Importance of Geospatial Heterogeneity in Chronic Disease Burden for Policy Planning in an Urban Setting Using a Case Study of Singapore
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of Clinics in Downtown Core Open on Friday 24 Jan 2020
LIST OF CLINICS IN DOWNTOWN CORE OPEN ON FRIDAY 24 JAN 2020 POSTAL S/N NAME OF CLINIC BLOCK STREET NAME LEVEL UNIT BUILDING TEL OPENING HOURS CODE 1 ACUMED MEDICAL GROUP 16 COLLYER QUAY 02 03 INCOME AT RAFFLES 049318 65327766 8.30AM-12.30PM 2 AQUILA MEDICAL 160 ROBINSON ROAD 05 01 SINGAPORE BUSINESS FEDERATION CENTER 068914 69572826 11.00AM- 8.00PM 3 AYE METTA CLINIC PTE. LTD. 111 NORTH BRIDGE ROAD 04 36A PENINSULA PLAZA 179098 63370504 2.30PM-7.00PM 4 CAPITAL MEDICAL CENTRE 111 NORTH BRIDGE ROAD 05 18 PENINSULA PLAZA 179098 63335144 4.00PM-6.30PM 5 CITYHEALTH CLINIC & SURGERY 152 BEACH ROAD 03 08 GATEWAY EAST 189721 62995398 8.30AM-12.00PM 6 CITYMED HEALTH ASSOCIATES PTE LTD 19 KEPPEL RD 01 01 JIT POH BUILDING 089058 62262636 9.00AM-12.30PM 7 CLIFFORD DISPENSARY PTE LTD 77 ROBINSON ROAD 06 02 ROBINSON 77 068896 65350371 9.00AM-1.00PM 8 DA CLINIC @ ANSON 10 ANSON ROAD 01 12 INTERNATIONAL PLAZA 079903 65918668 9.00AM-12.00PM 9 DRS SINGH & PARTNERS, RAFFLES CITY MEDICAL CENTRE 252 NORTH BRIDGE RD 02 16 RAFFLES CITY SHOPPING CENTRE 179103 63388883 9.00AM-12.30PM 10 DRS THOMPSON & THOMSON RADLINK MEDICARE 24 RAFFLES PLACE 02 08 CLIFFORD CENTRE 048621 65325376 8.30AM-12.30PM 11 DRS. BAIN + PARTNERS 1 RAFFLES QUAY 09 03 ONE RAFFLES QUAY - NORTH TOWER 048583 65325522 9.00AM-11.00AM 12 DTAP @ DUO MEDICAL CLINIC 7 FRASER STREET B3 17/18 DUO GALLERIA 189356 69261678 9.00AM-3.00PM 13 DTAP @ RAFFLES PLACE 20 CECIL STREET 02 01 PLUS 049705 69261678 8.00AM-3.00PM 14 FULLERTON HEALTH @ OFC 10 COLLYER QUAY 03 08/09 OCEAN FINANCIAL CENTRE 049315 63333636 -

Statistics Singapore Newsletter, September 2011
The Elderly in Singapore By Miss Wong Yuet Mei and Mr Teo Zhiwei Income, Expenditure and Population Statistics Division Singapore Department of Statistics Introduction Basic profiles such as: • age With better nutrition, advancement • sex in medical science and an increased • type of dwelling awareness of the importance of a • geographical distribution healthy lifestyle, the life expectancy of were compiled using administrative the Singapore resident population has records from multiple sources. improved over the years. Detailed profiles such as: On average, a new-born resident could • marital status expect to live to age 82 years in 2010. • education The life expectancy at birth was lower at • language most frequently spoken 75 years in 1990. at home • living arrangement For the average elderly person in • mobility status Singapore, life expectancy at age 65 • main source of financial support years rose from 16 years in 1990 to 20 years in 2010. Compared to 1990, there were obtained from the Census 2010 are more elderly persons aged 65 years sample enumeration of households staying and over today. in residential housing, and thus excluded those living in institutions such as old This article provides a statistical profile age or nursing homes. The resident of the elderly resident population aged population comprises Singapore citizens 65 years and over in Singapore. and permanent residents. Copyright © Singapore Department of Statistics. All rights reserved. Statistics Singapore Newsletter September 2011 Size of Elderly Resident Geographical Distribution Population Of the 352,600 elderly residents in 2011, Of the 3.79 million Singapore residents 56 per cent were concentrated in ten as at end-June 2011, 352,600 residents planning areas1. -

20130830 Holleczek Etal Digit
! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! This paper might be a pre-copy-editing or a post-print author-produced .pdf of an article accepted for publication. For the definitive publisher-authenticated version, please refer directly to publishing house’s archive system. Digital breadcrumbs: Detecting urban mobility patterns and transport mode choices from cellphone networks Thomas Holleczek, Liang Yu, Joseph K. Lee, Oliver Senn, Kristian Kloeckl, Carlo Ratti, Patrick Jaillet September 2, 2013 Many modern and growing cities are facing declines in public transport usage, with few efficient methods to explain why. In this article, we show that urban mobility patterns and transport mode choices can be derived from cellphone call detail records coupled with public transport data recorded from smart cards. Specifically, we present new data mining approaches to determine the spatial and temporal variability of public and private transportation usage and transport mode preferences across Singapore. Our results, which were validated by Singapore’s quadriennial Household Interview Travel Survey (HITS), revealed that there are 3.5 (HITS: 3.5 million) million and 4.3 (HITS: 4.4 million) million inter-district passengers by public and private transport, respectively. Along with classifying which transportation connections are weak or underserved, the analysis shows that the mode share of public transport use increases from 38 % in the morning to 44 % around mid-day and 52 % in the evening. 1Introduction Securing public transportation ridership is critical for developing a sustainable urban future. However, existing systems for analyzing and identifying weaknesses in public transport connec- tions face major limitations. In cities, origin-destination (OD) matrices—which measure the flow of people between di↵erent geographical regions—are often generated using household surveys and roadside monitoring, approaches which are time consuming, expensive, and lack spatial and temporal accuracy [1]. -

List of Publicly Accessible Locations Where E-Bins Are Deployed*
List of publicly accessible locations where E-Bins are deployed* *This is a working list, more locations will be added every week* Name Location Type of Bin Placed Best Denki • 1 Harbourfront Walk, Vivocity, #2-07 • 3155 Commonwealth Avenue West, The Clementi Mall, #04-46/47/48/49 • 68 Orchard Road, Plaza Singapura, #3-39 • 2 Jurong East Street 21, IMM, #3-33 • 63 Jurong West Central 3, Jurong Point, #B1-92 • 109 North Bridge Road, Funan, #3-16 3-in-1 Bin • 1 Kim Seng Promenade, Great World City, #07-01 (ICT, Bulb, Battery) • 391A Orchard Road, Ngee Ann City Tower A • 9 Bishan Place, Junction 8 Shopping Centre, #03-02 • 17 Petir Road, Hillion Mall, #B1-65 • 83 Punggol Central, Waterway Point • 311 New Upper Changi Road, Bedok Mall Cash • 135 Jurong Gateway Road 3-in-1 Bin Converters • 510 Tampines Central 1 (ICT, Bulb, Battery) Challenger • 302 Tiong Bahru Road, Tiong Bahru Plaza, #03-19 • 1 Jurong West Central 2, Jurong Point, #B1-94 • 200 Victoria Street, Bugis Junction, #03-10E • 5 Changi Business Park Central 1, Changi City Point, #01-56 3-in-1 Bin • 3 Simei Street 6, Eastpoint Mall, #B1-08 (ICT, Bulb, Battery) • 90 Hougang Avenue 10, Hougang Mall, #02-13 • 10 Paya Lebar Road, Paya Lebar Quarter (PLQ), #04-01 • 10 Tampines Central 1, Tampines 1, #04-25 City Square Mall • 180 Kitchener Road 3-in-1 Bin (ICT, Bulb, Battery) Compass One • 1 Sengkang Square, #B1-52/53 3-in-1 Bin (ICT, Bulb, Battery) Dairy Farm • Cold Storage, 5 Stadium Walk, Kallang Leisure Park, #B1-01 Group • Giant Hypermarket, 521 Tampines North Drive 2, #03-01, Singapore -

List of Licensed General Waste Disposal Facilities (Gwdfs) IMPORTANT NOTE: Please Contact the Companies for More Information
List of Licensed General Waste Disposal Facilities (GWDFs) IMPORTANT NOTE: Please contact the companies for more information. Since 1 August 2017, NEA began licensing General Waste Disposal Facilities (GWDFs). A GWDF is defined as a disposal facility which receives, stores, sorts, treats or processes general waste, and includes recycling facilities. Companies can apply for the Licence/Exemption via https://licence1.business.gov.sg. All general waste disposal facilities must obtain their licence or submit an exemption declaration by 31 July 2018. For more information on the GWDF Licence, please visit http://www.nea.gov.sg/energy-waste/waste-management/general-waste-disposal-facility/ Waste Stream Company Facility Address Contacts Ash Paper Plastic Sludge E-Waste Steel Slag Steel C&D waste C&D Refrigerant Scrap Metal Scrap Glass Waste Glass WoodWaste Textile Waste Textile Biomass Waste Biomass Return Concrete Return Used Cooking Oil Cooking Used Spent Copper Slag Spent Copper Mixed Recyclables Mixed Horticultural Waste Horticultural Tyre/RubberWaste Used CoffeeCapsules Used Refrigerant Cylinder/Tank Refrigerant Waste generated from the from generated Waste manufacture of electrical and manufactureofelectrical Industrial and Commercial Waste andCommercial Industrial 800 Super Waste Management 6 Tuas South Street 7 636892 [email protected]; Y Pte Ltd 62 Sungei Kadut Street 1 Sungei [email protected]; 85 Auto Trading Y Kadut Industrial Estate 729363 [email protected]; 21 Tuas West Avenue #03-01 A~Star Plastics Pte Ltd [email protected] -
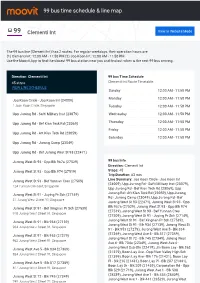
99 Bus Time Schedule & Line Route
99 bus time schedule & line map 99 Clementi Int View In Website Mode The 99 bus line (Clementi Int) has 2 routes. For regular weekdays, their operation hours are: (1) Clementi Int: 12:00 AM - 11:50 PM (2) Joo Koon Int: 12:00 AM - 11:50 PM Use the Moovit App to ƒnd the closest 99 bus station near you and ƒnd out when is the next 99 bus arriving. Direction: Clementi Int 99 bus Time Schedule 45 stops Clementi Int Route Timetable: VIEW LINE SCHEDULE Sunday 12:00 AM - 11:50 PM Monday 12:00 AM - 11:50 PM Joo Koon Circle - Joo Koon Int (24009) 1 Joon Koon Circle, Singapore Tuesday 12:00 AM - 11:50 PM Upp Jurong Rd - Safti Military Inst (23079) Wednesday 12:00 AM - 11:50 PM Upp Jurong Rd - Bef Kian Teck Rd (23069) Thursday 12:00 AM - 11:50 PM Friday 12:00 AM - 11:50 PM Upp Jurong Rd - Aft Kian Teck Rd (23059) Saturday 12:00 AM - 11:50 PM Upp Jurong Rd - Jurong Camp (23049) Upp Jurong Rd - Bef Jurong West St 93 (22471) Jurong West St 93 - Opp Blk 987a (27529) 99 bus Info Direction: Clementi Int Jurong West St 93 - Opp Blk 974 (27519) Stops: 45 Trip Duration: 63 min Jurong West St 93 - Bef Yunnan Cres (27509) Line Summary: Joo Koon Circle - Joo Koon Int (24009), Upp Jurong Rd - Safti Military Inst (23079), 124 Yunnan Crescent, Singapore Upp Jurong Rd - Bef Kian Teck Rd (23069), Upp Jurong Rd - Aft Kian Teck Rd (23059), Upp Jurong Jurong West St 91 - Juying Pr Sch (27149) Rd - Jurong Camp (23049), Upp Jurong Rd - Bef 31 Jurong West Street 91, Singapore Jurong West St 93 (22471), Jurong West St 93 - Opp Blk 987a (27529), Jurong West St 93 - Opp Blk -

Slides by JTC GD Calvin Chung
• Sungei Kadut Eco-District • Seletar Aerospace Park Catalysing Industrial Transformation for sustainability Mr. Calvin Chung Group Director/ Chief Environmental Officer 25 May 2021 1. National Challenges and Sustainability Targets 2 Carbon – the New Constraint for Singapore ▪ Singapore is no stranger to constraints: land scarce, lack of water. Carbon would be a new addition to the list ▪ Like Our Water Story – Singapore is embarking on another journey to address the carbon constraint Singapore carbon emission projection (Climate Action Tracker) ▪ Singapore has signed Paris Agreement and committed to 36% reduction in emission intensity below 2005 by 2030 ▪ Singapore national targets: peak emission of 65 million tons of CO2e by 2030 and to be halved by 2050 ▪ A carbon tax for industrial facilities at $5 SGD/tCo2e was implemented in 2019, to be reviewed in 2023 ▪ A 2GW target by 2030 for solar energy was unveiled Peak by 2030, in SIEW 2019 halved by 2050 4oC+ Critically Insufficient <3oC Insufficient <1.5oC Paris Agreement <4oC Highly Insufficient <2oC Compatible <<1.5oC Role Model 3 Strong National Drive Towards Sustainability – SG Green Plan 2030 • SG Green Plan - An overarching sustainability vision for Singapore, a whole-of-nation action plan to realise the vision, and a relatable communication with the public to inspire action • JTC’s ongoing sustainability effort has already been contributing to the SG Green Plan pillars. City in Nature Energy Reset Sustainable Living Green Economy Resilient Future ▪ One million more ▪ Green 80% of -

Notice of Contested Election for the Electoral Division of Hong Kah North
FRIDAY, SEPTEMBER 4, 2015 1 First published in the Government Gazette, Electronic Edition, on 1st September 2015 at 7.00 pm. No. 2186 –– PARLIAMENTARY ELECTIONS ACT (CHAPTER 218) (Section 34(6)) NOTICE OF CONTESTED ELECTION FOR THE ELECTORAL DIVISION OF HONG KAH NORTH NOTICE is given to the electors of the above Electoral Division that a Poll will be held for the Electoral Division as follows. POLL IN SINGAPORE The Poll in Singapore will be held on 11 September 2015. The Poll will open at 8 a.m. and close at 8 p.m. at the Polling Stations in the Electoral Division below: Polling Stations Polling Districts Westwood Primary School Canteen Hong Kah North Jurong West Street 73 HN One ... HN.01 HDB Pavilion Block 760B Hong Kah North Jurong West Street 74 HN Two ... HN.02 Westwood Secondary School Canteen Hong Kah North Jurong West Street 25 HN Three ... HN.03 HDB Pavilion Block 272 Hong Kah North Jurong West Street 24 HN Four ... HN.04 Dunearn Secondary School Canteen (A) Hong Kah North Bukit Batok West Avenue 2 HN Five ... HN.05 St. Anthony’s Primary School Canteen (A) Hong Kah North Bukit Batok Street 32 HN Six ... HN.06 St. Anthony’s Primary School Canteen (B) Hong Kah North Bukit Batok Street 32 HN Seven ... HN.07 Dazhong Primary School Canteen (A) Hong Kah North Bukit Batok Street 31 HN Eight ... HN.08 Dazhong Primary School Canteen (B) Hong Kah North Bukit Batok Street 31 HN Nine ... HN.09 Dunearn Secondary School Canteen (B) Hong Kah North Bukit Batok West Avenue 2 HN Ten .. -

243G Bus Time Schedule & Line Route
243G bus time schedule & line map 243G Boon Lay Int View In Website Mode The 243G bus line Boon Lay Int has one route. For regular weekdays, their operation hours are: (1) Boon Lay Int: 12:00 AM - 11:54 PM Use the Moovit App to ƒnd the closest 243G bus station near you and ƒnd out when is the next 243G bus arriving. Direction: Boon Lay Int 243G bus Time Schedule 15 stops Boon Lay Int Route Timetable: VIEW LINE SCHEDULE Sunday 12:00 AM - 11:54 PM Monday 12:00 AM - 11:54 PM Jurong West Ctrl 3 - Boon Lay Int (22009) 61 Jurong West Central 3, Singapore Tuesday 12:00 AM - 11:54 PM Jurong West St 64 - Blk 669 Cp (22441) Wednesday 12:00 AM - 11:54 PM Walking Trail, Singapore Thursday 12:00 AM - 11:54 PM Jurong West St 64 - Blk 670a (22591) Friday 12:00 AM - 11:54 PM 670A Jurong West Street 65, Singapore Saturday 12:00 AM - 11:54 PM Jurong West St 75 - Opp Blk 755 (27371) Jurong West St 75 - Blk 749 (27381) Jurong West St 82 - Blk 857 (27391) 243G bus Info Jurong West Street 82, Singapore Direction: Boon Lay Int Stops: 15 Jurong West St 81 - Blk 821 (27409) Trip Duration: 17 min 821 Jurong West Street 81, Singapore Line Summary: Jurong West Ctrl 3 - Boon Lay Int (22009), Jurong West St 64 - Blk 669 Cp (22441), Jurong West St 81 - Blk 827 (27419) Jurong West St 64 - Blk 670a (22591), Jurong West 827 Jurong West Street 81, Singapore St 75 - Opp Blk 755 (27371), Jurong West St 75 - Blk 749 (27381), Jurong West St 82 - Blk 857 (27391), Jurong West Ave 5 - Blk 710 (27361) Jurong West St 81 - Blk 821 (27409), Jurong West St 710 Jurong West Street 71, -

The Intervention of Plants in the Conflicts Between Buildings and Climate
THE INTERVENTION OF PLANTS IN THE CONFLICTS BETWEEN BUILDINGS AND CLIMATE ─ A CASE STUDY IN SINGAPORE CHEN YU (B. Arch., M.A. (Arch.)) A THESIS SUBMITTED FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF BUILDING NATIONAL UNIVERSITY OF SINGAPORE 2006 ACKNOWLEDGMENTS I could not come this far without my supervisor, Associate Prof. Wong Nyuk Hien, who guided, encouraged, and supported me not only as a patient teacher but also a great friend. I did benefit a lot from the unrestricted research environment and the tradition of being productive in his team. My appreciation should also extend to my thesis committee members, Dr. Lim Guan Tiong and Dr Liew Soo Chin for their invaluable advices and interests in my research work. It is also my deep gratitude that I can work under many different research projects during the last few years with Dr Tan Puay Yok, Ms Ong Chui Leng, Ms Angelia Sia from National Parks Board (NParks), Mr Wong Wai Ching from Building and Construction Authority (BCA), Mr Wong Siu Tee and Mr Calvin Chung From JTC Corporation, and Ms Tay Bee Choo from Housing and Development Board (HDB). The invaluable experience and the related research findings are of great help in this dissertation writing. Of particular significant is the experimental environment and the plants provided by NParks in its Pasir Panjiang nursery. I am grateful to Ms Boo Chih Min, Dr Tan Puay Yok, and Ms Angelia Sia for their effort in expediting the process. Meanwhile, without the kind help provided by Madam Chua-Tan Boon Gek and Ms Sanisah Rasman on the spot, the tedious field work would exhaust my patience at the very beginning. -

Participating Merchants Address Postal Code Club21 3.1 Phillip Lim 581 Orchard Road, Hilton Hotel 238883 A|X Armani Exchange
Participating Merchants Address Postal Code Club21 3.1 Phillip Lim 581 Orchard Road, Hilton Hotel 238883 A|X Armani Exchange 2 Orchard Turn, B1-03 ION Orchard 238801 391 Orchard Road, #B1-03/04 Ngee Ann City 238872 290 Orchard Rd, 02-13/14-16 Paragon #02-17/19 238859 2 Bayfront Avenue, B2-15/16/16A The Shoppes at Marina Bay Sands 018972 Armani Junior 2 Bayfront Avenue, B1-62 018972 Bao Bao Issey Miyake 2 Orchard Turn, ION Orchard #03-24 238801 Bonpoint 583 Orchard Road, #02-11/12/13 Forum The Shopping Mall 238884 2 Bayfront Avenue, B1-61 018972 CK Calvin Klein 2 Orchard Turn, 03-09 ION Orchard 238801 290 Orchard Road, 02-33/34 Paragon 238859 2 Bayfront Avenue, 01-17A 018972 Club21 581 Orchard Road, Hilton Hotel 238883 Club21 Men 581 Orchard Road, Hilton Hotel 238883 Club21 X Play Comme 2 Bayfront Avenue, #B1-68 The Shoppes At Marina Bay Sands 018972 Des Garscons 2 Orchard Turn, #03-10 ION Orchard 238801 Comme Des Garcons 6B Orange Grove Road, Level 1 Como House 258332 Pocket Commes des Garcons 581 Orchard Road, Hilton Hotel 238883 DKNY 290 Orchard Rd, 02-43 Paragon 238859 2 Orchard Turn, B1-03 ION Orchard 238801 Dries Van Noten 581 Orchard Road, Hilton Hotel 238883 Emporio Armani 290 Orchard Road, 01-23/24 Paragon 238859 2 Bayfront Avenue, 01-16 The Shoppes at Marina Bay Sands 018972 Giorgio Armani 2 Bayfront Avenue, B1-76/77 The Shoppes at Marina Bay Sands 018972 581 Orchard Road, Hilton Hotel 238883 Issey Miyake 581 Orchard Road, Hilton Hotel 238883 Marni 581 Orchard Road, Hilton Hotel 238883 Mulberry 2 Bayfront Avenue, 01-41/42 018972 -

Press Release
EMBARGOED TILL 8.00PM, 8 SEPTEMBER 2016 PRESS RELEASE Unveiling the Masterplan for Tengah : At Home With Nature Minister for National Development, Mr Lawrence Wong unveiled the masterplan for Singapore’s 24th HDB town, Tengah, at the HDB Awards Ceremony on 8 September 2016. Following the announcement, a public exhibition on the key planning concepts for Tengah will be held from 9 to 25 September 2016 at HDB Hub. 2 As the master planner and developer of Singapore’s public housing estates, HDB is constantly on the lookout for innovative ideas to provide residents with a quality living environment. In line with HDB’s Roadmap to provide well-designed, sustainable and community-centric towns, we have seen the steady completion of a new generation of public housing projects in recent years, each with their own distinctive designs, abundant green spaces, seamlessly-connected cycling and pedestrian networks, and vibrant community spaces for interaction. The upcoming new “Forest Town”, Tengah, will further raise the bar for public housing, with its fresh planning concepts, bold ideas and innovative designs. 3 Located in the Western region of Singapore, Tengah is bounded by the Kranji Expressway (KJE), Pan-Island Expressway (PIE), Brickland Road and Bukit Batok Road. The key driving planning concept behind Tengah is the creation of a “Forest Town”, with homes surrounded by lush greenery and nature, where residents can enjoy quality living and connect with the community in a myriad of amenities and green spaces. Tengah, Singapore’s 24th HDB town, will be transformed into a “Forest Town” that is green, sustainable and smart EMBARGOED TILL 8.00PM, 8 SEPTEMBER 2016 4 The development of Tengah will be guided by six key ideas as follows: Creating an evergreen forest town Provisions for moving around with ease Provisions for walking and cycling everywhere Creating five unique housing districts Enabling close-knit communities Creating a Smart and sustainable town 5 Tengah will see several ‘firsts’ in its development.