). WHile recycling/early endosomes and tHe machinery in phagocytic cells. Within the endoplasmic reticulum (ER) supply membrane secretory patHway, Sec22b is an ER-Golgi and protein effectors to nascent pHagosomes intermediate compartment (ERGIC)-resident (5,6), the latter also serve as cytokine secretion SNARE tHat controls pHagosome maturation sites (7). ThrougH sequential membrane and function in macropHages and dendritic excHanges witH organelles sucH as tHe cells. -

Cellular Response to Endoplasmic Reticulum Stress: a Matter of Life Or Death
Cell Death and Differentiation (2006) 13, 363–373 & 2006 Nature Publishing Group All rights reserved 1350-9047/06 $30.00 www.nature.com/cdd Review Cellular response to endoplasmic reticulum stress: a matter of life or death M Boyce1 and J Yuan*,1 therefore critical for numerous aspects of cell physiology, including vesicle trafficking, lipid and membrane biogenesis 1 Department of Cell Biology, Harvard Medical School, Boston, MA, USA and protein targeting and secretion. Accordingly, metazoan * Corresponding author: J Yuan, Department of Cell Biology, Harvard Medical cells react rapidly to ER dysfunction through a set of adaptive School, 240 Longwood Avenue, Boston, MA 02115, USA. pathways known collectively as the ER stress response Tel: þ 1 617 432 4170; Fax: þ 1 617 432 4177; (ESR).2–6 E-mail: [email protected] The ESR can be triggered by disparate perturbations in Received 01.8.05; revised 28.9.05; accepted 03.10.05; published online 06.1.06 normal ER function, such as the accumulation of unfolded, Edited by G Melino misfolded or excessive protein, ER lipid or glycolipid imbalances, or changes in the redox or ionic conditions of the ER lumen.2,3,5,6 In response to such dysfunction, the ESR Abstract acts both to increase the capacity of the ER to fold and The proper functioning of the endoplasmic reticulum (ER) is process client proteins, and to alleviate the burden on the critical for numerous aspects of cell physiology. Accordingly, organelle by reducing the amount of protein inside the ER. These effects are achieved through three major pathways: (I) all eukaryotes react rapidly to ER dysfunction through a set the unfolded protein response (UPR), a transcription-depen- of adaptive pathways known collectively as the ER stress dent induction of ER lumenal chaperone proteins and other response (ESR). -

Mammalian Erv46 Localizes to the Endoplasmic Reticulum–Golgi Intermediate Compartment and to Cis-Golgi Cisternae
Dartmouth College Dartmouth Digital Commons Dartmouth Scholarship Faculty Work 4-15-2003 Mammalian Erv46 Localizes to the Endoplasmic Reticulum–Golgi Intermediate Compartment and to Cis-Golgi Cisternae Lelio Orci University Hospitals Geneva Medical Center Mariella Ravazzola University Hospitals Geneva Medical Center Gary J. Mack Dartmouth College Charles Barlowe Dartmouth College Stefan Otte Dartmouth College Follow this and additional works at: https://digitalcommons.dartmouth.edu/facoa Part of the Medical Biochemistry Commons Dartmouth Digital Commons Citation Orci, Lelio; Ravazzola, Mariella; Mack, Gary J.; Barlowe, Charles; and Otte, Stefan, "Mammalian Erv46 Localizes to the Endoplasmic Reticulum–Golgi Intermediate Compartment and to Cis-Golgi Cisternae" (2003). Dartmouth Scholarship. 1401. https://digitalcommons.dartmouth.edu/facoa/1401 This Article is brought to you for free and open access by the Faculty Work at Dartmouth Digital Commons. It has been accepted for inclusion in Dartmouth Scholarship by an authorized administrator of Dartmouth Digital Commons. For more information, please contact [email protected]. Mammalian Erv46 localizes to the endoplasmic reticulum–Golgi intermediate compartment and to cis-Golgi cisternae Lelio Orci*, Mariella Ravazzola*, Gary J. Mack†, Charles Barlowe†‡, and Stefan Otte† *Department of Morphology, University Medical Center, 1211 Geneva 4, Switzerland; and †Department of Biochemistry, Dartmouth Medical School, Hanover, NH 03755 Communicated by William T. Wickner, Dartmouth Medical School, Hanover, NH, February 13, 2003 (received for review August 12, 2002) Yeast endoplasmic reticulum (ER) vesicle protein Erv46p is a novel growth but, when mutated, influence protein sorting and͞or membrane protein involved in transport through the early secre- transport in the early secretory pathway. tory pathway. Investigation of mammalian Erv46 (mErv46) reveals To date, the ultrastructural localization of only a few proteins that it is broadly expressed in tissues and protein-secreting cells. -

A Protumorigenic Secretory Pathway Activated by P53 Deficiency in Lung Adenocarcinoma
The Journal of Clinical Investigation RESEARCH ARTICLE A protumorigenic secretory pathway activated by p53 deficiency in lung adenocarcinoma Xiaochao Tan,1 Lei Shi,1 Priyam Banerjee,1 Xin Liu,1 Hou-Fu Guo,1 Jiang Yu,1 Neus Bota-Rabassedas,1 B. Leticia Rodriguez,1 Don L. Gibbons,1 William K. Russell,2 Chad J. Creighton,3,4 and Jonathan M. Kurie1 1Department of Thoracic/Head and Neck Medical Oncology, the University of Texas MD Anderson Cancer Center, Houston, Texas, USA. 2Department of Biochemistry and Molecular Biology, University of Texas Medical Branch, Galveston, Texas, USA. 3Department of Medicine, Dan L. Duncan Cancer Center, Baylor College of Medicine, Houston, Texas, USA. 4Department of Bioinformatics and Computational Biology, the University of Texas MD Anderson Cancer Center, Houston, Texas, USA. Therapeutic strategies designed to target TP53-deficient cancer cells remain elusive. Here, we showed that TP53 loss initiated a pharmacologically actionable secretory process that drove lung adenocarcinoma (LUAD) progression. Molecular, biochemical, and cell biological studies showed that TP53 loss increased the expression of Golgi reassembly and stacking protein 55 kDa (G55), a Golgi stacking protein that maintains Golgi organelle integrity and is part of a GOLGIN45 (G45)–myosin IIA–containing protein complex that activates secretory vesicle biogenesis in the Golgi. TP53 loss activated G55-dependent secretion by relieving G55 and myosin IIA from miR-34a–dependent silencing. G55-dependent secreted proteins enhanced the proliferative and invasive activities of TP53-deficient LUAD cells and promoted angiogenesis and CD8+ T cell exhaustion in the tumor microenvironment. A small molecule that blocks G55-G45 interactions impaired secretion and reduced TP53-deficient LUAD growth and metastasis. -

Brefeldin a (BFA)
Brefeldin A (BFA) sc-200861 Material Safety Data Sheet Hazard Alert Code EXTREME HIGH MODERATE LOW Key: Section 1 - CHEMICAL PRODUCT AND COMPANY IDENTIFICATION PRODUCT NAME Brefeldin A (BFA) STATEMENT OF HAZARDOUS NATURE CONSIDERED A HAZARDOUS SUBSTANCE ACCORDING TO OSHA 29 CFR 1910.1200. NFPA FLAMMABILITY1 HEALTH2 HAZARD INSTABILITY0 SUPPLIER Company: Santa Cruz Biotechnology, Inc. Address: 2145 Delaware Ave Santa Cruz, CA 95060 Telephone: 800.457.3801 or 831.457.3800 Emergency Tel: CHEMWATCH: From within the US and Canada: 877-715-9305 Emergency Tel: From outside the US and Canada: +800 2436 2255 (1-800-CHEMCALL) or call +613 9573 3112 PRODUCT USE Macrocyclic lactone which exhibits a wide range of antibiotic and antifungal properties. Fungal metabolite produced by Penicillium brefeldianum, P. decumbens, P. cyaneum. Reversibly blocks protein translocation from endoplasmic reticulum to the Golgi apparatus. SYNONYMS C16-H24-O4, "4H-cyclopent(F)oxacyclotridecin-4-one, ", "4H-cyclopent(F)oxacyclotridecin-4-one, ", "1, 6, 7, 8, 9, 11a-beta, 12, 13, 14, 14a-alpha-decahydro-1beta-13-alpha-", dihydroxy-6-beta-13-alpha-dihydroxy-6-beta-methyl-, "1, 6, 7, 8, 9, 11a- beta, 12, 13, 14, 14a-alpha-decahydro-1beta-13-alpha-", dihydroxy-6-beta-13-alpha-dihydroxy-6-beta-methyl-, asotoxin, c, cyanaein, decumbin, nectrolide, "gamma, 4-dihydroxy-2-(6-hydroxy-1-heptenyl)-4-cyclopentanecrotonic acid", "gamma, 4- dihydroxy-2-(6-hydroxy-1-heptenyl)-4-cyclopentanecrotonic acid", "lambda lactone", "macrolide antibiotic/ antifungal" Section 2 - HAZARDS IDENTIFICATION CANADIAN WHMIS SYMBOLS EMERGENCY OVERVIEW RISK Harmful if swallowed. POTENTIAL HEALTH EFFECTS ACUTE HEALTH EFFECTS SWALLOWED ■ Accidental ingestion of the material may be harmful; animal experiments indicate that ingestion of less than 150 gram may be fatal or may produce serious damage to the health of the individual. -

Differential Use of Endoplasmic Reticulum Membrane for Phagocytosis in J774 Macrophages
Differential use of endoplasmic reticulum membrane for phagocytosis in J774 macrophages Thalia Becker, Allen Volchuk*, and James E. Rothman† Department of Physiology and Cellular Biophysics, Russ Berrie Medical Science Pavilion, Columbia University, 1150 St. Nicholas Avenue, New York, NY 10032 Contributed by James E. Rothman, December 22, 2004 Sustained phagocytosis requires the continuous replacement of sion events with great specificity (13–16). However, in a rare cell-surface membrane from intracellular sources. Depending on apparent exception to the SNARE hypothesis, it was observed the nature of the engulfed particles, a variety of endocytic com- that the isolated ER-localized SNARE Sec22p (from yeast) partments have been demonstrated to contribute membranes could mediate fusion of liposomes by paring with isolated yeast needed for the formation of phagosomes. It has recently been plasma membrane target-SNAREs (Sso1p and Sec9p) (13). An reported that the endoplasmic reticulum (ER) can also fuse with the alternative interpretation would be that, rather than being an plasma membrane during phagocytosis [Gagnon, E., Duclos, S., artifact or an exception to the SNARE hypothesis, this unex- Rondeau, C., Chevet, E., Cameron, P. H., Steele-Mortimer, O., pected observation would be the basis for the prediction of a Paiement, J., Bergeron, J. J. & Desjardins, M. (2002) Cell 110, physiological transport pathway from ER to plasma membrane 119–131]. However, there is currently no known mechanistic basis in which Sec22 functions as the vesicle-SNARE. for this fusion process to occur. Here we report that direct ER– The present study demonstrates that, in Fc-receptor-mediated plasma membrane fusion during phagocytosis requires the ER phagocytosis, the ER resident SNARE protein ERS24 (the resident soluble N-ethylmaleimide-sensitive factor attachment mammalian equivalent to yeast Sec22p) (17), is required early in protein receptor (SNARE) protein ERS24͞Sec22b and that J774- the phagocytic process. -

Brefeldin A: Deciphering an Enigmatic Inhibitor of Secretion
Update on Brefeldin A Brefeldin A: Deciphering an Enigmatic Inhibitor of Secretion Andreas Nebenfu¨ hr, Christophe Ritzenthaler, and David G. Robinson* Department of Botany, University of Tennessee, Knoxville, Tennessee 37996–1100 (A.N.); Institut de Biologie Mole´culaire des Plantes du Centre National de la Recherche Scientifique, 67084 Strasbourg cedex, France (C.R.); and Heidelberg Institute for Plant Sciences, University of Heidelberg, D–69120 Heidelberg, Germany (D.G.R.) The fungal macrocyclic lactone brefeldin A (BFA) BFA-sensitive GEFs are localized to the Golgi appa- has proved to be of great value as an inhibitor of ratus of mammalian and yeast cells (Spang et al., protein trafficking in the endomembrane system of 2001). Thus, one of the earliest and best characterized mammalian cells (Sciaky et al., 1997). BFA has also effects of BFA in nonplant organisms is the loss of often been used as an inhibitor of secretion and vac- COPI coats from the Golgi apparatus (Kreis et al., uolar protein transport in plant cells, but just exactly 1995). how BFA achieves these effects has been a matter of In recent years, it has become apparent that the debate for some time (e.g. Satiat-Jeunemaitre et al., molecular targets for BFA also exist in plant cells. The 1996; Staehelin and Driouich, 1997). The apparently Arabidopsis gene GNOM encodes an Arf GEF that broad spectrum of BFA responses, combined with a falls into the subgroup of BFA-sensitive Sec7-like lack of understanding of the primary target of BFA, proteins (Steinmann et al., 1999). Although the intra- has made it difficult to develop a coherent explana- cellular localization of GNOM is not yet known, most tion of BFA effects, which in turn has led to a series data are consistent with its Golgi localization, in ac- of misconceptions that riddle the plant literature.