Antimicrobial and Chemical Analyses of Selected Bulbine Species
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Traditional Information and Antibacterial Activity of Four Bulbine Species (Wolf)
African Journal of Biotechnology Vol. 10 (2), pp. 220-224, 10 January, 2011 Available online at http://www.academicjournals.org/AJB DOI: 10.5897/AJB10.1435 ISSN 1684–5315 © 2011 Academic Journals Full Length Research Paper Traditional information and antibacterial activity of four Bulbine species (Wolf) R. M. Coopoosamy Department of Nature Conservation, Mangosuthu University of Technology, P O Box 12363, Jacobs4026, Durban, KwaZulu-Natal, South Africa. E-mail: [email protected]. Tel: +27 82 200 3342. Fax: +27 31 907 7665. Accepted 7 December, 2010 Ethnobotanical survey of Bulbine Wolf, (Asphodelaceae) used for various treatment, such as, diarrhea, burns, rashes, blisters and insect bites, was carried out in the Eastern Cape Province of South Africa. Information on the parts used and the methods of preparation was collected through questionnaire which was administered to the herbalists, traditional healers and rural dwellers which indicated the extensive use of Bulbine species. Most uses of Bulbine species closely resemble that of Aloe . Dried leaf bases and leaf sap are the commonest parts of the plants used. Preparations were in the form of decoctions and infusions. Bulbine frutescens was the most frequently and commonly used of the species collected for the treatment of diarrhoea, burns, rashes, blisters, insect bites, cracked lips and mouth ulcers. The leaf, root and rhizome extracts of B. frutescens, Bulbine natalensis, Bulbine latifolia and Bulbine narcissifolia were screened for antibacterial activities to verify their use by traditional healers. Key words: Herbal medicine, diarrhea, medicinal plants, Bulbine species, antibacterial activity. INTRODUCTION Many traditionally used plants are currently being investi- developing countries where traditional medicine plays a gated for various medicinal ailments such as treatment to major role in health care (Farnsworth, 1994; Srivastava et cure stomach aliments, bolding, headaches and many al., 1996). -

Ultrastructural Micromorphology of Bulbine Abyssinica A
Pak. J. Bot., 47(5): 1929-1935, 2015. ULTRASTRUCTURAL MICROMORPHOLOGY OF BULBINE ABYSSINICA A. RICH. GROWING IN THE EASTERN CAPE PROVINCE, SOUTH AFRICA CROMWELL MWITI KIBITI AND ANTHONY JIDE AFOLAYAN* Medicinal Plants and Economic Development Research Centre (MPED), Department of Botany, University of Fort Hare, Alice, 5700, South Africa Corresponding author e-mail: [email protected]; Phone: +27 82 202 2167; Fax: +27 866 282 295 Abstract The genus Bulbine (Asphodelaceae) comprises about 40 species in South Africa. Bulbine abyssinica is a succulent member of the genus that occurs from the Eastern Cape, through Swaziland, Lesotho, and further north to Ethiopia. The species is often used in traditional medicine to treat rheumatism dysentery, bilharzia and diabetes. Inspite of its ethno medicinal value, not much data concerning the micro-morphological features is available in literature. The present study was undertaken to examine the ultra-morphological features of the leaf, stem and root of the plant using light and scanning electron microscopes and the elemental composition. The elemental compositions of the plant parts were done using energy dispersive x- ray spectroscopy. The mean length and width of the guard cells in the abaxial surface are 0.15 ± 0.002 mm and 0.14 ± 0.002 mm, respectively while those of the adaxial surface are 0.14 ± 0.001 mm and 0.12 ± 0.001 mm, respectively. The electron microscopy revealed the presence of crystals in the leaves, stems and roots. The EDXS microanalysis of the crystals revealed the presence of sodium, silicon, potassium and calcium as the major constituents. The leaf also showed the presence of iron and magnesium, while the stem had aluminium, phosphorous and magnesium. -

Bulbinella Rossii
Bulbinella rossii COMMON NAME Ross Lily SYNONYMS Chrysobactron rossii Hook.f.; Anthericum rossii (Hook.f.) Hook.f. FAMILY Asphodelaceae AUTHORITY Bulbinella rossii (Hook.f.) Cheeseman FLORA CATEGORY Vascular – Native ENDEMIC TAXON Yes ENDEMIC GENUS Enderby Island. Photographer: Jane Gosden No ENDEMIC FAMILY No STRUCTURAL CLASS Herbs - Monocots NVS CODE BULROS CHROMOSOME NUMBER Sub Antarctic Islands. Photographer: Chris 2n = 14 Rance CURRENT CONSERVATION STATUS 2012 | At Risk – Naturally Uncommon | Qualifiers: RR PREVIOUS CONSERVATION STATUSES 2009 | At Risk – Naturally Uncommon 2004 | Range Restricted DISTRIBUTION Endemic. Auckland and Campbell Islands HABITAT Widespread and common from sea level to the tops of island ranges. Flourishes in disturbed sites, and so common near old habitations and because it is not especially palatable, where browsing animals congregate. prefers open herbfield and tussock grassland, where it may form dense colonies. FEATURES Dioecious, stout, perennial lily up to 1 m tall and 40 mm diameter at the base. Leaves fleshy, 0.6-1m x 15-60 mm wide, dark green, obtuse to subacute, apices recurved, nerves faint to prominent, easily felt when fresh. Peduncle up to 10 mm diameter, usually < leaf length. Inflorescence a cylindric raceme up to 150 x 600 mm; bracts and pedicels of almost equal length in female flowers and conspicuous in bud; in males < pedicels and inconspicuous in bud; pedicels 10-20 mm long, swollen just below flower. Flowers numerous, densely crowded, 10-14 mm diameter, golden yellow to sulphur yellow, often faintly tinged with orange; tepals oblong-ovate, spreading in males in females erect and remaining so, usually hardening as fruit ripens. Stamens < tepals; anthers in males conspicuously filled with pollen, in females rudimentary. -

A Fine-Scale Conservation Plan for Cape Lowlands Renosterveld: Technical Report
A Fine-Scale Conservation Plan for Cape Lowlands Renosterveld: Technical Report MAIN REPORT September 2003 Amrei von Hase Mathieu Rouget Kristal Maze Nick Helme Report No. CCU 2/03 Cape Conservation Unit Botanical Society of South Africa Pvt Bag X 10 7735 Claremont www.botanicalsociety.org.za/ccu Key Partners and Sponsors of the Cape Lowlands Renosterveld Project TABLE MOUNTAIN FUND 2 Acknowledgements Many individuals and organizations have contributed generously to the Cape Lowlands Renosterveld Project to whom the Botanical Society and the project team are greatly indebted. We express our appreciation to you in this section and in addition have provided acknowledgement to others in sections of this report where their contribution was relevant. We are particularly indebted to our key project partners, the Western Cape Nature Conservation Board (WCNCB), for putting their full support behind the project from its inception as well as their many contributions to the project. In Scientific Services we especially thank the late Chris Burgers, Helen de Klerk, Ernst Baard, Annelise le Roux, Guy Palmer and Andrew Turner for their guidance in the project planning and initiation stages, particularly on data and GIS matters. We are tremendously grateful to Chris who generously and infectiously shared with us his wealth of knowledge about the lowlands. In Operations we express our appreciation to the business unit managers, extension officers and regional ecologists who played a vital role particularly in shaping the final products of the project. We are especially grateful to Anton Wolfaardt and Chris Martens. Wendy Paisley of the Cape Conservation Unit (CCU) of the Botanical Society provided invaluable administrative and organizational support to the project. -

Eutaxia Microphylla Common Eutaxia Dillwynia Hispida Red Parrot-Pea Peas FABACEAE: FABOIDEAE Peas FABACEAE: FABOIDEAE LEGUMINOSAE LEGUMINOSAE
TABLE OF CONTENTS Foreword iv printng informaton Acknowledgements vi Introducton 2 Using the Book 3 Scope 4 Focus Area Reserve Locatons 5 Ground Dwellers 7 Creepers And Twiners 129 Small Shrubs 143 Medium Shrubs 179 Large Shrubs 218 Trees 238 Water Lovers 257 Grasses 273 Appendix A 290 Appendix B 293 Resources 300 Glossary 301 Index 303 ii iii Ground Dwellers Ground dwellers usually have a non-woody stem with most of the plant at ground level They sometmes have a die back period over summer or are annuals They are usually less than 1 metre high, provide habitat and play an important role in preventng soil erosion Goodenia blackiana, Kennedia prostrata, Glossodia major, Scaevola albida, Arthropodium strictum, Gonocarpus tetragynus Caesia calliantha 4 5 Bulbine bulbosa Bulbine-lily Tricoryne elator Yellow Rush-lily Asphodel Family ASPHODELACEAE Day Lily Family HEMEROCALLIDACEAE LILIACEAE LILIACEAE bul-BINE (bul-BEE-nee) bul-bohs-uh Meaning: Bulbine – bulb, bulbosa – bulbous triek-uhr-IEN-ee ee-LAHT-ee-or Meaning: Tricoryne – three, club shaped, elator – taller General descripton A small perennial lily with smooth bright-green leaves and General descripton Ofen inconspicuous, this erect branched plant has fne, yellow fowers wiry stems and bears small clusters of yellow star-like fowers at the tps Some Specifc features Plants regenerate annually from a tuber to form a tall longish leaves present at the base of the plant and up the stem stem from a base of feshy bright-green Specifc features Six petaled fowers are usually more than 1 cm across, -

Bulbine Bulbosa
Bulbine bulbosa Bulbine bulbosa Botanical Name: Bulbine bulbosa Common Names: Bulbine Lily, Native: Yes Foliage Type: Evergreen Plant Type: Herbs & Vegetables, Palms, Ferns & Tropical Plant Habit: Tufting, Upright Description: Native grass-like perennial shrub with long narrow foliage and small yellow star-like flowers which sit on large spikes throughout spring and summer. Bulbine bulbosa produces edible corms that can be roasted but all other parts of this plant are toxic and should not be eaten. Grows approx 70cm tall x 40cm wide. Great for garden beds or containers. Mature Height: 60cm-1m Position: Full Sun, Semi Shade Mature Width: 30-60cm Soil Type: Well Drained Family Name: Xanthorrhoeaceae Landscape Use(s): Bush Tucker, Edible Garden, Habitat, Low Water Garden, Mass Planting, Rockery, Container / Pot Origin: Australia Characteristics: Pest & Diseases: Generally trouble free Foliage Colours: Green, Grey Flower Colours: Yellow Flower Fragrant: No Cultural Notes: Minimal maintenance required. Prefers water often. Flowering Season: Spring, Summer Fruit: No Plant Care: Requirements: Keep moist during dry periods, Mulch well Growth Rate: Moderate Maintenance Level: Low Water Usage: High Tolerances: Drought: Medium / Moderate Frost: High Wind: High Disclaimer: Information and images provided is to be used as a guide only. While every reasonable effort is made to ensure accuracy and relevancy of all information, any decisions based on this information are the sole responsibility of the viewer. Call 1300 787 401 plantmark.com.au. -

Insights from Microsporogenesis in Asparagales
EVOLUTION & DEVELOPMENT 9:5, 460–471 (2007) Constraints and selection: insights from microsporogenesis in Asparagales Laurent Penet,a,1,Ã Michel Laurin,b Pierre-Henri Gouyon,a,c and Sophie Nadota aLaboratoire Ecologie, Syste´matique et Evolution, Batiment 360, Universite´ Paris-Sud, 91405 Orsay Ce´dex, France bUMR CNRS 7179, Universite´ Paris 6FPierre & Marie Curie, 2 place Jussieu, Case 7077, 75005 Paris, France cMuse´um National d’Histoire Naturelle, De´partement de Syste´matique et Evolution Botanique, 12 rue Buffon, 75005 Paris CP 39, France ÃAuthor for correspondence (email: [email protected]) 1Current address: Department of Biological Sciences, University of Pittsburgh, 4249 Fifth & Ruskin, Pittsburgh, PA 15260, USA. SUMMARY Developmental constraints have been proposed different characteristics of microsporogenesis, only cell to interfere with natural selection in limiting the available wall formation appeared as constrained. We show that set of potential adaptations. Whereas this concept has constraints may also result from biases in the correlated long been debated on theoretical grounds, it has been occurrence of developmental steps (e.g., lack of successive investigated empirically only in a few studies. In this article, cytokinesis when wall formation is centripetal). We document we evaluate the importance of developmental constraints such biases and their potential outcomes, notably the during microsporogenesis (male meiosis in plants), with an establishment of intermediate stages, which allow emphasis on phylogenetic patterns in Asparagales. Different development to bypass such constraints. These insights are developmental constraints were tested by character discussed with regard to potential selection on pollen reshuffling or by simulated distributions. Among the morphology. INTRODUCTION 1991) also hindered tests using the concept (Pigliucci and Kaplan 2000). -

JUDD W.S. Et. Al. (1999) Plant Systematics
CHAPTER8 Phylogenetic Relationships of Angiosperms he angiosperms (or flowering plants) are the dominant group of land Tplants. The monophyly of this group is strongly supported, as dis- cussed in the previous chapter, and these plants are possibly sister (among extant seed plants) to the gnetopsids (Chase et al. 1993; Crane 1985; Donoghue and Doyle 1989; Doyle 1996; Doyle et al. 1994). The angio- sperms have a long fossil record, going back to the upper Jurassic and increasing in abundance as one moves through the Cretaceous (Beck 1973; Sun et al. 1998). The group probably originated during the Jurassic, more than 140 million years ago. Cladistic analyses based on morphology, rRNA, rbcL, and atpB sequences do not support the traditional division of angiosperms into monocots (plants with a single cotyledon, radicle aborting early in growth with the root system adventitious, stems with scattered vascular bundles and usually lacking secondary growth, leaves with parallel venation, flow- ers 3-merous, and pollen grains usually monosulcate) and dicots (plants with two cotyledons, radicle not aborting and giving rise to mature root system, stems with vascular bundles in a ring and often showing sec- ondary growth, leaves with a network of veins forming a pinnate to palmate pattern, flowers 4- or 5-merous, and pollen grains predominantly tricolpate or modifications thereof) (Chase et al. 1993; Doyle 1996; Doyle et al. 1994; Donoghue and Doyle 1989). In all published cladistic analyses the “dicots” form a paraphyletic complex, and features such as two cotyle- dons, a persistent radicle, stems with vascular bundles in a ring, secondary growth, and leaves with net venation are plesiomorphic within angio- sperms; that is, these features evolved earlier in the phylogenetic history of tracheophytes. -

Indigenous Plant Guide
Local Indigenous Nurseries city of casey cardinia shire council city of casey cardinia shire council Bushwalk Native Nursery, Cranbourne South 9782 2986 Cardinia Environment Coalition Community Indigenous Nursery 5941 8446 Please contact Cardinia Shire Council on 1300 787 624 or the Chatfield and Curley, Narre Warren City of Casey on 9705 5200 for further information about indigenous (Appointment only) 0414 412 334 vegetation in these areas, or visit their websites at: Friends of Cranbourne Botanic Gardens www.cardinia.vic.gov.au (Grow to order) 9736 2309 Indigenous www.casey.vic.gov.au Kareelah Bush Nursery, Bittern 5983 0240 Kooweerup Trees and Shrubs 5997 1839 This publication is printed on Monza Recycled paper 115gsm with soy based inks. Maryknoll Indigenous Plant Nursery 5942 8427 Monza has a high 55% recycled fibre content, including 30% pre-consumer and Plant 25% post-consumer waste, 45% (fsc) certified pulp. Monza Recycled is sourced Southern Dandenongs Community Nursery, Belgrave 9754 6962 from sustainable plantation wood and is Elemental Chlorine Free (ecf). Upper Beaconsfield Indigenous Nursery 9707 2415 Guide Zoned Vegetation Maps City of Casey Cardinia Shire Council acknowledgements disclaimer Cardinia Shire Council and the City Although precautions have been of Casey acknowledge the invaluable taken to ensure the accuracy of the contributions of Warren Worboys, the information the publishers, authors Cardinia Environment Coalition, all and printers cannot accept responsi- of the community group members bility for any claim, loss, damage or from both councils, and Council liability arising out of the use of the staff from the City of Casey for their information published. technical knowledge and assistance in producing this guide. -

Networks in a Large-Scale Phylogenetic Analysis: Reconstructing Evolutionary History of Asparagales (Lilianae) Based on Four Plastid Genes
Networks in a Large-Scale Phylogenetic Analysis: Reconstructing Evolutionary History of Asparagales (Lilianae) Based on Four Plastid Genes Shichao Chen1., Dong-Kap Kim2., Mark W. Chase3, Joo-Hwan Kim4* 1 College of Life Science and Technology, Tongji University, Shanghai, China, 2 Division of Forest Resource Conservation, Korea National Arboretum, Pocheon, Gyeonggi- do, Korea, 3 Jodrell Laboratory, Royal Botanic Gardens, Kew, Richmond, United Kingdom, 4 Department of Life Science, Gachon University, Seongnam, Gyeonggi-do, Korea Abstract Phylogenetic analysis aims to produce a bifurcating tree, which disregards conflicting signals and displays only those that are present in a large proportion of the data. However, any character (or tree) conflict in a dataset allows the exploration of support for various evolutionary hypotheses. Although data-display network approaches exist, biologists cannot easily and routinely use them to compute rooted phylogenetic networks on real datasets containing hundreds of taxa. Here, we constructed an original neighbour-net for a large dataset of Asparagales to highlight the aspects of the resulting network that will be important for interpreting phylogeny. The analyses were largely conducted with new data collected for the same loci as in previous studies, but from different species accessions and greater sampling in many cases than in published analyses. The network tree summarised the majority data pattern in the characters of plastid sequences before tree building, which largely confirmed the currently recognised phylogenetic relationships. Most conflicting signals are at the base of each group along the Asparagales backbone, which helps us to establish the expectancy and advance our understanding of some difficult taxa relationships and their phylogeny. -
Bulbinella Modesta
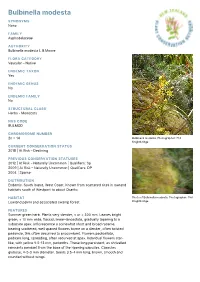
Bulbinella modesta SYNONYMS None FAMILY Asphodelaceae AUTHORITY Bulbinella modesta L.B.Moore FLORA CATEGORY Vascular – Native ENDEMIC TAXON Yes ENDEMIC GENUS No ENDEMIC FAMILY No STRUCTURAL CLASS Herbs - Monocots NVS CODE BULMOD CHROMOSOME NUMBER 2n = 14 Bulbinella modesta. Photographer: Phil Knightbridge CURRENT CONSERVATION STATUS 2018 | At Risk – Declining PREVIOUS CONSERVATION STATUSES 2012 | At Risk – Naturally Uncommon | Qualifiers: Sp 2009 | At Risk – Naturally Uncommon | Qualifiers: DP 2004 | Sparse DISTRIBUTION Endemic. South Island, West Coast. Known from scattered sites in lowland habitats south of Westport to about Okarito. HABITAT Photo of Bulbinella modesta. Photographer: Phil Lowland pakihi and associated swamp forest. Knightbridge FEATURES Summer green herb. Plants very slender, < or = 300 mm. Leaves bright green, < 10 mm wide, flaccid, linear-lanceolate, gradually tapering to a subacute apex. Inflorescence a somewhat short and broad raceme, bearing scattered, well spaced flowers borne on a slender, often twisted peduncle, this often decurved to procumbent. Flowers pedicellate, pedicels long, spreading, often recurved at apex. Individual flowers star- like, with yellow 9.5-13 mm, perianths. These long persistent, as shrivelled remnants pendant from the base of the ripening capsules. Capsules globose, 4-5-5 mm diameter. Seeds 3.5-4 mm long, brown, smooth and rounded without wings. SIMILAR TAXA A rather distinct species unlikely to be confused with any of the other New Zealand Bulbinella species. Perhaps closest to B. talbotii L.B.Moore from which it is easily distinguished by the taller flower head with openly (laxly) arranged flowers. Some people believe it is very close to if not the same as B. hookeri (Hook.) Cheeseman. -

A Biochemical Comparison of the in Vivo Effects of Bulbine Frutescens and Bulbine Natalensis on Cutaneous Wound Healing
Journal of Ethnopharmacology 133 (2011) 364–370 Contents lists available at ScienceDirect Journal of Ethnopharmacology journal homepage: www.elsevier.com/locate/jethpharm A biochemical comparison of the in vivo effects of Bulbine frutescens and Bulbine natalensis on cutaneous wound healing Nalini Pather a,∗, Alvaro M. Viljoen b, Beverley Kramer a a Embryonic Differentiation and Development Research Programme, School of Anatomical Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa b Department of Pharmaceutical Sciences Programme, Tshwane University of Technology, Pretoria, South Africa article info abstract Article history: Aim of the study: In South Africa the local population relies extensively on indigenous plants in the for- Received 28 May 2010 mulation of traditional medicines to treat skin ailments. The scientific merits of many of these plants Received in revised form 1 October 2010 used to treat wounds and burns are yet to be validated. Bulbine natalensis and Bulbine frutescens of the Accepted 4 October 2010 Asphodelaceae family are indigenous to only southern Africa and are widely used as a skin remedy. This Available online 19 October 2010 study aimed to explore the scientific value of these plants through investigating the in vivo biochemical effects of Bulbine natalensis and Bulbine frutescens on cutaneous wounds. Keywords: Material and methods: Excisional and incisional wounds treated with either B. natalensis or B. frutescens Wound healing Bulbine and mirrored control wounds were created on the back of 12 domestic pigs. Wound contraction was Biochemical recorded daily. The excisional wounds, biopsied at days 2, 4, 7, 10 and 16, were used to analyse the Collagen biochemical composition of the wounds by estimating the total amount of protein, DNA, collagen and Hexoamine hexosamine present.