Chapter Ten Telepharmacy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
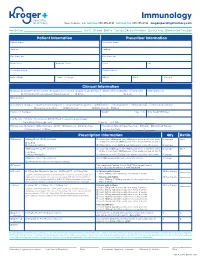
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -
DC Health Systems Plan 2017
DISTRICT OF COLUMBIA HEALTH SYSTEMS PLAN 2017 NOTICE OF NON-DISCRIMINATION In accordance with the D.C. Human Rights Act of 1977, as amended, D.C. Code section 2.1401.01 et seq., the District of Columbia does not discriminate on the basis of race, color, religion, national origin, sex, age, marital status, personal appearance, sexual orientation, family responsibilities, matriculation, political affiliation, disability, source of income, or place of residence or business. Discrimination in violation of the Act will not be tolerated. Violators will be subject to disciplinary action. Published July, 2017 Dear Residents: Upon taking office in 2015, my Administration focused on improving health outcomes for all residents, recognizing that all government policies—from education and housing, to economic development and transportation—impact the health and wellness of our communities. Every Washingtonian, regardless of where they live, should have the ability to live a healthy and fulfilling life in our nation’s capital. This Health Systems Plan will serve as a guide for all stakeholders as they implement initiatives aimed at strengthening Washington DC’s health system to improve the overall health status of residents by ad- dressing social determinants of health and promoting health equity. Through this plan, we will ensure that public and private agencies throughout DC have the direction they need to make sound investments and implement initiatives that will improve the health and well-being of residents across all eight wards. I am proud of the work we have done thus far. In 2016, the number of newly diagnosed HIV cases in Washington, DC decreased by 52 percent to 347. -

Clinical Pharmacy Specialist
SAMPLE JOB DESCRIPTION Clinical Pharmacist Specialist I. JOB SUMMARY The Clinical Pharmacist Specialists are responsible and accountable for the provision of safe, effective, and prompt medication therapy. Through various assignments within the department, they provide support of centralized and decentralized medication-use systems as well as deliver optimal medication therapy to patients with a broad range of disease states. Clinical Pharmacist Specialists proficiently provide direct patient-centered care and integrated pharmacy operational services in a decentralized practice setting with physicians, nurses, and other hospital personnel. These clinicians are aligned with target interdisciplinary programs and specialty services to deliver medication therapy management within specialty patient care services and to ensure pharmaceutical care programs are appropriately integrated throughout the institution. In these clinical roles, Clinical Pharmacist Specialists participate in all necessary aspects of the medication-use system while providing comprehensive and individualized pharmaceutical care to the patients in their assigned areas. Pharmaceutical care services include but are not limited to assessing patient needs, incorporating age and disease specific characteristics into drug therapy and patient education, adjusting care according to patient response, and providing clinical interventions to detect, mitigate, and prevent medication adverse events. Clinical Pharmacist Specialists serve as departmental resources and liaisons to other -

Mayo Clinic Alix School of Medicine
Transforming Medical Education through the Science of Health Care Delivery Learning Environment Science of Health Care Delivery Faculty Development Mayo Clinic Alix School of Medicine Consortium projects Curricular Framework Need/Gap Addressed Learning environment Mayo Clinic Alix School of Medicine - ASU framework for the Science of Learning environment Health Care Delivery, longitudinal, four-year medical student curriculum: Brief description: Develop a robust learning environment evaluation A supportive learning environment is critical to achieving desired learning program that incorporates measures relevant to health systems science, outcomes. Existing measures of the learning environment (such as those triangulates feedback from multiple stakeholders, is feasible to track over included in the Association of American Medical Colleges Year Two and time, and enables continuous improvement. Graduation Questionnaires) provide valuable and important data, but incompletely assess aspects of the learning environment relevant to Integration of health systems science into clinical settings SHCD competencies. Furthermore, combining feedback from medical students with the perspectives of other stakeholders may provide valuable Brief description: Develop and pilot new models for integrating health insights and help galvanize improvement efforts. systems science into clinical practice settings to demonstrate the relevance of SHCD to practice, engage students in authentic, workplace- Integration of health systems science into clinical settings based SHCD skill development, and support the development of a team- based, systems-oriented professional identity. This will require faculty Our SHCD curriculum exists in all four years of the Mayo Clinic Alix development to achieve desired student outcomes. School of Medicine (MCASOM) curriculum, but current learning experiences are primarily in non-clinical settings (blended learning with classroom and simulation activities). -

Patient Care Through Telepharmacy September 2016
Patient Care through Telepharmacy September 2016 Gregory Janes Objectives 1. Describe why telepharmacy started and how it has evolved with technology 2. Explain how telepharmacy is being used to provide better patient care, especially in rural areas 3. Understand the current regulatory environment around the US and what states are doing with regulation Agenda ● Origins of Telepharmacy ● Why now? ● Telepharmacy process ● Regulatory environment ● Future Applications Telepharmacy Prescription verification CounselingPrescription & verification Education History Origins of Telepharmacy 1942 Australia’s Royal Flying Doctor Service 2001 U.S. has first state pass telepharmacy regulation 2003 Canada begins first telepharmacy service 2010 Hong Kong sees first videoconferencing consulting services US Telepharmacy Timeline 2001 North Dakota first state to allow 2001 Community Health Association in Spokane, WA launches program 2002 NDSU study begins 2003 Alaska Native Medical Center program 2006 U.S. Navy begins telepharmacy 2012 New generation begins in Iowa Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii NDSU Telepharmacy Study Study from 2002-2008 ● 81 pharmacies ○ 53 retail and 28 hospital ● Rate of dispensing errors <1% ○ Compared to national average of ~2% ● Positive outcomes, mechanisms could be improved Source: The North Dakota Experience: Achieving High-Performance -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

COVID-19 and Your Mental Health Worries and Anxiety About COVID-19 and Its Impact Can Be Overwhelming. Social Distancing Makes I
COVID-19 and your mental health Worries and anxiety about COVID-19 and its impact can be overwhelming. Social distancing makes it even more challenging. Learn ways to cope during this pandemic. By Mayo Clinic Staff The COVID-19 pandemic has likely brought many changes to how you live your life, and with it uncertainty, altered daily routines, financial pressures and social isolation. You may worry about getting sick, how long the pandemic will last and what the future will bring. Information overload, rumors and misinformation can make your life feel out of control and make it unclear what to do. During the COVID-19 pandemic, you may experience stress, anxiety, fear, sadness and loneliness. And mental health disorders, including anxiety and depression, can worsen. Learn self-care strategies and get the care you need to help you cope. Self-care strategies are good for your mental and physical health and can help you take charge of your life. Take care of your body and your mind and connect with others to benefit your mental health. Take care of your body Be mindful about your physical health: Get enough sleep. Go to bed and get up at the same times each day. Stick close to your typical schedule, even if you're staying at home. Participate in regular physical activity. Regular physical activity and exercise can help reduce anxiety and improve mood. Find an activity that includes movement, such as dance or exercise apps. Get outside in an area that makes it easy to maintain distance from people — as recommended by the U.S. -

A Tool to Help Clinicians Do What They Value Most
Health Information Technology: a Tool to Help Clinicians Do What They Value Most Health care professionals like you play a vital role in improving the health outcomes, quality of care, and the health care experience of patients. Health information technology (health IT) is an important tool that you can use to improve clinical practice and the health of your patients. Health IT can help health care professionals to do what you do best: provide excellent care to your patients. Research shows that when patients are Health IT encompasses a wide range of electronic tools that can help you: engaged in their health care, it can lead to • Access up-to-date evidence-based clinical guidelines and decision measurable improvements in safety and support quality. • Improve the quality of care and safety of your patients Source: Agency for Healthcare Research and Quality (AHRQ) • Provide proactive health maintenance for your patients • Better coordinate patients’ care with other providers through the secure and private sharing of clinical information. Health IT can help you to solve clinical problems with real-time data Quality improvement and clinical decision support rely on information about your patient population being readily available in digital form. Health IT can help you monitor your patients’ health status and make specific and targeted recommendations to improve your patients’ health. Access to real-time data through electronic health records and health IT will help you: A MAJORITY OF PROVIDERS • Use clinical decision support to highlight care options tailored to believe that electronic health information your patients has the potential to improve the quality of patient care and care coordination. -

Pharmacist-Physician Team Approach to Medication-Therapy
Pharmacist-Physician Team Approach to Medication-Therapy Management of Hypertension The following is a synopsis of “Primary-Care-Based, Pharmacist-Physician Collaborative Medication-Therapy Management of Hypertension: A Randomized, Pragmatic Trial,” published online in June 2014 in Clinical Therapeutics. What is already known on this topic? found that the role of the pharmacist differed within each study; whereas some pharmacists independently initiated and High blood pressure, also known as hypertension, is a changed medication therapy, others recommended changes major risk factor for cardiovascular disease, the leading to physicians. Pharmacists were already involved in care in all cause of death for U.S. adults. Helping patients achieve but one study. blood pressure control can be difficult for some primary care providers (PCPs), and this challenge may increase with After reviewing the RCTs, the authors conducted a randomized the predicted shortage of PCPs in the United States by 2015. pragmatic trial to investigate the processes and outcomes that The potential shortage presents an opportunity to expand result from integrating a pharmacist-physician team model. the capacity of primary care through pharmacist-physician Participants were randomly selected to receive PharmD-PCP collaboration for medication-therapy management (MTM). MTM or usual care from their PCPs. The authors conducted MTM performed through a collaborative practice agreement the trial within a university-based internal medicine medical allows pharmacists to initiate and change medications. group where the collaborative PharmD-PCP MTM team Researchers have found positive outcomes associated included an internal medicine physician and two clinical with having a pharmacist on the care team; however, the pharmacists, both with a Doctor of Pharmacy degree, at least evidence is limited to only a few randomized controlled 1 year of pharmacy practice residency training, and more than trials (RCTs). -

Hospital Clinic Visits by Cindy C
PROFESSIONAL OPPORTUNITIES PROFESSIONAL OPPORTUNITY | Billing and Coding | T Hospital Clinic Visits by Cindy C. Parman,T CPC, CPC-H, RCC hen a physician performs a three years prior to the current visit, be based on hospital facil- patient visit in an office or or an established patient visit (codes ity resources. The guidelines Wfreestanding center where 99211-99215) for an individual who should not be based on physician the doctor ownsACCC and/or rents the has been registered as an inpatient or resources (67 FR 66792). space, employsMember and/or contracts with outpatient within the past three years. 3. The coding guidelines should Pall staff,R andO bears allF operatingILE costs, According to the Medicare be clear to facilitate accurate payers make a single payment for Claims Processing Manual, Chapter payments and be usable for this encounter. This physician pay- 2: “The term ‘encounter’ means a compliance purposes and audits ment includes both the professional direct personal contact in the hos- (67 FR 66792). service and the technical service (in pital between a patient and a physi- 4. The coding guidelines should other words, the practice expenseACCC cian, or other person who is autho- meet the HIPAA requirements component). When the patient visit is rized by State law and, if applicable, (67 FR 66792). AperformedC in theT hospitalI ONoutpatient by hospital staff bylaws to order 5. The coding guidelines should department setting, however, the phy- or furnish services for diagnosis or only require documentation that sician bills and receives reimbursement treatment of the patient…When a is clinically necessary for patient for only the professional service. -

Chapter 54 Manual of Requirements for Family Child Care Registration
CHAPTER 54 MANUAL OF REQUIREMENTS FOR FAMILY CHILD CARE REGISTRATION STATE OF NEW JERSEY DEPARTMENT OF CHILDREN AND FAMILIES EFFECTIVE - March 20, 2017 EXPIRES - February 21, 2024 DEPARTMENT OF CHILDREN AND FAMILIES OFFICE OF LICENSING PO BOX 717 TRENTON, NEW JERSEY 08625-0717 Toll - Free Telephone 1-877-667-9845 N.J.A.C. 3A:54 MANUAL OF REQUIREMENTS FOR FAMILY CHILD CARE REGISTRATION SUBCHAPTER 1. GENERAL PROVISIONS................................................................................ 1 3A:54-1.1 Legal authority ................................................................................................................ 1 3A:54-1.2 Definitions ....................................................................................................................... 2 3A:54-1.3 Approval requirements for sponsoring organizations ..................................................... 4 3A:54-1.4 Public access to records ................................................................................................... 6 SUBCHAPTER 2. ADMINISTRATION OF SPONSORING ORGANIZATIONS ................... 8 3A:54-2.1 Sponsoring organization eligibility ................................................................................. 8 3A:54-2.2 Administrative responsibility .......................................................................................... 8 3A:54-2.3 Reporting requirements ................................................................................................... 9 3A:54-2.4 Sponsoring organization records