Insert Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Runway 05/23
TORONTO PEARSON NOISE OFFICE NOTICE DATES Noise Office Complaint Phone: 416-247-7682 2021-02-17 to 2021-10-17 WebTrak: webtrak5.bksv.com/gta Online Noise Complaint click here Time period Runway Type of work UPDATE 05/23 A temporary closure of Runway 05/23 is required to allow access to the site August 1 to mid-October 2021, Runway 05/23 is part and due to the proximity of the work Monday to Saturday from 8:00 pm to of our preferential site to the runway 7:30 am nightly runway system *Between February 17 and July 30, 2021, the closure consisted of daytime work. This was moved to nighttime to accommodate for increasing traffic volume. Scope of the closure Aircraft manufacturer Bombardier is relocating its assembly operations from Downsview to Toronto Pearson. To accommodate this work a temporary closure of Runway 05/23 is required to allow access to the site. This closure can be cancelled day of in case of inclement weather. Please note that the closure dates are dependent on weather conditions, and an extension of closure dates is possible. Between the hours of 6:30am to 7:30 am and 8:00pm to midnight: This is a closure of one of the east/west runways; most traffic will move to one of the other east/west runways, Runway 06L/24R or 06R/24L and in combination with arrivals on Runway 15L or departures on Runway 33R. These runways are already in regular use, however there may be change to the proportion of traffic. The North/South runways may be used at times during traffic peaks to accommodate the higher traffic levels. -

Part I, Vol. 145, Extra No. 6
EXTRA Vol. 145, No. 6 ÉDITION SPÉCIALE Vol. 145, no 6 Canada Gazette Gazette du Canada Part I Partie I OTTAWA, FRIDAY, MAY 20, 2011 OTTAWA, LE VENDREDI 20 MAI 2011 CHIEF ELECTORAL OFFICER DIRECTEUR GÉNÉRAL DES ÉLECTIONS CANADA ELECTIONS ACT LOI ÉLECTORALE DU CANADA Return of Members elected at the 41st general election Rapport de députés(es) élus(es) à la 41e élection générale Notice is hereby given, pursuant to section 317 of the Canada Avis est par les présentes donné, conformément à l’article 317 Elections Act, that returns, in the following order, have been de la Loi électorale du Canada, que les rapports, dans l’ordre received of the election of Members to serve in the House of ci-dessous, ont été reçus relativement à l’élection de députés(es) à Commons of Canada for the following electoral districts: la Chambre des communes du Canada pour les circonscriptions ci-après mentionnées : Electoral Districts Members Circonscriptions Députés(es) Saskatoon—Humboldt Brad Trost Saskatoon—Humboldt Brad Trost Tobique—Mactaquac Mike Allen Tobique—Mactaquac Mike Allen Pickering—Scarborough East Corneliu Chisu Pickering—Scarborough-Est Corneliu Chisu Don Valley East Joe Daniel Don Valley-Est Joe Daniel Brampton West Kyle Seeback Brampton-Ouest Kyle Seeback Eglinton—Lawrence Joe Oliver Eglinton—Lawrence Joe Oliver Fundy Royal Rob Moore Fundy Royal Rob Moore New Brunswick Southwest John Williamson Nouveau-Brunswick-Sud-Ouest John Williamson Québec Annick Papillon Québec Annick Papillon Cypress Hills—Grasslands David Anderson Cypress Hills—Grasslands David Anderson West Vancouver—Sunshine West Vancouver—Sunshine Coast—Sea to Sky Country John Dunbar Weston Coast—Sea to Sky Country John Dunbar Weston Regina—Qu’Appelle Andrew Scheer Regina—Qu’Appelle Andrew Scheer Prince Albert Randy Hoback Prince Albert Randy Hoback Algoma—Manitoulin— Algoma—Manitoulin— Kapuskasing Carol Hughes Kapuskasing Carol Hughes West Nova Greg Kerr Nova-Ouest Greg Kerr Dauphin—Swan River—Marquette Robert Sopuck Dauphin—Swan River—Marquette Robert Sopuck Crowfoot Kevin A. -

Orking Rough, Living Poor
Working Rough, Living Poor Employment and Income Insecurities faced by Racialized Groups and their Impacts on Health Published by Access Alliance Multicultural Health and Community Services, 2011 Study funded by: To be cited as: Wilson, R.M., P. Landolt, Y.B. Shakya, G. Galabuzi, Z. Zahoorunissa, D. Pham, F. Cabrera, S. Dahy, and M-P. Joly. (2011). Working Rough, Living Poor: Employment and Income Insecurities Faced by Racialized Groups in the Black Creek Area and their Impacts on Health. Toronto: Access Alliance Multicultural Health and Community Services. The content for this report was collaboratively analyzed and written by the core team of the Income Security, Race and Health research working group. The research was designed and implemented with valuable feedback from all our Advisory Committee members and other community partners (see list in Acknowledgement section) The views expressed in this report do not necessarily represent the views of The Wellesley Institute or the Metcalf Foundation. Requests for permission and copies of this report should be addressed to: Access Alliance Multicultural Health and Community Services 500-340 College Street Toronto, ON M5S 3G3 Telephone: (416) 324-8677 Fax: (416) 324-9074 www.accessalliance.ca © 2011 Access Alliance Multicultural Health and Community Services About the Income Security, Race and Health Research Working Group The Income Security, Race and Health (ISRH) Research Working Group is a interdisciplinary research group comprising of academics, service providers, and peer researchers interested in examining racialized economic and health inequalities. The group was established in Toronto in 2006 under the leadership of Access Alliance. The key goals of the ISRH team are to investigate the systemic causes of growing racialized inequalities in employment and income, and to document the health impacts of these inequalities. -
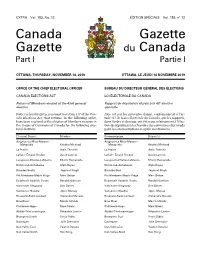
Canada Gazette, Part I
EXTRA Vol. 153, No. 12 ÉDITION SPÉCIALE Vol. 153, no 12 Canada Gazette Gazette du Canada Part I Partie I OTTAWA, THURSDAY, NOVEMBER 14, 2019 OTTAWA, LE JEUDI 14 NOVEMBRE 2019 OFFICE OF THE CHIEF ELECTORAL OFFICER BUREAU DU DIRECTEUR GÉNÉRAL DES ÉLECTIONS CANADA ELECTIONS ACT LOI ÉLECTORALE DU CANADA Return of Members elected at the 43rd general Rapport de député(e)s élu(e)s à la 43e élection election générale Notice is hereby given, pursuant to section 317 of the Can- Avis est par les présentes donné, conformément à l’ar- ada Elections Act, that returns, in the following order, ticle 317 de la Loi électorale du Canada, que les rapports, have been received of the election of Members to serve in dans l’ordre ci-dessous, ont été reçus relativement à l’élec- the House of Commons of Canada for the following elec- tion de député(e)s à la Chambre des communes du Canada toral districts: pour les circonscriptions ci-après mentionnées : Electoral District Member Circonscription Député(e) Avignon–La Mitis–Matane– Avignon–La Mitis–Matane– Matapédia Kristina Michaud Matapédia Kristina Michaud La Prairie Alain Therrien La Prairie Alain Therrien LaSalle–Émard–Verdun David Lametti LaSalle–Émard–Verdun David Lametti Longueuil–Charles-LeMoyne Sherry Romanado Longueuil–Charles-LeMoyne Sherry Romanado Richmond–Arthabaska Alain Rayes Richmond–Arthabaska Alain Rayes Burnaby South Jagmeet Singh Burnaby-Sud Jagmeet Singh Pitt Meadows–Maple Ridge Marc Dalton Pitt Meadows–Maple Ridge Marc Dalton Esquimalt–Saanich–Sooke Randall Garrison Esquimalt–Saanich–Sooke -
Complete Streets Policy & Implementation Guide For
SEVE COMPLETE STREETS POLICY & IMPLEMENTATION GUIDE FOR GREY BRUCE Guide prepared by the Toronto Centre for Active Transportation & MMM Group Ltd. Executive Summary Communities across Canada are adopting policies and guidelines to implement Complete Streets, which are streets designed for all ages, abilities and modes of travel, and provide safe and comfortable access for all users. While Complete Streets are typically considered in an urban context, there is an increasing demand to create physical environments that support active living in rural communities as well. This requires understanding and addressing the unique characteristics and needs of both the urban and rural landscapes, and connectivity between them. Several factors within Grey and Bruce Counties support consideration of Complete Streets, such as: an aging population high rates of physical inactivity high rates of motor vehicle usage growing interest and participation in cycling for transportation and tourism There is a growing body of evidence about the health, safety and environmental benefits of Complete Streets. There are also economic and business benefits, as streetscapes that incorporate cyclist- and pedestrian-friendly features have been shown to increase property values, promote tourism and lower maintenance and operations costs for municipalities. While there are challenges within Grey and Bruce Counties (such as expansive distances that facilitate auto-dependency and cold snowy King Street in Kitchener, Ontario is an example of a Complete Street, as it winters) there are nonetheless many context-sensitive incorporates wide sidewalks, public spaces opportunities to encourage active transportation, such as and cycling infrastructure. enhancing connectivity to existing trails and shorelines, Source: http://completestreetsforcanada.ca/ examples/king-street-kitchener GREY BRUCE COMPLETE STREETS POLICY & IMPLEMENTATION GUIDE | MARCH 2015 2 promoting tourism in all seasons, and piloting new ways to revitalize main streets in support of local businesses. -

List of Mps on the Hill Names Political Affiliation Constituency
List of MPs on the Hill Names Political Affiliation Constituency Adam Vaughan Liberal Spadina – Fort York, ON Alaina Lockhart Liberal Fundy Royal, NB Ali Ehsassi Liberal Willowdale, ON Alistair MacGregor NDP Cowichan – Malahat – Langford, BC Anthony Housefather Liberal Mount Royal, BC Arnold Viersen Conservative Peace River – Westlock, AB Bill Casey Liberal Cumberland Colchester, NS Bob Benzen Conservative Calgary Heritage, AB Bob Zimmer Conservative Prince George – Peace River – Northern Rockies, BC Carol Hughes NDP Algoma – Manitoulin – Kapuskasing, ON Cathay Wagantall Conservative Yorkton – Melville, SK Cathy McLeod Conservative Kamloops – Thompson – Cariboo, BC Celina Ceasar-Chavannes Liberal Whitby, ON Cheryl Gallant Conservative Renfrew – Nipissing – Pembroke, ON Chris Bittle Liberal St. Catharines, ON Christine Moore NDP Abitibi – Témiscamingue, QC Dan Ruimy Liberal Pitt Meadows – Maple Ridge, BC Dan Van Kesteren Conservative Chatham-Kent – Leamington, ON Dan Vandal Liberal Saint Boniface – Saint Vital, MB Daniel Blaikie NDP Elmwood – Transcona, MB Darrell Samson Liberal Sackville – Preston – Chezzetcook, NS Darren Fisher Liberal Darthmouth – Cole Harbour, NS David Anderson Conservative Cypress Hills – Grasslands, SK David Christopherson NDP Hamilton Centre, ON David Graham Liberal Laurentides – Labelle, QC David Sweet Conservative Flamborough – Glanbrook, ON David Tilson Conservative Dufferin – Caledon, ON David Yurdiga Conservative Fort McMurray – Cold Lake, AB Deborah Schulte Liberal King – Vaughan, ON Earl Dreeshen Conservative -

Directory of Family Health Team Websites
Directory of Family Health Team websites FHT Name FHT's web address Municipality Parry Sound- Algonquin FHT http://www.algonquinfht.ca/ Muskoka Renfrew-Nipissing- Algonquins of Pikwakanagan FHT http://ottawa.cioc.ca/record/OCR1945 Pembroke Alliston FHT http://centraleastontario.cioc.ca/record/ALL0430 Simcoe-Grey Amherstburg FHT http://www.afht.ca/ Essex Timiskaming- Anson General FHT http://www.micsgroup.com/Site_Published/Micsgroup/anson_family_pgms.aspx Cochrane Renfrew-Nipissing- Arnprior and District FHT http://arnpriorfht.ca/ Pembroke Athens District FHT www.mydoctor.ca/adfht Leeds-Grenville Thunder Bay- Atikokan FHT http://www.atikokanfht.com/ Atikokan Aurora-Newmarket FHT http://www.auroranewmarketfht.com/ Newmarket-Aurora Baawaating FHT https://sites.google.com/site/baawaatingfht/home Algoma-Manitoulin Prince Edward- Bancroft FHT http://bancroftfht.com/ Hastings Barrie FHT http://www.barriefht.ca/ Barrie Niagara West- Beamsville FHT https://groups.ontariomd.ca/groups/bmc_fht Glanbrook Blue Sky FHT http://www.blueskyfht.com/ Nipissing Bluewater Area FHT http://www.bluewaterareafht.ca/ Huron-Bruce Bridgepoint FHT http://www.bridgepointhealth.ca/fht Toronto-Danforth Northumberland- Brighton/Quinte West FHT http://www.bqwfht.ca/ Quite West Brockton and Area FHT http://www.bafht.com/ Huron-Bruce Bruyere Academic FHT http://www.bruyere.org/bins/content_page.asp?cid=8-6816&lang=1 Ottawa-Vanier Parry Sound- Burk's Falls FHT http://www.mahc.ca/Content.cfm?C=6167&SC=1&SCM=0&MI=4179&L1M=4150 Muskoka Burlington FHT Burlington CANES FHT http://www.canes.on.ca/Default.aspx?tabid=1627 -

2018 Election Liberal Party of Ontario Candidates
2018 Election Liberal Party of Ontario Candidates NAME RIDING WEBSITE LINK Joe Dickson Ajax [email protected] Naheed Yaqubian Aurora-Oak Ridges- [email protected] Richmond Hill Ann Hoggarth Barrie-Innisfil [email protected] Robert Quaiff Bay of Quinte [email protected] Arthur Potts Beaches-East York [email protected] Safdar Hussain Brampton Centre [email protected] Dr. Parminder Singh Brampton East [email protected] Harinder Malhi Brampton North [email protected] Sukhwant Thethi Brampton South [email protected] Vic Dhillon Brampton West [email protected] Ruby Toor Brantford-Brant [email protected] Francesca Dobbyn Bruce-Grey-Owen Sound [email protected] Eleanor McMahon Burlington [email protected] Kathryn McGarry Cambridge [email protected] Theresa Qadri Carleton [email protected] Margaret Schleier Stahl Chatham-Kent-Leamington [email protected] Cristina Martins Davenport [email protected] Michael Coteau Don Valley East [email protected] Shelley Carroll Don Valley North [email protected] Kathleen Wynne Don Valley West [email protected] Bob Gordanier Dufferin-Caledon [email protected] Granville Anderson Durham [email protected] 1 | P a g e NAME RIDING WEBSITE LINK Mike Colle Eglinton-Lawrence [email protected] Carlie Forsythe -

Legislative Assembly of Ontario INDIVIDUAL MEMBERS
Legislative Assembly of Ontario INDIVIDUAL MEMBERS' EXPENDITURES FOR THE FISCAL YEAR 2020 - 2021 PREPARED FOR THE SPEAKER: HON. TED ARNOTT FINANCIAL SERVICES JUNE 2021 CE DOCUMENT EST ÉGALEMENT PUBLIÉ EN FRANÇAIS MEMBERS' TRAVEL AND TORONTO ACCOMMODATION EXPENSES 2020-2021 TRAVEL BETWEEN TRAVEL RESIDENCE AND QUEEN'S ASSEMBLY FAMILY TOTAL WITHIN TORONTO PARK TRAVEL TRAVEL POINTS RIDING ACCOMMODATION TOTAL (includes committee) MEMBER RIDING (1) (2) (3) (4) (5) (6) $ $ $ $ $$ ANAND, DEEPAK 2,459 37 1.0 2,789 5,285 Mississauga -- Malton ANDREW, JILL 2,179 1,751 1.0 3,930 Toronto -- St. Paul's ARMSTRONG, TERESA J. 3,557 23,294 26,851 London -- Fanshawe ARNOTT, HON. TED 4,603 286 4,889 Wellington -- Halton Hills ARTHUR, IAN 3,962 13 27,062 31,038 Kingston and the Islands BABER, ROMAN York Centre BABIKIAN, ARIS Scarborough -- Agincourt BAILEY, ROBERT 6,590 836 24,750 32,176 Sarnia -- Lambton BARRETT, TOBY 1,302 2,802 16,953 21,057 Haldimand -- Norfolk BEGUM, DOLY Scarborough Southwest BELL, JESSICA University -- Rosedale BERNS-MCGOWN, RIMA Beaches -- East York BETHLENFALVY, HON. PETER Pickering -- Uxbridge BISSON, GILLES 25,080 4,985 25,380 55,445 Timmins BLAIS, STEPHEN 11,428 0.5 27,384 38,812 Orléans BOUMA, WILL 1,589 34 1.0 159 28,056 29,838 Brantford -- Brant BOURGOUIN, GUY 11,153 1.0 7,802 28,207 47,162 Mushkegowuk -- James Bay (N) BURCH, JEFF 2,513 26,428 28,942 Niagara Centre CALANDRA, HON. PAUL 4,773 4,773 Markham -- Stouffville Page 1 MEMBERS' TRAVEL AND TORONTO ACCOMMODATION EXPENSES 2020-2021 TRAVEL BETWEEN TRAVEL RESIDENCE AND QUEEN'S ASSEMBLY FAMILY TOTAL WITHIN TORONTO PARK TRAVEL TRAVEL POINTS RIDING ACCOMMODATION TOTAL (includes committee) MEMBER RIDING (1) (2) (3) (4) (5) (6) $ $ $ $ $$ CHO, HON. -

Download the Toronto PATH Map
Whatever your destination... ...PATH signs lead the way. On the PATH Map Squares represent buildings. M The Green Line represents links between and through buildings. Colours represent the four points of the compass – Toronto’s north (blue), south (red), east (yellow), and west (orange). Downtown Walkway H represents hotel. C represents cultural building. S represents sports venue. represents tourist attraction Adelaide Place F-9, G-9 MetLife Place M-11 11 Adelaide St. West L-10 MetroCentre B-12 1 Adelaide St. East N-10 Metro Hall B-12 PATH Marker Welcome to PATH – 105 Adelaide St. West I-10 Metro Toronto Convention Centre B-16, C-18 Signs ranging from 130 Adelaide St. West H-9 Munich Re Centre (390 Bay Street) J-7 Toronto’s Downtown Walkway Air Canada Centre J-17 free-standing outdoor pylons linking 27 kilometres of under- Allen Lambert Galleria One Dundas West M-3 to door decals identify entrances (Brookfield Place) L-15 One Queen Street East N-7 ground shopping, services and Atrium on Bay K-2 Osgoode Subway Station E-6 to the walkway. entertainment Bank of Nova Scotia K-11 Parking, City Hall I-6 220 Bay J-13 Parking, University Avenue F-15 In many elevators there is 390 Bay (Munich Re Centre) J-7 Plaza at Sheraton Centre, The H-7 Bay Adelaide Centre L-8 a small PATH logo mounted Bay East Teamway K-16 1 Queen Street East N-7 beside the button for the floor Bay Wellington Tower K-14 2 Queen Street East N-6 Bay West Teamway J-16 Queen Subway Station N-6 leading to the walkway. -

Votes & Proceedings
Legislative Assemblée Assembly législative of Ontario de l’Ontario Votes and Proceedings Procès-verbaux No. 1 No 1 1st Session 1re session 42nd Parliament 42e législature Wednesday Mercredi July 11, 2018 11 juillet 2018 2 10:00 A.M. 10 H 00 (Great Seal of Ontario) (Grand sceau de l’Ontario) V. ELIZABETH DOWDESWELL V. ELIZABETH DOWDESWELL ELIZABETH THE SECOND, by the Grace of ELIZABETH DEUX, par la grâce de Dieu, God of the United Kingdom, Canada and Her Reine du Royaume-Uni, du Canada et de ses other Realms and Territories Queen, Head of autres royaumes et territoires, Chef du the Commonwealth, Defender of the Faith. Commonwealth, Défenseur de la Foi. Caroline Mulroney Caroline Mulroney Attorney General Procureur général The First Session of the 42nd Parliament of the Que la première session de la 42e législature Province of Ontario be convened for the actual de la province de l’Ontario soit convoquée en dispatch of business at 10:00 am on vue d’expédier les affaires à 10 heures, le Wednesday, the 11th day of July, 2018. mercredi 11 juillet 2018. WITNESS: TÉMOIN : THE HONOURABLE L’HONORABLE V. ELIZABETH DOWDESWELL V. ELIZABETH DOWDESWELL LIEUTENANT GOVERNOR OF OUR LIEUTENANTE-GOUVERNEURE DE PROVINCE OF ONTARIO NOTRE PROVINCE DE L’ONTARIO GIVEN at Toronto, Ontario, on July 5, 2018. FAIT à Toronto (Ontario) le 5 juillet 2018. BY COMMAND PAR ORDRE TODD SMITH TODD SMITH Minister of Government and Consumer ministre des Services gouvernementaux et des Services Services aux consommateurs ____________ This being the first day of the First Session of the Forty-Second Parliament convoked by Proclamation of the Lieutenant Governor to take part in the business of the Legislative Assembly, the Clerk of the Legislative Assembly laid upon the Table a Roll, hereinafter fully set out, containing a list of the names of the members who had been returned at the General Election to serve in this Parliament. -

Ontario MPP Contact Information
Ontario MPP Contact Information Riding MPP Political Party Constituency Mailing Address Queen's Park Address Ajax--Pickering Liberal Suite 201A Ministry of Northern Development and 50 Commercial Avenue Mines Ajax, Ontario, L1S 2H5 Room 5501, 5th Floor, Whitney Block 99 Wellesley Street West Toronto, Ontario, M7A 1W3 Dickson, Joe Algoma--Manitoulin NDP Unit 310, Lester B Pearson Civic Ctr. Room 160, Main Legislative Building, 255 Highway 108 North Queen's Park Elliot Lake, Ontario, P5A 2T1 Toronto, Ontario, M7A 1A5 Mantha, Michael Ancaster--Dundas--Flamborough--Westdale Liberal 299 Dundas Street East Ministry of Municipal Affairs and P.O. BOX 1240 Housing Waterdown, Ontario, L0R 2H0 17th Floor 777 Bay Street McMeekin, Hon Ted Toronto, Ontario, M5G 2E5 Barrie Liberal Unit 14 Ministry of Labour 20 Bell Farm Road 14th Floor Barrie, Ontario, L4M 6E4 400 University Avenue Hoggarth, Ann Toronto, Ontario, M7A 1T7 Beaches--East York Liberal 1821 Danforth Avenue Ministry of Agriculture, Food and Rural Toronto, Ontario, M4C 1J2 Affairs 11th Floor 77 Grenville Street Potts, Arthur Toronto, Ontario, M5S 1B3 Bramalea--Gore--Malton NDP Unit 18 Room 172, Main Legislative Building, 470 Chrysler Drive Queen's Park Singh, Jagmeet Brampton, Ontario, L6N 0C1 Toronto, Ontario, M7A 1A5 Brampton West Liberal Suite 304 Ministry of Aboriginal Affairs 37 George Street North Suite 400 Brampton, Ontario, L6X 1R5 160 Bloor Street East Dhillon, Vic Toronto, Ontario, M7A 2E6 If you are unsure which riding you live in, please contact Elections Ontario: 1-888-668-8683;