Ulnar Collateral Ligament Reconstruction: Where Do We Stand in 2021? Brandon J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LONG ISLAND UNIVERSITY MEN’S LACROSSE GAME 2 GAME INFO Series History LIU (0-1, 0-0 NEC) VS
LONG ISLAND UNIVERSITY MEN’S LACROSSE GAME 2 GAME INFO Series History LIU (0-1, 0-0 NEC) VS. WAGNER (0-1, 0-0 NEC) Overall 0-0 Saturday, February 15 • 1:00 p.m. • Brookville, N.Y. • Bethpage Federal Credit Union Stadium Last Meeting First Meeting SHARKS SEAHAWKS Head Coach: Eric Wolf Head Coach: Bill McCutcheon Record at LIU: 21-11 Record at Wagner: 2-13 MEDIA COVERAGE Career Record: 21-11 Career Record: 2-13 Last Game: Lost at Siena Last Game: Lost at Hofstra Live Video NEC Front Row Live Stats LIUAthletics.com OPENING FACE-OFF 2020 SCHEDULE FOLLOW THE SHARKS • Despite being separated by just 31 miles, FEBRUARY Social Media Men’s Lacrosse Twitter @LIUMLAX Saturday will mark the first ever meeting 8 AT SIENNA (L) 14-12 Men’s Lacrosse Instagram @liumlacrosse between LIU and Wagner in men’s lacrosse. 15 WAGNER 1:00 P.M. LIU Athletics Twitter @LIUAthletics 22 ST. JOHN’S 1:00 P.M. LIU Athletics Instagram @LIUAthletics • The Sharks opened their 2020 LIU Website LIUAthletics.com 29 AT HOFSTRA 1:00 P.M. campaign and first season of Division MARCH I competition since 1992 at Siena on 3 AT FAIRFIELD 7:00 P.M. LIU AT A GLANCE Saturday, Feb. 8, falling by a 14-12 7 QUINNIPIAC 2:00 P.M. Primary Media Contact Casey Schermick margin despite a big fourth-quarter run. 10 AT UMASS 2:00 P.M. Office Phone (516) 299-3957 14 NJIT * 12:00 P.M. Cell Phone (516) 532-0852 • Several LIU newcomers had strong E-Mail [email protected] 21 SACRED HEART * 1:00 P.M. -

“Italian Immigrants” Flourish on Long Island Russell Burke Associate Professor Department of Biology
“Italian Immigrants” Flourish on Long Island Russell Burke Associate Professor Department of Biology talians have made many important brought ringneck pheasants (Phasianus mentioned by Shakespeare. Also in the contributions to the culture and colchicus) to North America for sport late 1800s naturalists introduced the accomplishments of the United hunting, and pheasants have survived so small Indian mongoose (Herpestes javan- States, and some of these are not gen- well (for example, on Hofstra’s North icus) to the islands of Mauritius, Fiji, erally appreciated. Two of the more Campus) that many people are unaware Hawai’i, and much of the West Indies, Iunderappreciated contributions are that the species originated in China. Of supposedly to control the rat popula- the Italian wall lizards, Podarcis sicula course most of our common agricultural tion. Rats were crop pests, and in most and Podarcis muralis. In the 1960s and species — except for corn, pumpkins, cases the rats were introduced from 1970s, Italian wall lizards were imported and some beans — are non-native. The Europe. Instead of eating lots of rats, the to the United States in large numbers for mongooses ate numerous native ani- the pet trade. These hardy, colorful little mals, endangering many species and lizards are common in their home coun- Annual Patterns causing plenty of extinctions. They also try, and are easily captured in large num- 3.0 90 became carriers of rabies. There are 80 2.5 bers. Enterprising animal dealers bought 70 many more cases of introductions like them at a cut rate in Italy and sold them 2.0 60 these, and at the time the scientific 50 1.5 to pet dealers all over the United States. -
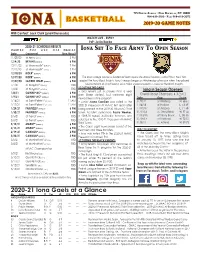
2020-21 Iona Gaels at a Glance No
715 NORTH AVENUE • NEW ROCHELLE, NY 10801 914-633-2310 • FAX: 914-633-2072 2019-20 GAME NOTES WBB Contact: Jack Clark ([email protected]) WATCH LIVE - ESPN+ PxP: Justin Rocke 2020-21 SCHEDULE/RESULTS Overall: 0-0 H: 0-0 A: 0-0 N: 0-0 MAAC: 0-0 IONA SET TO FACE ARMY TO OPEN SEASON Date Opponent Time/Result 11/29/20 at Army (ESPN+) 3 PM 12/4/20 BRYANT (ESPN3/+) 6 PM 12/11/20 at Monmouth* (ESPN3/+) 7 PM 12/12/20 at Monmouth* (ESPN3/+) 7 PM 12/18/20 RIDER* (ESPN3/+) 6 PM 12/19/20 RIDER* (ESPN3/+) 6 PM The Iona College women’s basketball team opens the 2020-21 season in West Point, New York 12/22/20 SACRED HEART (ESPN3/+) 6 PM against the Army Black Knights. Army’s season began on Wednesday afternoon when they played host to Hofstra at Christl Arena. Alisa Fallon scored 23 points in a loss for the Black Knights. 1/1/21 at Niagara* (ESPN3/+) TBD SCOUTING THE GAELS 1/2/21 at Niagara* (ESPN3/+) TBD • Iona returns just six players from a year Iona in Season Openers 1/8/21 QUINNIPIAC* (ESPN3/+) 6 PM prior (three starters), but welcome eight Overall Under Chambers: 4-3 (.571) 1/9/21 QUINNIPIAC* (ESPN3/+) 6 PM newcomers to the program. Date Opp. Score 1/16/21 at Saint Peter’s* (ESPN3/+) 11 AM • Junior Juana Camilion was voted to the 11/9/19 at Winthrop W, 68-61 1/17/21 at Saint Peter’s* (ESPN3/+) 11 AM 2020-21 Preseason All-MAAC First Team after 11/6/18 at Hofstra L, 74-49 1/29/21 FAIRFIELD* (ESPN3/+) 6 PM being named to the 2019-20 All-MAAC Third 11/10/17 at Arizona L, 71-58 1/30/21 FAIRFIELD* (ESPN3/+) 6 PM Team. -

The Lawrence Herbert School of Communication
The Lawrence Herbert School of Communication The Lawrence Herbert School of Communication educates Highlights students to master, excel in, and provide leadership for the future of media. A curriculum that provides strong technical skills while • LinkedIn ranked Hofstra as the No. 2 school for media remaining steadfastly committed to a liberal arts foundation professionals based on alumni career outcomes. means that our graduates are ready for the jobs out there today, • The Department of Radio, TV, Film is one of just 19 programs but are also able to adapt to new conditions in the years and selected nationwide as one of Variety magazine’s 2016 “Best decades ahead. Showbiz Programs.” • The Sports Media concentration in the BA in Journalism program The school was named in 2013 in honor of Lawrence Herbert ’51, educates future producers, writers, reporters and anchors for this growing and important field. inventor of the Pantone Matching System and former chairman and CEO of Pantone, Inc. Mr. Herbert’s transformative • Four students were selected to participate in NBCUniversal’s 2016 commitment allows the Herbert School to innovate and keep Summer Olympics Internship Program. pace with a rapidly changing media landscape. • WRHU-88.7 FM won the prestigious National Association of Broadcasters Marconi Radio Award as the non-commercial station of the year in 2014, and was a finalist in 2016. The Princeton Departments and Programs Review ranked WRHU the #1 college radio station in the U.S. in 2015 and 2016. Journalism, Media Studies, and Public Relations • Hofstra is among an elite group of institutions recognized by the Accrediting Council on Education in Journalism and Mass • BA – Journalism; Mass Media Studies; Public Relations Communications (ACEJMC) for its commitment to the highest • BA/MA – Journalism • MA – Journalism • MA – Public Relations standards of teaching and programming excellence. -

2013-14 Men's Basketball Media Guide
HOFSTRA 2013-14 MEN’S BASKETBALL MEDIA GUIDE 1 Stephen Nwaukoni 2 IT STARTS WITH THE FUSE THAT THE GAME LIGHTS INSIDE US. PASSION IS EXCHANGED BETWEEN THE COURT AND THE STANDS. ENERGY BECOMES SYNERGY. OUR UNCOMMON DESIRE BECOMES OUR COMMON GROUND. BECAUSE THIS SEASON, IT'S ABOUT INTENSITY. IT'S DRIVEN BY INNOVATION THAT ELEVATES, AND SPEED THAT WILL RISE. THE GAME WILL BECOME FASTER, AND PRIDE WILL BURN HOTTER. IN ARENAS ALL OVER THE COUNTRY, INTENSITY WILL INSPIRE COLLEGE FANS AND COLLEGE PLAYERS TO UNITE AS ONE. ~ 2 Table of Contents Nike . 3 Table of Contents . 4 Hofstra Highlights . 6 Hofstra Facilities . 8 Hofstra Game Day . 10 2013-14 Quick Facts12 . Media Information . 14 Media Following . 15 Strength and Conditioning . 16 Player Development . 17 Hofstra in the Community . 18 Hofstra Athletics . 19 Joe Mihalich . 20 Mike Farrelly . 24 Shane Nichols . 25 Craig “Speedy” Claxton . 26 Colin Curtin/Managers . 27 Support Staff . 28 2013-14 Roster . 29 2013-14 Outlook . 30 Meet the Pride . 32 Stephen Nwaukoni . 34 Moussa Kone . 36 Jordan Allen . 38 Darren Payen . 40 Adam Savion . 42 Dion Nesmith . 44 Zeke Upshaw . 46 Eliel Gonzalez . 48 Chris Jenkins . 50 Jamall Robinson . 52 Brian Bernardi . 54 Juan’ya Green . 56 Ameen Tanksley . 58 This is Hofstra . 60 Hofstra University President . 62 University Senior Administration/Trustees . 63 Director of Athletics . 64 Athletics Administration and Head Coaches . 66 University Academic Support . 68 Sports Medicine . 69 Long Island . 70 New York City . 71 David S . Mack Sports and Exhibition Complex . 72 Madison Square Garden/Barclays Center . 74 The Colonial Athletic Association . -
2019-2020 Newsletter -PDF
Sport Management Sport Analytics Syracuse2019-2020 Newsletter Persevering Through 2020’s Challenges How our students, faculty and alumni embraced virtual learning, remote employment View a text-based accessible version CO VER ST OR Y Persevering Through How our students, faculty and alumni embraced virtual learning, remote employment We welcomed a new decade with innovative ideas and graduated our largest class of students in May 2020, but even with the excitement surrounding major milestones, this new chapter did not unfold as we – or anyone - had planned. We persevered through a pandemic and we could not have done it without the unwavering commitment from our Sport Management faculty and staff, the understanding and flexibility of our students, the guidance from Falk College and Syracuse University leadership, and the loyal support of our alumni and advisory council members. So many of our events, trips, conferences, presentations, lectures and internships were canceled or cut short, including senior Capstones, graduate practicums, Los Angeles Immersion, Syracuse Sport Business Conference, Berlin Sport Analytics Faculty adapt from classroom instruction to online teaching Undergraduate director Dr. Gina Pauline dents both online and in person. I also experienced the challenges of being The Spring 2020 semester brought an unexpected challenge that no one a full-time working mother with three kids at home who were also learning saw coming. Think about it, 20 years from now, we will look back on this remotely. It was a juggling act for sure! We all came out stronger in the end year and say, “Remember when you were quarantined at home for months and I’m proud of my family, our students and everyone in the department and everything was shut down due to a global pandemic?” Everyone will who worked together in these difficult times. -
Athletics at Hofstra and on Long Island
Athletics at Hofstra and on Long Island: An exhibit that highlights some fun facts, interesting historical items and photographs of teams and individuals in our sports history. Root, root, root for the home team! All materials from Hofstra University Archives and Long Island Studies, Hofstra Pride: Athletics at Hofstra University Women’s basketball team, 1936, note the name on the bus: Hofstra College was associated with NYU until 1939. Women’s championship basketball team, 1939-40. Helena Mroczkowska Dow, was not only an Olympic fencing champion, but she flew planes! A member of the class of 1940 she was involved in student government, but it was her fencing prowess that brought her to national attention. She was a member of a remarkable Olympic family; her husband fenced in the 1936 Olympics in Berlin and was captain of the 1948 US Olympic fencing team. Helena fenced in the 1948 Olympics in London and her son, Robert, fenced sabre in the 1972 Olympics in Munich. It is believed that they are the only “Mother-Father-Son” trio in any sport in US Olympic history. The wrestling squad of 1945-46 went undefeated although they didn’t organize as a team until two years later. In the 1950’s Hofstra played baseball games at Ebbets Field against St. John’s. The Dodgers left town after the 1957 season and the demolition of the stadium began in February of 1960. This photo from 1951. The first time cheerleaders organized at Hofstra was in 1947, this squad from 1952 wears traditional saddle shoes and Hofstra sweaters. -

To Apply for Undergraduate Admission As A
Hofstra University Office of Undergraduate Admission 100 Hofstra University Hempstead, NY 11549-1000 516-463-6700 hofstra.edu To Apply for Undergraduate Admission as a First-Year Student First-year undergraduate candidates to Hofstra University may apply by using this paper application or by using our online application at hofstra.edu/apply. Please be advised that all materials and documents submitted as part of an application become the property of Hofstra University and cannot be returned to the applicant. A first-year undergraduate applicant is a current high school senior, a high school graduate with no postsecondary coursework, or the recipient of a high school equivalency applying for matriculated (degree-seeking) status at Hofstra University. First-year candidates may apply as Early Action or Regular Decision. Early Action is a nonbinding early application and notification process for fall semester first-year students only. Students accepted via Early Action are not required to withdraw other college applications, but are required to notify Hofstra University of their intentions by May 1. There are two rounds of Early Action as indicated in the chart below. Regular Decision candidates are considered on a “rolling basis.” While there is no deadline for regular decision applications, students are encouraged to apply early so as to receive the fullest consideration. Once your application and all supporting documents are received, the application is reviewed by our admission committee. Application Type Submission Decision Notification Begins Early Action 1 November 15 December 15 Early Action 2 December 15 January 15 Regular Decision Rolling February 1 and rolling basis thereafter CHECKLIST To apply, please submit the following: ❑ A completed, signed and dated 2021 First-Year Student Application for Undergraduate Admission. -

Hofstra University 2004-05 Men's Basketball
HOFSTRA UNIVERSITY Hofstra – ODU Quick Facts Series Record: ODU leads 6-4 2004-05 MEN’S BASKETBALL Current Streak: Hofstra – 1 straight SUPPLEMENTAL GAME NOTES This Year: Hofstra 66, ODU 63 (2/23 @ ODU) ODU 67, Hofstra 66 (1/19 @ Hofstra) Hofstra Coach: Tom Pecora (4th year), 55-63 (55-63 overall) #5 Hofstra (21-7, 12-6) at CAA Tournament ODU Coach: Blaine Taylor (4th year), 68-48 (210-113) Semifinals vs. #1 Old Dominion (26-5) Sunday, March 6, 3 p.m. Hofstra-ODU By the Numbers Hofstra ODU Richmond, VA/Richmond Coliseum 21-7 Record 26-5 12-6 CAA Record 15-3 TV/Radio: WRHU (88.7 FM), Metro Channel 73.4 Points Per Game 71.1 66.3 Opps. Points Per Game 60.2 +7.1 Scoring Margin +10.9 Streaks, Stats, and Storylines: 37.0 Rebounds Per Game 36.5 • Hofstra has won seven straight and 10 of its last 11. It also 35.0 Opps. Rebs Per Game 34.9 began the year with nine straight wins (and 10 of 11). +2.0 Rebounding Margin +1.6 13.4 Assists Per Game 16.6 • Hofstra was the only team to win at Old Dominion this 7.9 Steals Per Game 9.8 season, which it did on Feb. 23 (66-63). That win was also the th 14.2 Turnovers Per Game 12.0 1000 in Hofstra history (the Pride is now 1002-753 all-time). 14.8 Opps. TO Per Game 17.3 4.8 Blocks Per Game 4.7 • Both Hofstra-Old Dominion games this year came down to 45.7 Field Goal Pct. -

Maryland Players Selected in Major League Baseball Free-Agent Drafts
Maryland Players selected in Major League Baseball Free-Agent Drafts Compiled by the Maryland State Association of Baseball Coaches Updated 16 February 2021 Table of Contents History .............................................................................. 2 MLB Draft Selections by Year ......................................... 3 Maryland First Round MLB Draft Selections ................. 27 Maryland Draft Selections Making the Majors ............... 28 MLB Draft Selections by Maryland Player .................... 31 MLB Draft Selections by Maryland High School ........... 53 MLB Draft Selections by Maryland College .................. 77 1 History Major League Baseball’s annual First-Year Player Draft began in June, 1965. The purpose of the draft is to assign amateur baseball players to major league teams. The draft order is determined based on the previous season's standings, with the team possessing the worst record receiving the first pick. Eligible amateur players include graduated high school players who have not attended college, any junior or community college players, and players at four-year colleges and universities three years after first enrolling or after their 21st birthdays (whichever occurs first). From 1966-1986, a January draft was held in addition to the June draft targeting high school players who graduated in the winter, junior college players, and players who had dropped out of four-year colleges and universities. To date, there have been 1,170 Maryland players selected in the First-Year Player Drafts either from a Maryland High School (337), Maryland College (458), Non-Maryland College (357), or a Maryland amateur baseball club (18). The most Maryland selections in a year was in 1970 (38) followed by 1984 (37) and 1983 (36). The first Maryland selection was Jim Spencer from Andover High School with the 11th overall selection in the inaugural 1965 June draft. -

IONA GAELS BASKETBALL ROSTER NUMERICAL No
IONA GAELS BASKETBALL ROSTER NUMERICAL No. Name Cl. Pos. Ht. Wt. Hometown / Last School 0 Mo Thiam Sr. F 6-9 210 Dakar, Senegal / New Mexico State 2 E.J. Crawford Sr. G/F 6-6 210 Hartford, CT / St. Thomas More 3 Asante Gist Jr. G 5-11 185 East Orange, NJ / Eastern Kentucky 4 Parker Weiss Fr. G 6-3 170 Naples, FL / Community School of Naples 5 Ben Perez Sr. G 6-3 180 San Marcos, CA / South Plains Coll. (TX) 10 Andrija Ristanovic So. F 6-10 200 Belgrade, Serbia / Hillcrest Prep (AZ) 11 Isaiah Washington Jr. G 6-1 195 Harlem, NY / Minnesota 12 Tajuan Agee Sr. F 6-8 215 Chicago, IL / Hyde Park / Tyler JC (TX) 13 Colton Cashaw Jr. G 6-3 190 Charlotte, NC / Spartanburg Methodist (SC) 20 Isaiah Ross Jr. G 6-4 195 Davenport, IA / UMKC 24 Dylan van Eyck Jr. F 6-9 210 Boskoop, Netherlands / NE Oklahoma A&M 44 Niksa Nikolic Sr. F 6-8 234 Belgrade, Serbia / Southeastern CC (IA) Acting Head Coach: Tra Arnold (Biola '05) Assistant Coach: Ricky Johns (Utah '07) Assistant Coach: Jeff Mailhot (Cal Baptist '05) Assistant Coach: John Mateyko (American International '83) Graduate Manager: Taylor McHugh (Bryant '19) Video Coordinator: Ethan Nardone (Stony Brook ’11) Head Coach: Tim Cluess (Hofstra '83) Head Athletic Trainer: Sam De Rosa (Iona '87) Strength & Conditioning Coach: Kelly Shaver (Georgia State '07) Athletic Communications Contacts: Brian Beyrer (Iona '01), Jonathan Stanko (Iona '14) Team Managers: Brian Kerins '21, Omorede Rainey '22, Javier Rudales '23, Elijah Williams '23 BY CLASS: BY STATE: BY TENURE: Seniors (5) ...................................... -

Baseball:Layout 1 2/11/2008 11:38 AM Page 1
Baseball:Layout 1 2/11/2008 11:38 AM Page 1 ARKANSASBASEBALL STATE TABLE OF CONTENTS Table of Contents ......................................................1 Quick Facts .................................................................2 SEASON OUTLOOK .....................................................3 Grand Slam Banquet.................................................6 MEET THE 2008 ASU INDIANS .....................................7 page 3 2008 Roster..................................................................8 2008 Seniors ................................................................9 SEASON OUTLOOK 2008 Juniors...............................................................11 2008 Sophomores.....................................................17 2008 Freshmen..........................................................19 COACHES AND STAFF..............................................25 Head Coach Keith Kessinger..................................26 Assistant Coaches....................................................28 Support Staff .............................................................29 page 7 2007 YEAR IN REVIEW...............................................31 2007 Statistics............................................................33 Sophomore MEET THE INDIANS Infielder 2007 Results...............................................................34 Jordan Kimball INDIAN RECORD BOOK ...........................................35 Honors & Awards......................................................36 Individual Records