Problem of Pulmonary Embolism : Report of Thirty Nine Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

USMLE – What's It
Purpose of this handout Congratulations on making it to Year 2 of medical school! You are that much closer to having your Doctor of Medicine degree. If you want to PRACTICE medicine, however, you have to be licensed, and in order to be licensed you must first pass all four United States Medical Licensing Exams. This book is intended as a starting point in your preparation for getting past the first hurdle, Step 1. It contains study tips, suggestions, resources, and advice. Please remember, however, that no single approach to studying is right for everyone. USMLE – What is it for? In order to become a licensed physician in the United States, individuals must pass a series of examinations conducted by the National Board of Medical Examiners (NBME). These examinations are the United States Medical Licensing Examinations, or USMLE. Currently there are four separate exams which must be passed in order to be eligible for medical licensure: Step 1, usually taken after the completion of the second year of medical school; Step 2 Clinical Knowledge (CK), this is usually taken by December 31st of Year 4 Step 2 Clinical Skills (CS), this is usually be taken by December 31st of Year 4 Step 3, typically taken during the first (intern) year of post graduate training. Requirements other than passing all of the above mentioned steps for licensure in each state are set by each state’s medical licensing board. For example, each state board determines the maximum number of times that a person may take each Step exam and still remain eligible for licensure. -
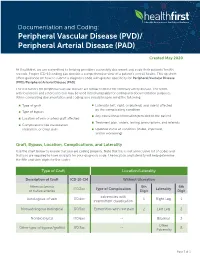
Documentationand Coding Tips: Peripheral Vascular Disease
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Thrombosis, Embolism, Infarction
Thrombosis, Embolism and Infarction THROMBOSIS Thrombus formation (called Virchow's triad): (1) endothelial injury, (2) stasis or turbulent blood flow (3) hypercoagulability of the blood Endothelial Injury Endothelial injury is particularly important for thrombus formation in the heart or the arterial circulation, where the normally high flow rates might otherwise impede clotting by preventing platelet adhesion and washing out activated coagulation factors. Thus, thrombus formation within cardiac chambers (e.g., after endocardial injury due to myocardial infarction), over ulcerated plaques in atherosclerotic arteries, or at sites of traumatic or inflammatory vascular injury (vasculitis) is largely a consequence of endothelial cell injury. Endothelial Injury Physical loss of endothelium can lead to exposure of the subendothelial ECM, adhesion of platelets, release of tissue factor, and local depletion of PGI2 and plasminogen activators. However, it should be emphasized that endothelium need not be denuded or physically disrupted to contribute to the development of thrombosis; any perturbation in the dynamic balance of the prothombotic and antithrombotic activities of endothelium can influence local clotting events. Thus, dysfunctional endothelial cells can produce more procoagulant factors (e.g., platelet adhesion molecules, tissue factor, PAIs) or may synthesize less anticoagulant effectors (e.g., thrombomodulin, PGI2, t-PA). Endothelial dysfunction can be induced by a wide variety of insults, including hypertension, turbulent blood flow, bacterial endotoxins, radiation injury, metabolic abnormalities such as hypercholesterolemia. Alterations in Normal Blood Flow Turbulence contributes to arterial and cardiac thrombosis by causing endothelial injury or dysfunction, as well as by forming countercurrents and local pockets of stasis; stasis is a major contributor in the development of venous thrombi. -

Association Between Multi-Site Atherosclerotic Plaques and Systemic Arteriosclerosis
Association between multi-site atherosclerotic plaques and systemic arteriosclerosis: results from the BEST study (Beijing Vascular Disease Patients Evaluation Study) huan liu Peking University Shougang Hospital https://orcid.org/0000-0001-6223-7677 Jinbo Liu Peking University Shougang Hospital Wei Huang Peking University Shougang Hospital Hongwei Zhao Peking University Shougang Hospital Na zhao Peking University Shougang Hospital Hongyu wang ( [email protected] ) Research Keywords: arteriosclerosis, atherosclerosis, atherosclerotic plaque, carotid femoral artery pulse wave velocity CF-PWV Posted Date: June 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-31641/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on August 1st, 2020. See the published version at https://doi.org/10.1186/s12947-020-00212-3. Page 1/18 Abstract Background Arteriosclerosis can be reected in various aspect of the artery, including atherosclerotic plaque formation or stiffening on the arterial wall. Both arteriosclerosis and atherosclerosis are important and closely associated with cardiovascular disease (CVD). The aim of the study was to evaluate the association between systemic arteriosclerosis and multi-site atherosclerotic plaques. Methods The study was designed as an observational cross-sectional study. A total of 1178 participants (mean age 67.4 years; 52.2% male) enrolled into the observational study from 2010 to 2017. Systemic arteriosclerosis was assessed by carotid femoral artery pulse wave velocity (CF-PWV) and multi-site atherosclerotic plaques (MAP, >=2 of the below sites) were reected in the carotid or subclavian artery, abdominal aorta and lower extremities arteries using ultrasound equipment. -

3. Thrombosis. Embolism. DIC. Shock
3. Thrombosis. Embolism. DIC. Shock. PATHOLOGY OF VASCULAR OCCLUSION: thrombosis, embolism, disseminated intravascular coagulation (DIC) Hemostasis (”stopping of hemorrhage”) Physiological process to maintain blood in a fluid, clot-free state in normal vessels, and to stop bleeding from ruptured vessels Main components of hemostasis: endothelium, platelets, and coagulation proteins Endothelial cells have both procoagulant and anticoagulant properties, and according to the needs of the body they may either promote clotting or inhibiting it Procoagulant functions Release of • von Willebrand factor (vWF); mediates the binding of platelets to endothelial surfaces • Tissue factor (TF); promotes the extrinsic pathway of the coagulation cascade • Inhibitors of plasminogen activator Anticoagulant functions • Inhibition of platelet aggregation via prostacyclin secretion • Dilation of blood vessels via nitric oxide secretion • Antithrombin activity, accomplished by thrombomodulin, which captures thrombin • Fibrinolysis, via secreting plasminogen activator, which generates plasmin from plasminogen Platelets Upon contact with TF and/or vWF, platelets become activated and 1) adhere to injured sites 2) release chemical mediators to induce further platelet aggregation, and activation of coagulation proteins 3) aggregate with other platelets and form the hemostatic plug. Both RBCs and leukocytes are also found in hemostatic plugs. Coagulation proteins Group of plasma proteins that are activated by acting upon each other in a sequence known as the extrinsic and intrinsic pathway. These proteins converge, and finally thrombin converts fibrinogen to fibrin within and about the platelet plug. THROMBOSIS • Intravascular clotting in a living person • Clots formed inside the blood vessels or cardiac chambers are called thrombi • Thrombi are always potential sources of further complications Factors promoting thrombus formation (Virchow’s triad) 1. -

A Whole Blood Thrombus Mimic: Constitutive Behavior Under Simple Shear a B a a a Gabriella P
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.19.210732; this version posted July 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. A Whole Blood Thrombus Mimic: Constitutive Behavior Under Simple Shear a b a a a Gabriella P. Sugerman , Sotirios Kakaletsis , Parin Thakkar , Armaan Chokshi , Sapun H. Parekh a,b,g < and Manuel K. Rausch , aUniversity of Texas at Austin, Department of Biomedical Engineering, 107 W Dean Keeton St, Austin, TX 78712 bUniversity of Texas at Austin, Department of Aerospace Engineering & Engineering Mechanics, 2617 Wichita St, Austin, TX 78712 gUniversity of Texas at Austin, Oden Institute for Computational Engineering and Sciences, 201 E 24th St, Austin, TX 78712 ARTICLEINFO ABSTRACT Keywords: Deep vein thrombosis and pulmonary embolism affect 300,000-600,000 patients each year in the US. venous thrombus The progression from deep vein thrombus to pulmonary embolism occurs when blood clots, as a hyperelasticity whole or partially, break off from the deep veins and eventually occlude the pulmonary arteries. Ve- large deformation nous thromboembolism is the cause of up to 100,000 deaths per year in the US alone. To date, we deep vein thrombosis don’t fully understand this mechanical process among other reasons because in-vivo samples are dif- pulmonary embolism ficult to obtain, highly heterogeneous, and their shapes are inappropriate for most mechanical tests. Toward overcoming these obstacles, we have set out to develop an in-vitro thrombus mimic and to test this mimic under large deformation simple shear. -

Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: the Hisayama Study
JASN Express. Published on June 20, 2007 as doi: 10.1681/ASN.2007010067 CLINICAL EPIDEMIOLOGY www.jasn.org Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: The Hisayama Study Toshiharu Ninomiya,* Michiaki Kubo,* Yasufumi Doi,† Koji Yonemoto,* Yumihiro Tanizaki,* Kazuhiko Tsuruya,† Katsuo Sueishi,‡ Masazumi Tsuneyoshi,§ Mitsuo Iida,† and Yutaka Kiyohara* Departments of *Environmental Medicine, †Medicine and Clinical Science, ‡Pathophysiological and Experimental Pathology, and §Anatomic Pathology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan ABSTRACT Information regarding the association between prehypertension BP level and renal arteriosclerosis is limited. In 652 consecutive population-based autopsy samples without hypertension treatment before death, the relationship between the severity of renal arteriosclerosis and BP levels classified according to the criteria of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure was examined. The age- and gender-adjusted frequencies of renal arteriosclerosis linearly increased with elevating BP levels; both hypertensive and prehypertensive subjects had significantly higher frequencies of renal arteriosclerosis than subjects with normal BP (normal 11.9%; prehypertension 28.5%; stage 1 hypertension 32.9%; stage 2 hypertension 58.2%; all P Ͻ 0.01 versus normal). In a logistic regression model, prehypertension was significantly associated with renal arteriosclerosis after adjustment for other cardiovascular risk factors (prehyper- tension multivariate-adjusted odds ratio [mOR] 5.99 [95% confidence interval (CI) 2.20 to 15.97]; stage 1 hypertension mOR 6.99 [95% CI 2.61 to 18.72]; stage 2 hypertension mOR 22.21 [95% CI 8.35 to 59.08]). This significant association was observed for all renal arterial sizes. -

Peripheral Vascular Disease Becomes Increasingly Prevalent with by the Symptom Or Complication (E.G
SePTeMBer 2010 Informative and educational updates for providers FOCUS ON: PerIPherAl Always… • Document the cause of the peripheral arterial disease, VASCUlAr DISeASe if known, as well as the complication (e.g. PAD due to diabetes with ulcer lower leg). • Document arteriosclerosis as “arteriosclerosis of” and the site, “arteriosclerotic” or “arteriosclerosis with,” followed Peripheral vascular disease becomes increasingly prevalent with by the symptom or complication (e.g. arteriosclerosis of age. As such this is a growing concern in the United States given the the lower extremities with rest pain, arteriosclerosis of growing proportion of older adults. Based on a NhANeS report the the lower extremities with ulceration), not the symptom incidence can be as high as 15 to 17% in the population aged 70 and or complication alone. over. Documentation and Coding Tips4 The concern around peripheral vascular disease is several fold: Only a minority of patients may present with the classic symptoms of • “Peripheral arterial disease,” “peripheral vascular disease” limb claudication or ischemia. In one study only about 11 percent of and “intermittent claudication” are coded to 443.9 – the patients with PVD presented with classic symptoms.1 In another Peripheral vascular disease, unspecified. study as many as 28 percent of patients with peripheral vascular • Atherosclerosis of the native arteries of the extremities is disease were found to be physically inactive sometimes due to other coded based on documentation of the condition with the illness thereby precluding the development of symptoms.2 There is a symptom or complication: significant overlap of peripheral vascular disease with coronary artery 440.20 – Atherosclerosis of the extremities, unspecified disease, cerebrovascular disease and abdominal aortic aneurysms. -

Intracranial Vertebral Artery Dissection in Wallenberg Syndrome
Intracranial Vertebral Artery Dissection in Wallenberg Syndrome T. Hosoya, N. Watanabe, K. Yamaguchi, H. Kubota, andY. Onodera PURPOSE: To assess the prevalence of vertebral artery dissection in Wallenberg syndrome. METHODS: Sixteen patients (12 men, 4 women; mean age at ictus, 51 .6 years) with symptoms of Wallenberg syndrome and an infarction demonstrated in the lateral medulla on MR were reviewed retrospectively. The study items were as follows: (a) headache as clinical signs, in particular, occipitalgia and/ or posterior neck pain at ictus; (b) MR findings, such as intramural hematoma on T1-weighted images, intimal flap on T2-weighted images, and double lumen on three-dimensional spoiled gradient-recalled acquisition in a steady state with gadopentetate dimeglumine; (c) direct angiographic findings of dissection, such as double lumen, intimal flap, and resolution of stenosis on follow-up angiography; and (d) indirect angiographic findings of dissection (such as string sign, pearl and string sign, tapered narrowing, etc). Patients were classified as definite dissection if they had reliable MR findings (ie, intramural hematoma, intimal flap, and enhancement of wall and septum) and/ or direct angiographic findings; as probable dissection if they showed both headache and suspected findings (ie, double lumen on 3-D spoiled gradient-recalled acquisition in a steady state or indirect angiographic findings) ; and as suspected dissection in those with only headache or suspected findings. RESULTS: Seven of 16 patients were classified as definite dissection, 3 as probable dissection, and 3 as suspected dissection. Four patients were considered to have bilateral vertebral artery dissection on the basis of MR findings. CONCLUSIONS: Vertebral artery dissection is an important cause of Wallenberg syndrome. -

Doppler Ultrasound Exam of an Arm Or Leg Doppler Ultrasound Exam of an Arm Or Leg
30/07/2019 Doppler ultrasound exam of an arm or leg Doppler ultrasound exam of an arm or leg Definition This test uses ultrasound to look at the blood flow in the large arteries and veins in the arms and legs. Alternative Names Peripheral vascular disease - Doppler; PVD - Doppler; PAD - Doppler; Blockage of leg arteries - Doppler; Intermittent claudication - Doppler; Arterial insufficiency of the legs - Doppler; Leg pain and cramping - Doppler; Calf pain - Doppler; Venous Doppler - DVT How the Test is Performed The test is done in the ultrasound or radiology department or in a peripheral vascular lab. During the exam: A water-soluble gel is placed on a handheld device called a transducer. This device directs high-frequency sound waves to the artery or veins being tested. Blood pressure cuffs may be put around different parts of the body, including the thigh, calf, ankle, and different points along the arm. A paste is applied to the skin over the arteries or veins being examined. Images are created as the transducer is moved over each area. How to Prepare for the Test You will need to remove clothes from the arm or leg being examined. How the Test will Feel Sometimes, the person performing the test will need to press on the vein to make sure it does not have a clot. Some people may feel slight pain. Why the Test is Performed This test is done as the first step to look at arteries and veins. Sometimes, arteriography and venography may be needed later. The test is done to help diagnose: Arteriosclerosis of the arms or legs Blood clot (deep vein thrombosis) Venous insufficiency The test may also be used to: Look at injury to the arteries Monitor arterial reconstruction and bypass grafts Normal Results printer-friendly.adam.com/content.aspx?print=1&productId=117&pid=1&gid=003775&c_custid=1549 1/2 30/07/2019 Doppler ultrasound exam of an arm or leg A normal result means the blood vessels show no signs of narrowing, clots, or closure, and the arteries have normal blood flow. -

Mechanisms of Thrombosis
Mechanisms of Thrombosis Maureane Hoffman, MD, PhD Professor of Pathology Thrombosis • Formation of a blood clot in an artery or vein of a living person • Arterial thrombosis denies oxygen and nutrition to an area of the body – Thrombosis of an artery leading to the heart causes a myocardial infarction – Thrombosis of an artery leading to the brain causes a stroke • Acute arterial thrombosis often results from the deposition of atherosclerotic material in the wall of an artery, which gradually narrows the channel, precipitating clot formation Thrombosis • Extends into vessel without blocking it completely - mural thrombus • Blocks it completely - occlusive thrombus • Extends along the blood vessel - propagative thrombus Thrombosis • Venous thrombosis blocks return of deoxygenated blood to the heart • Venous thrombosis is quite common in the lower extremities, but can also occur in the upper extremeties • Symptoms include swelling, bluish discoloration and pain. • The most feared complication of venous thrombosis is pulmonary embolism Pulmonary Emboli Lines of Zahn in a pulmonary embolus Is it thrombus or post-mortem clot? • Thrombus adheres to the vessel wall • May be red, white, or mixed • Is crumbly and layered Small pulmonary emboli Thrombosis in the Aorta What Causes Thrombosis? Virchow’s Triad: Stasis Vascular Injury Hypercoagulability Vascular Injury endothelial cell TF TF VIIa Hypercoagulability The coagulant/anticoagulant proteins and the cells each play a role Evolution of the Paradigm Old: Hypercoagulable State = Systemic -
Aetiology of Deep Venous Thrombosis - Implications for Prophylaxis
6 Aetiology of Deep Venous Thrombosis - Implications for Prophylaxis Paul S. Agutter and P. Colm Malone Theoretical Medicine and Biology Group, United Kingdom 1. Introduction Clinical research on deep venous thrombosis (DVT) and thromboembolism (VTE) has focused in recent years on the contributions of potentiating factors, alone and in combination, to the risk of contracting these conditions. Many such ‘risk factors’ have been identified (Geerts et al., 2004) and are discussed elsewhere in this book. The National Institute for Clinical Excellence (NICE) in the United Kingdom has exploited this knowledge to make the prevention of DVT its main focus for 2011. In his keynote lecture introducing the policy and procedures adopted by NICE, Arya (2011) described the tools for evaluating risk in various patient groups and emphasised ‘anticoagulation’ in the design and implementation of evidence-based prophylactic measures. He claimed that the frequency of VTE in hospital patients should be reduced by 2/3 if the agreed protocols are followed. An achievement of that magnitude would be most welcome. Comparable views have been articulated elsewhere in Europe. Although NICE is distinctive in recommending assessment for thromboprophylaxis for all medical inpatients, the health services of other European Union countries offer broadly similar guidelines, especially for patients with acute medical conditions with expected durations of hospital stay longer than 3-4 days (Khoury et al., 2011). Similarly, in the USA, the Surgeon General issued a ‘Call to Action to Prevent Deep Venous Thrombosis and Pulmonary Embolism’ in 2008 (Sliwka & Fang, 2010), and the Joint Commission on Accreditation of Healthcare Organizations requires prophylaxis for patients at moderate or high risk of VTE (Rothberg et al., 2010).