An Integrative Guide to Sacroiliac Joint Dysfunction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peripartum Pubic Symphysis Diastasis—Practical Guidelines
Journal of Clinical Medicine Review Peripartum Pubic Symphysis Diastasis—Practical Guidelines Artur Stolarczyk , Piotr St˛epi´nski* , Łukasz Sasinowski, Tomasz Czarnocki, Michał D˛ebi´nski and Bartosz Maci ˛ag Department of Orthopedics and Rehabilitation, Medical University of Warsaw, 02-091 Warsaw, Poland; [email protected] (A.S.); [email protected] (Ł.S.); [email protected] (T.C.); [email protected] (M.D.); [email protected] (B.M.) * Correspondence: [email protected] Abstract: Optimal development of a fetus is made possible due to a lot of adaptive changes in the woman’s body. Some of the most important modifications occur in the musculoskeletal system. At the time of childbirth, natural widening of the pubic symphysis and the sacroiliac joints occur. Those changes are often reversible after childbirth. Peripartum pubic symphysis separation is a relatively rare disease and there is no homogeneous approach to treatment. The paper presents the current standards of diagnosis and treatment of pubic diastasis based on orthopedic and gynecological indications. Keywords: pubic symphysis separation; pubic symphysis diastasis; pubic symphysis; pregnancy; PSD 1. Introduction The proper development of a fetus is made possible due to numerous adaptive Citation: Stolarczyk, A.; St˛epi´nski,P.; changes in women’s bodies, including such complicated systems as: endocrine, nervous Sasinowski, Ł.; Czarnocki, T.; and musculoskeletal. With regard to the latter, those changes can be observed particularly D˛ebi´nski,M.; Maci ˛ag,B. Peripartum Pubic Symphysis Diastasis—Practical in osteoarticular and musculo-ligamento-fascial structures. Almost all of those changes Guidelines. J. Clin. Med. -

Lower Back Pain and the Sacroiliac Joint What Is the Sacroiliac Joint?
PATIENT INFORMATION Lower Back Pain and the Sacroiliac Joint What is the Sacroiliac Joint? Your Sacroiliac (SI) joint is formed by the connection of the sacrum and iliac bones. These two large bones are part of the pelvis Sacroiliac and are held together by a collection of joint ligaments. The SI joint supports the weight of your upper body which places a large amount of stress across your SI joint. What is Sacroiliac Joint Disorder? The SI joint is a documented source of lower back pain. The joint is the most likely source of pain in 30% of patients with lower back pain. Pain caused by sacroiliac joint disorder can be felt in the lower back, buttocks, or legs. Sacroiliac joint fixation is indicated in patients with severe, chronic sacroiliac joint pain who have failed extensive conservative measures, or in acute cases of trauma. What are potential symptoms? • Lower back pain • Lower extremity pain (numbness, tingling, weakness) • Pelvis/buttock pain • Hip/groin pain • Unilateral leg instability (buckling, giving away) • Disturbed sleep patterns • Disturbed sitting patterns (unable to sit for long periods of time on one side) • Pain going away from sitting to standing How is Sacroiliac Joint Disorder diagnosed? Sacroiliac joint disorder is diagnosed by the patient’s history, physical findings, radiological investigations and SI joint injections. Sacroiliac injection, which is the gold standard for confirming SI joint disorder will be delivered with fluoroscopic or CT guidance to validate accurate placement of the needle in the SI joint. What is the Orthofix SambaScrew®? Your surgeon has chosen the SambaScrew because it utilizes a minimally invasive surgical technique to sacroiliac fixation. -

Chronic Sacroiliac Joint and Pelvic Girdle Pain and Dysfunction
Chronic Sacroiliac Joint and Pelvic Girdle Pain and Dysfunction Successfully Holly Jonely, PT, ScD, FAAOMPT1,3 Melinda Avery, PT, DPT1 Managed with a Multimodal and Mehul J. Desai, MD, MPH2,3 Multidisciplinary Approach: A Case Series 1The George Washington University, Department of Health, Human Function and Rehabilitation Sciences, Program in Physical Therapy, Washington, DC 2The George Washington University, School of Medicine & Health Sciences, Department of Anesthesia & Critical Care, Washington, DC 3International Spine, Pain & Performance Center, Washington, DC ABSTRACT PGP, impairments of the SIJ are not lim- Case 2 Background and Purpose: Sacroiliac ited to intraarticular pain and often include A 30-year-old nulliparous female with joint (SIJ) or pelvic girdle pain (PGP) account impairments of the surrounding muscles or a chronic history of right posterior pelvic for 20-40% of all low back pain cases in the connective tissues, as well as, aberrant and pain following an injury as a college athlete United States. Diagnosis and management asymmetrical movement patterns within the participating in crew. She reported slipping of these disorders can be challenging due to region of the lumbo-pelvic-hip complex.7 in a boat and falling onto her sacrum. Her limited and conflicting evidence in the lit- These impairments have a negative impact previous conservative management included erature and the varying patient presentation. on the PG’s role in support and load trans- physical therapy that emphasized pelvic The purpose of this case series is to describe fer between the lower extremities and trunk. manipulations, use of a pelvic belt, and stabi- the outcome observed in 3 patients present- This ariabilityv in observed impairments lization exercises. -

The Sacroiliac Problem: Review of Anatomy, Mechanics, and Diagnosis
The sacroiliac problem: Review of anatomy, mechanics, and diagnosis MYRON C. BEAL, DD., FAAO East Lansing, Michigan methods have evolved along with modifications in Studies of the anatomy of the the hypotheses. Unfortunately, definitive analysis sacroiliac joint are reviewed, of the sacroiliac joint problem has yet to be including joint changes associated achieved. with aging and sex. Both descriptive Two excellent reviews of the medical literature and analytical investigations of joint on the sacroiliac joint are by Solonen i and a three- movement are presented, as well as part series by Weisl. clinical hypotheses of sacroiliac joint The present treatise will review the anatomy of motion. The diagnosis of sacroiliac the sacroiliac joint, studies of sacroiliac move- joint dysfunction is described in ment, hypotheses of sacroiliac mechanics, and the detail. diagnosis of sacroiliac dysfunction. Anatomy The formation of the sacroiliac joint begins during the tenth week of intrauterine life, and the joint is fully developed by the seventh month. The joint In recent years it has been generally recognized surfaces remain flat until sometime after puberty; that the sacroiliac joints are capable of movement. smooth surfaces in the adult are the exception. The clinical significance of sacroiliac motion, or The contour of the joint surface continues to lack of motion, is still subject to debate. The role of change with age. 2m In the third and fourth decades the sacroiliac joints in body mechanics can be illus- there is an increase in the number and size of the trated by a mechanical analogy. A 1 to 2 mm. mal- elevations and depressions, which interlock and alignment of a bearing in a machine can cause ab- limit mobility. -

Sacroiliac Joint Dysfunction a Case Study
NOR200188.qxd 3/8/11 9:53 PM Page 126 Sacroiliac Joint Dysfunction A Case Study CPT William Murray Pain is a widespread issue in the United States. Nine of physical therapist. She was evaluated and her treatment 10 Americans regularly suffer from pain, and nearly every consisted of a transcutaneous electrical nerve stimula- person will experience low back pain at one point in their lives. tion unit while in the PT clinic, aqua therapy, and ice Undertreated or unrelieved pain costs more than and heat application. $60 billion a year from decreased productivity, lost income, After several weeks, Ms. T returned to the primary care and medical expenses. The ability to diagnose and provide ap- provider and informed her that the pain has not decreased and “feels like that it is getting worse.” She also informed propriate medical treatment is imperative. This case study ex- the provider that she was having difficulty sleeping and amines a 23-year-old Active Duty woman who is preparing to constantly feeling tired secondary to pain. Throughout the be involuntarily released from military duty for an easily cor- next several months, the primary care provider tried nu- rectable medical condition. She has complained of chronic low merous medication trials with no relief for the patient. Ms. back pain that radiates into her hip and down her leg since ex- T gives a history of being prescribed numerous medica- periencing a work-related injury. She has been seen by numer- tions within several drug classifications. She stated vari- ous providers for the previous 11 months before being referred ous side effects that are related to the medications and to the chronic pain clinic. -

Sacroiliac Joint Imaging
Sacroiliac Joint Imaging Jacob Jaremko, MD, PhD Edmonton, Canada SPR, May 2017 Longview, Alberta © Overview . SI joint anatomy . Sacroiliitis pathophysiology . Sacroiliitis imaging . Disease features . Imaging protocols . Role in diagnosis of JIA / JSpA sidysfunction.com SIJ Anatomy . Largest synovial joint in the body… . but little synovium . and minimal motion . Complex shape . Restraining ligaments . Normal 2.5, 0.7 mm . (lax in pregnancy) . Sturesson et al., Spine 1969; 14: 162-5 SIJ Microscopic Anatomy . Synovial part . Ventral, inferior 1/3 – 1/2 . Traditional joint with fluid, synovium, cartilage . Unique fibrocartilage . Normally non-enhancing . Ligamentous part . Dorsal, superior ½ - d2/3 . Non-synovial; enthesis organ . Variants, vascular channels, normally enhancing . Puhakka et al., Skel Radiol 2004; 33:15–28 SIJ normal X-ray appearance . Curvilinear . Overlapping structures & bowel 1 year earlier, age 3 SIJ Pathology Abdominal pain . Case: . 4 year old boy . Post MVC . pneumothorax . liver laceration Age 4 . bony injury? MVC 1 year earlier, age 3 SIJ Trauma Abdominal pain . 4 yr M . Post MVC . Sacral fracture . Widened SI joint . Subtle on Xray Age 4 MVC Sacroiliitis . Clinical: . Deep low-back pain worst in AM, tender SIJ . Xray, CT, MRI: . Several imaging features 11 yr M, asymptomatic 12 yr M, known JSpA Sacroiliitis Pathophysiology . SI joints . Dense fibrocartilage . Bone/cartilage interface resembles an enthesis . Synovium at margins Bone Fibrocartilage Joint Synovium Sacroiliitis Pathophysiology . Initial insult = autoimmune attack of subchondral bone Bone Fibrocartilage Joint Synovium BME Sacroiliitis Pathophysiology . Initial insult = autoimmune attack of subchondral bone . Followed by destruction of cortical bone (erosion) . Opposite of RA – inflammation begins in bone, not at synovium Bone Fibrocartilage Joint Synovium Erosion Sacroiliitis Pathophysiology . -

Sacroiliac Joint Dysfunction and Piriformis Syndrome
Classic vs. Functional Movement Approach in Physical Therapy Setting Crista Jacobe-Mann, PT Nevada Physical Therapy UNR Sports Medicine Center Reno, NV 775-784-1999 [email protected] Lumbar Spine Intervertebral joints Facet joints Sacroiliac joint Anterior ligaments Posterior ligaments Pelvis Pubic symphysis Obturator foramen Greater sciatic foramen Sacrospinous ligament Lesser sciatic foramen Sacrotuberous ligament Hip Capsule Labrum Lumbar spine: flexion and extension ~30 total degrees of rotation L1-L5 Facet joints aligned in vertical/saggital plane SI joints 2-5 mm in all directions, passive movement, not caused by muscle activation Shock absorption/accepting load with initial contact during walking Hip Joints Extension 0-15 degrees 15% SI joint pain noted in chronic LBP patients Innervation: L2-S3 Classic signs and symptoms Lower back pain generally not above L5 transverse process Pain can radiate down posterior thigh to posterior knee joint, glutes, sacrum, iliac crest sciatic distribution Pain with static standing, bending forward, donning shoes/socks, crossing leg, rising from chair, rolling in bed Relief with continuous change in position Trochanteric Bursitis Piriformis Syndrome Myofascial Pain Lumbosacral Disc Herniation and Bulge Lumbosacral Facet Syndrome J. Travell suspects Si joint pain may causes piriformis guarding and lead to Piriformis syndrome… Tenderness to palpation of PSIS, lower erector spinae, quadratus lumborum and gluteal muscles Sometimes positive SLR Limited hip mobility -

Diagnosis and Treatment Sacroiliac Joint Pain | Blue Cross NC
Corporate Medical Policy Diagnosis and Treatment of Sacroiliac Joint Pain File Name: diagnosis_and_treatment_of_sacroiliac_joint_pain Origination: 8/2010 Last CAP Review: 4/2021 Next CAP Review: 4/2022 Last Review: 4/2021 Description of Procedure or Service Sacroiliac joint (SIJ) arthrography using fluoroscopic guidance with injection of an anesthetic has been explored as a diagnostic test for sacroiliac joint pain. Duplication of the patient’s pain pattern with the injection of contrast medium suggests a sacroiliac etiology, as does relief of chronic back pain with injection of local anesthetic. Treatment of sacroiliac joint pain with corticosteroids, radiofrequency ablation (RFA), stabilization, or minimally invasive sacroiliac joint fusion has also been explored. Similar to other structures in the spine, it is assumed that the sacroiliac joint may be a source of low back pain. In fact, prior to 1928, the sacroiliac joint was thought to be the most common cause of sciatica. In 1928, the role of the intervertebral disc was elucidated, and from that point forward the sacroiliac joint received less research attention. Research into sacroiliac joint pain has been plagued by lack of a criterion standard to measure its prevalence and against which various clinical examinations can be validated. For example, sacroiliac joint pain is typically without any consistent, demonstrable radiographic or laboratory features and most commonly exists in the setting of morphologically normal joints. Clinical tests for sacroiliac joint pain may include various movement tests, palpation to detect tenderness, and pain descriptions by the patient. Further confounding the study of the sacroiliac joint is that multiple structures, such as posterior facet joints and lumbar discs, may refer pain to the area surrounding the sacroiliac joint. -
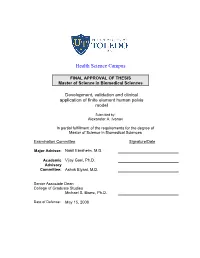
Development, Validation and Clinical Application of Finite Element Human Pelvis Model
Health Science Campus FINAL APPROVAL OF THESIS Master of Science in Biomedical Sciences Development, validation and clinical application of finite element human pelvis model Submitted by: Alexander A. Ivanov In partial fulfillment of the requirements for the degree of Master of Science in Biomedical Sciences Examination Committee Signature/Date Major Advisor: Nabil Ebraheim, M.D. Academic Vijay Goel, Ph.D. Advisory Committee: Ashok Biyani, M.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: May 15, 2008 A Thesis Entitled Development, Validation and Clinical Application of the Finite Element Model of Human Pelvis. By Alexander A. Ivanov, M.D. Submitted as partial fulfillment of the requirements for the Master of Science in Orthopaedic Science ______________________________ Advisor: Dr. Nabil A. Ebraheim, M.D. ______________________________ Co-Advisor: Dr. Vijay K. Goel, Ph.D. ______________________________ Graduate School The University of Toledo 2008 1 © 2008, Alexander A. Ivanov 2 College of Health Science I HEREBY RECOMMEND THAT THE THESIS PREPARED UNDER MY SUPERVISION BY: Alexander A Ivanov, M.D. ENTITLED: Development, validation and clinical application of finite element human pelvis model BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF: Master of Science in Orthopaedic Science ______________________________________________________________ Thesis Advisor: Dr. Nabil A. Ebraheim, M.D. _______________________________________________________________ Thesis Co-Advisor: Dr. Vijay K. Goel, Ph.D. Recommendation concurred by: ___________________________________ Committee Dr.Ashok Biyani, M.D. Of Final Examination ________________________________________________________________ Dean, College of Health Science 3 Acknowledgment I would like to extend my gratitude to my advisors Dr. Nabil Ebraheim and Dr. Vijay Goel for their incredible support of this work. -

Biomechanics of the Sacroiliac Joint: Part I−−Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain
Biomechanics of the Sacroiliac Joint: Part I−−Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain Ali Kiapour, Amin Joukar, Hossein Elgafy, Deniz U. Erbulut, Anand K. Agarwal and Vijay K. Goel Int J Spine Surg published online 30 December 2019 http://ijssurgery.com/content/early/2019/12/30/6077 This information is current as of September 23, 2021. Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://ijssurgery.com/alerts The International Journal of Spine Surgery 2397 Waterbury Circle, Suite 1, Aurora, IL 60504, Phone: +1-630-375-1432 © 2019 ISASS. All RightsDownloaded Reserved. from http://ijssurgery.com/ by guest on September 23, 2021 International Journal of Spine Surgery, Vol. 00, No. 00, 0000, pp. 000–000 https://doi.org/10.14444/6077 ÓInternational Society for the Advancement of Spine Surgery Biomechanics of the Sacroiliac Joint: Part I—Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain ALI KIAPOUR, PHD,1,2 AMIN JOUKAR, MS,1 HOSSEIN ELGAFY, MD,1 DENIZ U. ERBULUT, PHD,1 ANAND K. AGARWAL, MD,1 VIJAY K. GOEL, PHD1 1Engineering Center for Orthopaedic Research Excellence (E-CORE), Departments of Bioengineering and Orthopaedics, The University of Toledo, Toledo, Ohio; 2Department of Neurosurgery, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts ABSTRACT Background: The sacroiliac joints (SIJs), the largest axial joints in the body, sit in between the sacrum and pelvic bones on either side. They connect the spine to the pelvis and thus facilitate load transfer from the lumbar spine to the lower extremities. The majority of low back pain (LBP) is perceived to originate from the lumbar spine; however, another likely source of LBP that is mostly overlooked is the SIJ. -

ROCHESTER REGIONAL HEALTH SPINE CENTER Sacroiliac Joint Pain
ROCHESTER REGIONAL HEALTH SPINE CENTER Sacroiliac Joint Pain (also commonly called SI Joint Pain) Overview The sacroiliac (SI) joints are formed by the connection of the sacrum and the right and left iliac bones. The sacrum is the triangular-shaped bone in the lower portion of the spine, below the lumbar spine. While most of the bones (vertebrae) of the spine are mobile, the sacrum is made up of fused vertebrae that do not move. The iliac bones are the two large bones that make up the pelvis. As a result, the SI joints connect the spine to the pelvis. The sacrum and the iliac bones (ileum) are held sacroiliac (SI) joint sacroiliac (SI) joint together by a collection of strong ligaments. There is relatively little motion at the SI joints. There are normally less than 4 degrees of rotation and 2mm of translation at these joints. Most of the motion in the area of the pelvis occurs either at the hips or the lumbar spine. These joints need to support the entire weight of the upper body when we are erect, which places a large amount of stress across them. This can lead to wearing of the cartilage of the SI joints and eventually, arthritis. There are many different terms for sacroiliac joint problems, including SI joint dysfunction, SI joint syndrome, SI joint strain to a condition that causes pain to the SI joints due to a ilium ilium and SI joint inflammation. Each of these terms refers variety of possible causes. Causes & Symptoms The most common symptom of SI joint dysfunction is pain. -

An Exploration of Ultrasound-Guided Therapeutic Injection of the Dorsal Interosseous Ligaments of the Sacroiliac Joint for Mechanical Dysfunction of the Joint
Central JSM Pain and Management Bringing Excellence in Open Access Research Article *Corresponding author M. Cusi, 15 Vernon Street, Strathfield, NSW 2135, Australia, Tel: 61-2-9746-6360; 61-0-438-419-615; Email: An Exploration of Ultrasound- Submitted: 08 Augsut 2016 Guided Therapeutic Injection Accepted: 31 August 2016 Published: 02 September 2016 Copyright of the Dorsal Interosseous © 2016 Cusi et al. Ligaments of the Sacroiliac OPEN ACCESS Keywords • Ultrasound Joint for Mechanical • Dorsal interosseous ligament • Sacroiliac joint • Sacroiliac joint incompetence Dysfunction of the Joint • SPECT/ CT Jennifer Saunders1, Mel Cusi1*, Lisa Hackett2, and Hans Van der Wall3 1Sydney School of Medicine, University of Notre Dame, Australia 2Orthopaedic Research Institute, University of NSW, Australia 3Concord Nuclear Imaging & Sydney School of Medicine, University of Notre Dame Sydney, Australia Abstract Mechanical dysfunction of the sacroiliac joint is a common cause of lateralising low back pain in young patients in either the peri-partum period or after trauma. Diagnosis is based on evidence-based clinical guidelines and fused scintigraphic tomographic and x-ray computed tomography studies (SPECT/ CT). Accurate diagnosis is important as up to 80% of these patients respond to directed physiotherapy. The remainder can respond to prolotherapy with injection into the dorsal interosseous ligament of the sacroiliac joint. We describe a technique for injection of this structure under ultrasound guidance. Injections into this structure using simple landmarks, allow reproduction of the typical symptoms and pain maps indicating good accuracy in the 36 patients studied. INTRODUCTION functional and pain outcomes [8-11]. A proportion that does not The lifetime prevalence of low back pain has been reported to respondthat with to specific physiotherapy therapy, appearsapproximately to respond 80% towill image-guided regain good be as high as 84% with the prevalence of chronic low back pain prolotherapy with hypertonic dextrose or platelet-enriched being approximately 23% [1].