1 Nhs Leeds West Ccg Financial Due Diligence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Notices and Proceedings for the North East of England 2454
Office of the Traffic Commissioner (North East of England) Notices and Proceedings Publication Number: 2454 Publication Date: 18/12/2020 Objection Deadline Date: 08/01/2021 Correspondence should be addressed to: Office of the Traffic Commissioner (North East of England) Hillcrest House 386 Harehills Lane Leeds LS9 6NF Telephone: 0300 123 9000 Website: www.gov.uk/traffic-commissioners The next edition of Notices and Proceedings will be published on: 18/12/2020 Publication Price £3.50 (post free) This publication can be viewed by visiting our website at the above address. It is also available, free of charge, via e-mail. To use this service please send an e-mail with your details to: [email protected] Remember to keep your bus registrations up to date - check yours on https://www.gov.uk/manage-commercial-vehicle-operator-licence-online PLEASE NOTE THE PUBLIC COUNTER IS CLOSED AND TELEPHONE CALLS WILL NO LONGER BE TAKEN AT HILLCREST HOUSE UNTIL FURTHER NOTICE The Office of the Traffic Commissioner is currently running an adapted service as all staff are currently working from home in line with Government guidance on Coronavirus (COVID-19). Most correspondence from the Office of the Traffic Commissioner will now be sent to you by email. There will be a reduction and possible delays on correspondence sent by post. The best way to reach us at the moment is digitally. Please upload documents through your VOL user account or email us. There may be delays if you send correspondence to us by post. At the moment we cannot be reached by phone. -

The Following PRISONERS, Whose Estates and Effects Have Been Vested in the Provisions Assignee by Order of the Court, Having
The following PRISONERS, whose Estates and George Marscten, formerly of Kirk gate. Wakefield, York- Effects have been vested in the Provisions shire, Joiner and Carpenter, afterwards of East-moor, Stanley, near Wakefield, Cow Keeper, Joiner, and Car- Assignee by Order of the Court, having filec penter, then of Armitage-yard, and late of Tavern- their Schedules, are ordered to be brought up street, Primrose-hill, all in Wakefield, Joiner and Car- before a Commissioner on Circuit, to be dealt penter. with according to the Statute, as follows: Adjourned. Robert Overend, late of Scholes, near Halifax, Yorkshire' Wire Drawer and Card Maker, partner with Robert At the Court-House, at Wakefield, in the Comity Overend, late of the ssmc place, deceased, and latterly of York, on the 14th day of February 1843, •with Hannah Ovcrcnd, of the same place, Wire Drawer at Ten o'Clock in the Forenoon precisely. and Card Maker, acting as Manager of the said several businesses for the said Hannah Overend. John Holroyd, formerly of Giggleswick, near Settle, York- shire, Wine and Spirit Merchant, afterwards of Settle, At the Court-Honse, at "Wakefield, in the County "Wine and Spirit Merchant, and late of Giggleswick of York, on the 15th day of February 1843, afc aforesaid, out of business. Ten o'Clock in the Forenoon precisely. George Woodcock, late of Granville-street, Sheffield-park, Yorkshire, out of business, previously of No. 7, East- George Johnson, formerly of Old Infirmary-yard, Kirkgate, street, Sheffield-park aforesaid, and formerly of New-street, Leeds, Fruiterer and Herring Merchant, then a Prisoner Sheffield-park, Journeyman Brush Maker and Retailer of in York Cast'.e, then of the same place and trades, then Beer. -

56 Bus Time Schedule & Line Route
56 bus time schedule & line map 56 Moor Grange <-> Leeds City Centre View In Website Mode The 56 bus line (Moor Grange <-> Leeds City Centre) has 5 routes. For regular weekdays, their operation hours are: (1) Moor Grange <-> Leeds City Centre: 7:30 PM - 11:10 PM (2) Moor Grange <-> Whinmoor: 5:15 AM - 10:40 PM (3) Swarcliffe <-> Moor Grange: 5:07 AM (4) Whinmoor <-> Leeds City Centre: 11:10 PM - 11:40 PM (5) Whinmoor <-> Moor Grange: 5:15 AM - 10:40 PM Use the Moovit App to ƒnd the closest 56 bus station near you and ƒnd out when is the next 56 bus arriving. Direction: Moor Grange <-> Leeds City Centre 56 bus Time Schedule 26 stops Moor Grange <-> Leeds City Centre Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:30 PM - 11:10 PM Latchmere Drive, Moor Grange Latchmere Green, Leeds Tuesday 7:30 PM - 11:10 PM Latchmere Road, Moor Grange Wednesday 7:30 PM - 11:10 PM Old Farm Approach, Moor Grange Thursday 7:30 PM - 11:10 PM Friday 7:30 PM - 11:10 PM Old Oak Drive, West Park Old Oak Garth, Leeds Saturday 11:10 PM Beckett Park, West Park Ghyll Road, West Park 56 bus Info Woodbridge Crescent, Beckett Park Direction: Moor Grange <-> Leeds City Centre Stops: 26 Woodbridge Place, Beckett Park Trip Duration: 22 min Queenswood Drive, Leeds Line Summary: Latchmere Drive, Moor Grange, Latchmere Road, Moor Grange, Old Farm Approach, Queenswood Road, Beckett Park Moor Grange, Old Oak Drive, West Park, Beckett Jaques Close, Leeds Park, West Park, Ghyll Road, West Park, Woodbridge Crescent, Beckett Park, Woodbridge Place, Beckett Eden -
The State of Men's Health in Leeds
The State of Men’s Health in Leeds: Data Dr. Amanda Seims, Leeds Beckett University Professor Alan White, Leeds Beckett University 1 2 To reference this document: Seims A. and White A. (2016) The State of Men’s Health in Leeds: Data Report. Leeds: Leeds Beckett University and Leeds City Council. ISBN: 978-1-907240-64-5 This study was funded by Leeds City Council Acknowledgements We would like to thank the following individuals for their input and feedback and also for their commitment to men’s health in Leeds: Tim Taylor and Kathryn Jeffries Dr Ian Cameron DPH and Cllr Lisa Mulherin James Womack and Richard Dixon - Leeds Public Health intelligence team 1 Contents Acknowledgements ........................................................................................................................... 1 1 Introduction and data analyses .................................................................................................. 9 1.1 Analysis of routinely collected health, socio-economic and service use data ............................. 9 2 The demographic profile of men in Leeds ................................................................................. 10 2.1 The male population ................................................................................................................... 10 2.2 Population change for Leeds ...................................................................................................... 11 2.3 Ethnic minority men in Leeds .................................................................................................... -

Coal Mining in Morley
BRITISH MINING No.87 COAL MINING IN MORLEY by JIM THORP O.B.E. MONOGRAPH OF THE NORTHERN MINE RESEARCH SOCIETY JUNE 2009 CONTENTS List of illustrations 4 Acknowledgements 5 Introduction 6 Not just a textile history 8 Rich coal seams 11 The Royal Commission for Women and Children 14 The Act - an inspector calls 18 The Act - the inspection 22 Morley Main and William Best 25 The Morley Main explosion 31 The inquest - identification 36 The inquest – evidence 39 The inquest – the professionals 44 Relief 47 More disasters 52 A heavy price 57 The pits go to law 62 Topcliffe and the Iron Man 67 Topcliffe and town gas 71 Pitmen- the owners 74 Pitmen - the miners 78 Disputes 81 Touching on finance 86 The end of the line 89 Appendix 1 - Lists of fatalities in major pit disasters 91 Appendix 2 - Frank Newby Wardell 92 Appendix 3 - Collieries and archival sources 93 Appendix 4 - mining geology of the Morley coalfield 96 Bibliography and sources of information 99 Index 102 LIST OF ILLUSTRATIONS Page Frontispiece Morley coat of arms 5 Figure 1. Map showing the position of Morley within the W. Riding of Yorkshire 7 Figure 2. Undated photograph of Queen Street Morley and the Town Hall 10 Figure 3. Collieries in the Morley area 12 Figure 4. Coal cutting from the 1842 Children’s Employment Commission 15 Figure 5. Howley Park Colliery and the drawing shaft from the Middleton Seam 17 Figure 6. Hauling coal underground from the 1842 Children’s Employment Commission 19 Figure 7. Howley Park Colliery and the drawing shaft for the Silkstone Seam 21 Figure 8 The Plate Road, Morley, May 1960 23 Figure 9. -

Download Original Attachment
Building Name Address 1 Address 2 Address 3 Address 4 Address 5 Postcode Building Use Tenure Type Airedale House Airedale House Royd Ings Avenue KEIGHLEY West Yorkshire BD21 4BZ Police Station Freehold Denholme Contact Point, Mechanics Inst Denholme Contact Point Mechanics Institute, Main Street Denholme BRADFORD West Yorkshire BD13 4BL Contact Point Leasehold Dudley Hill Centre Dudley Hill Centre Harry Street BRADFORD West Yorkshire BD4 9PH Support Office Freehold Eccleshill Police Station Eccleshill Police Station Javelin House Javelin Close BRADFORD West Yorkshire BD10 8SD Police Station Freehold Haworth Contact Point Haworth Contact Point 28 Changegate Haworth BRADFORD West Yorkshire BD22 8DY Contact Point Freehold Ilkley Police Station Ilkley Police Station Riddings Road ILKLEY West Yorkshire LS29 9LU Police Station Freehold New Park Road 24A New Park Road Queensbury BRADFORD West Yorkshire BD13 2EU Neighbourhood Policing Freehold Shipley Police Station Shipley Police Station Manor Lane SHIPLEY West Yorkshire BD18 3RJ Police Station Freehold Toller Lane Police Station Toller Lane Police Station Lawcroft House, Toller Lane Lillycroft Road BRADFORD West Yorkshire BD9 5AF Police Station Freehold Trafalgar House Trafalgar House Nelson Street BRADFORD West Yorkshire BD5 0EW Police Station Freehold Brighouse Police Station Brighouse Police Station Bradford Road BRIGHOUSE West Yorkshire HD6 4AA Police Station Freehold Halifax Police Station Halifax Police Station Richmond Close HALIFAX West Yorkshire HX1 5TW Police Station Freehold Todmorden -

Proposed Site Allocations in New Farnley
Issue 12 Spring 2014 Proposed Site Allocations In New Farnley roposed Land Development on that the Village Design Statement Pfields between Castle Ings Gar - Document had not been consulted. dens and Low Moor Side effecting As a result of the complaint, the properties that back onto this field group were invited to give a speech which include Walsh Lane, Whitehall about their concerns, at a full Road and the surrounding areas of council meeting which consisted of the New Farnley Village. 99 local ward concillors and chaired In June 2013 a number of resi - by the Lord Mayor of Leeds. dents living adjacent to the pro - A deputation held at the Civic Hall posed sites received letters on Wednesday 15th January 2014 informing them about the propos - attended by members of the NFVG als, various members of the Vision at Leonardo Buildings and obtained including the Chairperson Steve Group had been contacted by resi - all the appropriate booklets etc Fletcher, Secretary Christine Ed - dents enquiring if we had any addi - about the “proposed site alloca - munds, Treasurer Jenny Jamieson tional information. Due to the tions” and Project Co-ordinator Maggie recent approval and adoption in Numerous copies of the booklets Thompson. April 2013 of “The New Farnley De - and comment slips for residents to Maggie Thompson read out the sign Statement” which is part of the put their views forward were dis - speech which had been prepared Leeds Local Development Frame - tributed around the village and at earlier by the group expressing work and is a Statutory Develop - strategic points including the Com - serious concerns about the ment Plan for the area and therefore munity Centre, local GP surgeries St appalling consultation process. -

Internal Memo
Leeds Admission Policy 2019/20 Primary phase The admissions policy for Leeds community and voluntary-controlled schools for entry to Primary phase (Reception) in September 2019 The Chief Executive of Leeds City Council makes all offers of a school place for Reception places as Leeds City Council is the admissions authority for these schools. Headteachers or school-based staff are not authorised to offer a child a place for Reception for September entry. The authority to convey the offer of a place has been delegated to schools for places in other year groups and for entry to Reception outside the normal admissions round. A list of the Community and Voluntary Controlled schools where this admission policy applies is provided in Annex A. This also includes the number of places available in each school for September 2019 entry. Children with an education, health and care plan will be admitted to the school named on their plan. Where there are fewer applicants than places available, all applicants will be offered a place. Where there are more applicants than places available, we will offer places to children in the following order of priority. Priority 1 a) Children in public care or fostered under an arrangement made by the local authority or children previously looked after by a Local Authority. (see note 2) b) Pupils without an EHC plan but who have Special Educational Needs, or with exceptional medical or mobility needs, that can only be met at a specific school. (See note 3) Priority 2 Children with older brothers or sisters who will be at school at the start of the academic year and are living at the same address (see note 4). -

WEST YORKSHIRE Extracted from the Database of the Milestone Society a Photograph Exists for Milestones Listed Below but Would Benefit from Updating!
WEST YORKSHIRE Extracted from the database of the Milestone Society A photograph exists for milestones listed below but would benefit from updating! National ID Grid Reference Road No. Parish Location Position YW_ADBL01 SE 0600 4933 A6034 ADDINGHAM Silsden Rd, S of Addingham above EP149, just below small single storey barn at bus stop nr entrance to Cringles Park Home YW_ADBL02 SE 0494 4830 A6034 SILSDEN Bolton Rd; N of Silsden Estate YW_ADBL03 SE 0455 4680 A6034 SILSDEN Bolton Rd; Silsden just below 7% steep hill sign YW_ADBL04 SE 0388 4538 A6034 SILSDEN Keighley Rd; S of Silsden on pavement, 100m south of town sign YW_BAIK03 SE 0811 5010 B6160 ADDINGHAM Addingham opp. Bark La in narrow verge, under hedge on brow of hill in wall by Princefield Nurseries opp St Michaels YW_BFHA04 SE 1310 2905 A6036 SHELF Carr House Rd;Buttershaw Church YW_BFHA05 SE 1195 2795 A6036 BRIGHOUSE Halifax Rd, just north of jct with A644 at Stone Chair on pavement at little layby, just before 30 sign YW_BFHA06 SE 1145 2650 A6036 NORTHOWRAM Bradford Rd, Northowram in very high stone wall behind LP39 YW_BFHG01 SE 1708 3434 A658 BRADFORD Otley Rd; nr Peel Park, opp. Cliffe Rd nr bus stop, on bend in Rd YW_BFHG02 SE 1815 3519 A658 BRADFORD Harrogate Rd, nr Silwood Drive on verge opp parade of shops Harrogate Rd; north of Park Rd, nr wall round playing YW_BFHG03 SE 1889 3650 A658 BRADFORD field near bus stop & pedestrian controlled crossing YW_BFHG06 SE 212 403 B6152 RAWDON Harrogate Rd, Rawdon about 200m NE of Stone Trough Inn Victoria Avenue; TI north of tunnel -

Notices and Proceedings for the North East of England 2469
Office of the Traffic Commissioner (North East of England) Notices and Proceedings Publication Number: 2469 Publication Date: 02/04/2021 Objection Deadline Date: 23/04/2021 Correspondence should be addressed to: Office of the Traffic Commissioner (North East of England) Hillcrest House 386 Harehills Lane Leeds LS9 6NF Telephone: 0300 123 9000 Website: www.gov.uk/traffic-commissioners The next edition of Notices and Proceedings will be published on: 02/04/2021 Publication Price £3.50 (post free) This publication can be viewed by visiting our website at the above address. It is also available, free of charge, via e-mail. To use this service please send an e-mail with your details to: [email protected] Remember to keep your bus registrations up to date - check yours on https://www.gov.uk/manage-commercial-vehicle-operator-licence-online PLEASE NOTE THE PUBLIC COUNTER IS CLOSED AND TELEPHONE CALLS WILL NO LONGER BE TAKEN AT HILLCREST HOUSE UNTIL FURTHER NOTICE The Office of the Traffic Commissioner is currently running an adapted service as all staff are currently working from home in line with Government guidance on Coronavirus (COVID-19). Most correspondence from the Office of the Traffic Commissioner will now be sent to you by email. There will be a reduction and possible delays on correspondence sent by post. The best way to reach us at the moment is digitally. Please upload documents through your VOL user account or email us. There may be delays if you send correspondence to us by post. At the moment we cannot be reached by phone. -

Temple Newsham Leeds 1 1405 M1 North At
LOC LOC STREET LOC TOWN STREET 1/ (NORTH BOUND) TEMPLE NEWSHAM LEEDS 1 1405 M1 NORTH AT TEMPLE NEWSAM 1 1650 A1 (M) NORTH PARRLINGTON 1 2055 DENBY DALE ROAD WAKEFIELD 1 A 1 SELBY FORK SELBY 1 A1 PONTEFRACT 1 SELBY FORK 1 A1 (M) DARRINGTON PONTEFRACT 1 A1 (M) DARRINGTON N/B TURN GATE PONTEFRACT 1 A1 (M) FERRYBRIDGE PONTEFRACT 2 A1 (M) FERRYBRIDGE N/B PONTEFRACT 1 A1 (M) FERRYBRIDGE WEST BOUND PONTEFRACT 1 A1 (m) HOLMFIELD INTERCHANGE PONTEFRACT 2 A1 (M) NBC ABERFORD LEEDS 1 A1 (M) NORTH FERRYBRIDGE 1 A1 (M) NORTH AT BRAMHAM LEEDS 1 A1 (M) NORTH AT FERRYBRIDGE PONTEFRACT 2 A1 (M) NORTH AT PARRINGTON PONTEFRACT 1 A1 (M) NORTH AT PARRLINGTON PONTEFRACT 1 A1 (M) NORTH BOUND DARRINGTON PONTEFRACT 1 A1 (M) NORTH BOUND FERRYBRIDGE PONTEFRACT 2 A1 (M) NORTH FERRYBRIDGE PONTEFRACT 2 A1 (M) NORTH HOLMFIELD KNOTTINGLEY 1 A1 (M) NORTH HOOK MOOR LEEDS 1 A1 (M) NORTH, DARRINGTON PONTEFRACT 1 A1 (m) NORTHBOUND HOLMFIELD, KNOTTINGLEY 1 A1 (m) S/B HOOK MOOR 2 A1 (M) SOURTH AT SELBY FORK SELBY 1 A1 (M) SOUTH ABERFORD 1 A1 (M) SOUTH AT DARRINGTON PONTEFRACT 1 A1 (M) SOUTH AT MICKLEFIELD SELBY 1 A1 (M) SOUTH BOUND FERRYBRIDGE PONTEFRACT 1 A1 (M) SOUTH FERRYBRIDGE PONTEFRACT 1 A1 (M) SOUTH MICKLEFIELD SELBY 1 A1 (M) SOUTH PARRLINGTON 1 A1 (M) SOUTHBOUND HOOKMOOR 1 LEEDS 1 A1 (M) SOUTHBOUND LEDSHAM LEEDS 1 A1 AT HILME PONTEFRACT 1 A1 BRAMHAM WETHERBY 1 A1 FERRYBRIDGE PONTEFRACT 1 A1 FRYSTON PARK PONTEFRACT 1 A1 M LEEDS 1 PONTEFRACT 1 A1 M SOUTH FERRY BRIDGE WAKEFIELD 1 A1 M DARRINGTON PONTEFRACT 1 A1 M FERRYBRIDGE PONTEFRACT 1 A1 M FERRYBRIDGE NORTH PONTEFRACT -
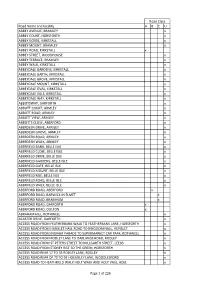
Road Name and Locality a B C U ABBEY AVENUE, BRAMLEY X
Road Class Road Name and locality A BCU ABBEY AVENUE, BRAMLEY x ABBEY COURT, HORSFORTH x ABBEY GORSE, KIRKSTALL x ABBEY MOUNT, BRAMLEY x ABBEY ROAD, KIRKSTALL x ABBEY STREET, WOODHOUSE x ABBEY TERRACE, BRAMLEY x ABBEY WALK, KIRKSTALL x ABBEYDALE GARDENS, KIRKSTALL x ABBEYDALE GARTH, KIRKSTALL x ABBEYDALE GROVE, KIRKSTALL x ABBEYDALE MOUNT, KIRKSTALL x ABBEYDALE OVAL, KIRKSTALL x ABBEYDALE VALE, KIRKSTALL x ABBEYDALE WAY, KIRKSTALL x ABBOTSWAY, GARFORTH x ABBOTT COURT, ARMLEY x ABBOTT ROAD, ARMLEY x ABBOTT VIEW, ARMLEY x ABBOTTS CLOSE, ABERFORD x ABERDEEN DRIVE, ARMLEY x ABERDEEN GROVE, ARMLEY x ABERDEEN ROAD, ARMLEY x ABERDEEN WALK, ARMLEY x ABERFIELD BANK, BELLE ISLE x ABERFIELD CLOSE, BELLE ISLE x ABERFIELD DRIVE, BELLE ISLE x ABERFIELD GARDENS, BELLE ISLE x ABERFIELD GATE, BELLE ISLE x ABERFIELD MOUNT, BELLE ISLE x ABERFIELD RISE, BELLE ISLE x ABERFIELD ROAD, BELLE ISLE x ABERFIELD WALK, BELLE ISLE x ABERFORD ROAD, ABERFORD x ABERFORD ROAD, BARWICK IN ELMET x ABERFORD ROAD, BRAMHAM x ABERFORD ROAD, GARFORTH x ABERFORD ROAD, OULTON x ABRAHAM HILL, ROTHWELL x ACASTER DRIVE, GARFORTH x ACCESS ROAD FROM FEATHERBANK WALK TO FEATHERBANK LANE, HORSFORTH x ACCESS ROAD FROM HUNSLET HALL ROAD TO KINGDOM HALL, HUNSLET x ACCESS ROAD FROM INGRAM PARADE TO SUPERMARKET CAR PARK, ROTHWELL x ACCESS ROAD FROM RODLEY LANE TO OAKLANDS ROAD, RODLEY x ACCESS ROAD FROM ST PETERS STREET TO MILLGARTH STREET, LEEDS x ACCESS ROAD FROM STONEY RISE TO THE GREEN, HORSFORTH x ACCESS ROAD REAR 17 TO 33 RODLEY LANE, RODLEY x ACCESS ROAD REAR OF 70 TO 92 HOLMSLEY LANE,