Sterile Technique: Key Concepts and Practices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infection Control in Dentistry: How to Asepsis Photographic Mirrors?
Infection control in dentistry: how to asepsis photographic mirrors? Amanda Osório Ayres de Freitas* Mariana Marquezan* Giselle Naback Lemes Vilani* Rodrigo César Santiago* Luiz Felipe de Miranda Costa* Sandra Regina Torres** Abstract: The aim of this study was to evaluate the efficacy of six different methods of disinfection and sterilization of intraoral photographic mirrors through microbiological testing and to analysis their potential harm to mirrors’ surface. Fourteen occlusal mirrors were divided into seven groups. Group 1 comprised two mirrors as received from manufacturer. The other six groups comprised mirrors disinfected/sterilized by autoclave, immersion in enzymatic detergent, and friction with chlorhexidine detergent, chlorhexidine wipes, common detergent and 70% ethylic alcohol. Microbiological and quality surface analyses were performed. Sterilization in autoclave was microbiologic effective, but caused damage to the mirror surface. Chlorhexidine (in wipes or detergent) and liquid soap were effective disinfectant agents for photographic mirrors decontamination, without harmful effect on its surface. Enzymatic detergent immersion and friction with 70% ethylic alcohol were not effective as disinfectant agents for photographic mirrors decontamination. According to the results, the more effective and safe methods for photographic mirrors disinfection were friction with chlorhexidine wipes or detergent, as well as liquid soap. Results, the most efficacious methods for photographic mirrors disinfection were friction with chlorhexidine wipes and detergent, as well as common detergent. Descriptors: Dental Instruments; Decontamination; Microbiology; Surface Properties. *Doutoranda em Odontologia na Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil **Pósdoutora em odontologia pela University of Washington (UW), Seattle, WA, Estados Unidos ISSN 22365843 │ 93 Introduction Dental photography is an important tool for diagnostic and treatment planning, and it’s also a registration of the patient’s condition before and after treatment. -

A Study of Rawitz's 'Inversion Staining' by ALEKSANDRA PRZEL^CKA
231 A Study of Rawitz's 'Inversion Staining' By ALEKSANDRA PRZEL^CKA {From the Cytological Laboratory, Department of Zoology, University Museum, Oxford, and the Nencki Institute, 3 Pasteur St., Warsaw 22; present address, Nencki Institute) SUMMAHY The Rawitz method involves mordanting with tannic acid and potassium antimony tartrate, and staining with basic fuchsine. The mordanting causes basic fuchsine to act as though it were an acid dye ('inversion staining'). A modification of the method is described in the present paper. This modification makes it possible to obtain the same results in a shorter time. The chief substances stained by Rawitz's method are phospholipids, certain pro- teins, and certain polysaccharides. Although the method cannot be regarded as a cytochemical test in the strict sense, yet it gives useful indications of chemical composition and in addition is valuable to the morphological cytologist as a technique for showing certain cytoplasmic inclusions (mitotic spindle, acrosome, mitochondria, 'Golgi apparatus' of certain cells). INTRODUCTION T is well known that the so-called 'Golgi apparatus' is extremely difficult to I reveal by any staining method. Baker, in the course of his investigation on this organelle in the epididymis of the mouse, found that it can be stained by basic fuchsin after a special mordanting process (1957). The method was taken from Rawitz (1895), who found that basic fuchsin, if mordanted with tannic acid and potassium antimony tartrate, loses the character of a dye for chro- matin and colours the cytoplasm instead. Rawitz called this effect 'inversion staining'. Since this technique, when applied to various kinds of cytological material, gave good selectivity in visualizing certain delicate cell structures, it seemed interesting to investigate the nature of the chemical compounds which are responsible for positive Rawitz staining. -

Eosin Staining
Science of H & E Andrew Lisowski, M.S., HTL (A.S.C.P.) 1 Hematoxylin and Eosin Staining “The desired end result of a tissue stained with hematoxylin and eosin is based upon what seems to be almost infinite factors. Pathologists have individual preferences for section thickness, intensities, and shades. The choice of which reagents to use must take into consideration: cost, method of staining, option of purchasing commercially-prepared or technician-prepared reagents, safety, administration policies, convenience, availability, quality, technical limitations, as well as personal preference.” Guidelines for Hematoxylin and Eosin Staining National Society for Histotechnology 2 Why Do We Stain? In order to deliver a medical diagnosis, tissues must be examined under a microscope. Once a tissue specimen has been processed by a histology lab and transferred onto a glass slide, it needs to be appropriately stained for microscopic evaluation. This is because unstained tissue lacks contrast: when viewed under the microscope, everything appears in uniform dull grey color. Unstained tissue H&E stained tissue 3 What Does "Staining" Do? . Contrasts different cells . Highlights particular features of interest . Illustrates different cell structures . Detects infiltrations or deposits in the tissue . Detect pathogens Superbly contrasted GI cells Placenta’s large blood H&E stain showing extensive vessels iron deposits There are different staining techniques to reveal different structures of the cell 4 What is H&E Staining? As its name suggests, H&E stain makes use of a combination of two dyes – hematoxylin and eosin. It is often termed as “routine staining” as it is the most common way of coloring otherwise transparent tissue specimen. -

Laboratory Exercises in Microbiology: Discovering the Unseen World Through Hands-On Investigation
City University of New York (CUNY) CUNY Academic Works Open Educational Resources Queensborough Community College 2016 Laboratory Exercises in Microbiology: Discovering the Unseen World Through Hands-On Investigation Joan Petersen CUNY Queensborough Community College Susan McLaughlin CUNY Queensborough Community College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/qb_oers/16 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Laboratory Exercises in Microbiology: Discovering the Unseen World through Hands-On Investigation By Dr. Susan McLaughlin & Dr. Joan Petersen Queensborough Community College Laboratory Exercises in Microbiology: Discovering the Unseen World through Hands-On Investigation Table of Contents Preface………………………………………………………………………………………i Acknowledgments…………………………………………………………………………..ii Microbiology Lab Safety Instructions…………………………………………………...... iii Lab 1. Introduction to Microscopy and Diversity of Cell Types……………………......... 1 Lab 2. Introduction to Aseptic Techniques and Growth Media………………………...... 19 Lab 3. Preparation of Bacterial Smears and Introduction to Staining…………………...... 37 Lab 4. Acid fast and Endospore Staining……………………………………………......... 49 Lab 5. Metabolic Activities of Bacteria…………………………………………….…....... 59 Lab 6. Dichotomous Keys……………………………………………………………......... 77 Lab 7. The Effect of Physical Factors on Microbial Growth……………………………... 85 Lab 8. Chemical Control of Microbial Growth—Disinfectants and Antibiotics…………. 99 Lab 9. The Microbiology of Milk and Food………………………………………………. 111 Lab 10. The Eukaryotes………………………………………………………………........ 123 Lab 11. Clinical Microbiology I; Anaerobic pathogens; Vectors of Infectious Disease….. 141 Lab 12. Clinical Microbiology II—Immunology and the Biolog System………………… 153 Lab 13. Putting it all Together: Case Studies in Microbiology…………………………… 163 Appendix I. -

CARBOL FUCHSIN STAIN (ZIEHL-NEELSEN) - for in Vitro Use Only - Catalogue No
CARBOL FUCHSIN STAIN (ZIEHL-NEELSEN) - For in vitro use only - Catalogue No. SC24K Our Carbol Fuchsin (Ziehl-Neelsen) Stain is Formulation per 100 mL used in the microscopic detection of acid-fast microorganisms such as Mycobacterium . SC25 Carbol Fuchsin Stain (Ziehl-Zeelsen) Acid-fast organisms such as Mycobacterium Basic Fuchsin ..................................................... 0.3 g have cell walls that are resistant to conventional Phenol ................................................................ 5.0 g staining by aniline dyes such as the Gram stain. Ethanol ............................................................ 10 mL However methods that promote the uptake of dyes De-ionized Water ............................................. 90 mL are available; once stained these organisms are not easily decolorized even with acid-alcohol or acid- SC26 Carbol Fuchsin Decolorizer acetone solutions therefore they are described as Hydrochloric Acid .......................................... 3.0 mL acid-fast. Their resistance to destaining is a useful Ethanol .......................................................... 97.0 mL characteristic in differentiating these organisms from contaminating organisms and host cells. SC27 Carbol Fuchsin Counterstain (Methylene Blue) The Ziehl-Neelsen staining procedure is often Methylene Blue ................................................. 0.3 g referred to as hot carbolfuchsin because of the need De-ionized Water ............................................100 mL to apply heat during the staining -

Hematoxylin & Eosin
Washington University School of Medicine Neuromuscular Lab CAP: 1923316 CLIA: 26D0652044 NY: PFI 3499 HEMATOXYLIN & EOSIN (H & E) STAIN PROTOCOL PRINCIPLE: This protocol is applied in the routine staining of cationic and anionic tissue components in tissue sections. This is the standard reference stain used in the study of histochemical tissue pathology. SPECIMEN REQUIRED: Snap frozen human striated muscle. (Use the 2-methylbutane freezing method) METHOD: Fixation: None. Use snap frozen tissue. Technique: Cut 10 - 16 micron (12 µm) sections in cryostat from snap frozen biopsy. Attach first and last sections to a Superfrost Plus microscope slide. Equipment: Ceramic staining rack - Thomas Scientific #8542-E40 Columbia staining dish - Thomas Scientific #8542-C12 Columbia staining dish(jar) - Thomas Scientific #8542-E30 Forceps Latex gloves Reagents: Reagent alcohol - HPLC Fisher A995-4 or histological A962, FLAMMABLE store at room temp. in a flammable cabinet Eosin Y, disodium salt (Sigma #E-6003, store at room temperature) Harris Hematoxylin Stain, acidified (Lerner Laboratories #1931382)(R.T.) Permount - Fisher SP15-100, FLAMMABLE; HEALTH HAZARD Xylenes (Fisher #HC700-1GAL, FLAMMABLE Solutions: I. Eosin Y, 1 % aqueous (store at room temperature) Eosin Y dye 1 g Deionized water 100 ml H&E protocol.docx 1997 Washington University School of Medicine Neuromuscular Lab CAP: 1923316 CLIA: 26D0652044 NY: PFI 3499 2. Harris Hematoxylin, acidified (store at room temperature) Filter (Baxter #F2217-150, Grade 363, Qualitative) before use 3. Alcohol 50 % reagent alcohol ~50 ml deionized water ~50 ml 4. Alcohol 70 % reagent alcohol ~70 ml deionized water ~30 ml 5. Alcohol 80 % reagent alcohol ~80 ml deionized water ~20 ml 6. -

The Application of Catalase for the Elimination of Hydrogen Peroxide Residues After Bleaching of Cotton Fabrics
Anais da Academia Brasileira de Ciências (2002) 74(3): 433-436 (Annals of the Brazilian Academy of Sciences) ISSN 0001-3765 www.scielo.br/aabc The application of catalase for the elimination of hydrogen peroxide residues after bleaching of cotton fabrics ALEXANDRA M. AMORIM, MARCELO D. G. GASQUES, JÜRGEN ANDREAUS and MAURO SCHARF Department of Chemistry, Universidade Regional de Blumenau, 89010.971 - Blumenau- SC - Brazil Manuscript received on February 19, 2001; accepted for publication on April 27, 2002; presented by Fernando Galembeck ABSTRACT Results of dyeing of cotton fabrics with a bifunctional reactive dye were significantly improved when the fabric after bleaching with hydrogen peroxide was treated with catalase for the elimination of hydrogen peroxide residues from the fabrics. Compared to processes with a varying number of washing steps, with and without commercial reducing agents, the consumption of water could be significantly reduced, without altering the final color shade. Key words: catalase, peroxide bleaching, cotton fabrics, textile chemistry, reactive dye, dyeing. INTRODUCTION (Buschle-Diller et al. 1998), proteases for wool pro- cessing (Heine and Hocke 1995, Bishop et al. 1998), In the last years biotechnological processes are grad- and catalases for hydrogen peroxide removal is still ually invading traditional industries like the textile under investigation, but commercial products are al- industry. In some cases they are substituting tra- ready available (Pacheco 1998, Durán and Durán ditional processes, in other cases biotechnological 2000). products are used to produce new product proper- Reactive dyes of the (Monochlor- and Dich- ties. The principal advantages are associated to less lor-) triazinyl or vinylsulfone type are substantive to severe reaction conditions, lower processing tem- cellulosic fibers under neutral conditions but react peratures and non-toxic and biodegradable products. -
Wright-Giemsa Staining
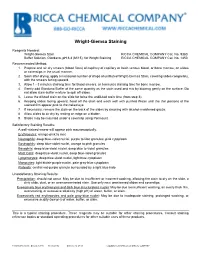
Wright-Giemsa Staining Reagents Needed: Wright-Giemsa Stain RICCA CHEMICAL COMPANY Cat. No. 9380 Buffer Solution, Giordano, pH 6.4 (M/15), for Wright Staining RICCA CHEMICAL COMPANY Cat. No. 1450 Recommended Method: 1. Prepare and air dry smears (blood films) of capillary of capillary or fresh venous blood, or bone marrow, on slides or coverslips in the usual manner. 2. Soon after drying, apply a measured number of drops of undiluted Wright-Giemsa Stain, covering slides completely, with the smears facing upward. 3. Allow 1 - 3 minutes staining time for blood smears, or 5 minutes staining time for bone marrow. 4. Gently add Giordano Buffer of the same quantity as the stain used and mix by blowing gently on the surface. Do not allow stain-buffer mixture to spill off slides. 5. Leave the diluted stain on the slide for twice the undiluted stain time (from step 3). 6. Keeping slides facing upward, flood off the stain and wash well with purified Water until the thin portions of the stained film appear pink to the naked eye. 7. If necessary, remove the stain on the back of the slides by cleaning with alcohol-moistened gauze. 8. Allow slides to air dry by resting an edge on a blotter. 9. Slides may be mounted under a coverslip using Permount. Satisfactory Staining Results: A well-stained smear will appear pink macroscopically. Erythrocytes: orange-pink to rose Neutrophils: deep blue-violet nuclei, purple to lilac granules, pink cytoplasm Eosinophils: deep blue-violet nuclei, orange to pink granules Basophils: deep blue-violet nuclei, deep blue to violet granules Mast Cells: deep blue-violet nuclei, deep blue-violet granules Lymphocytes: deep blue-violet nuclei, light blue cytoplasm Monocytes: light bluish-purple nuclei, pale gray-blue cytoplasm Platelets: central red-purple granule surrounded by a light blue halo Unsatisfactory Staining Results: Precipitation: should not occur. -

ALCIAN BLUE Ph2.5 - ACID MUCOPOLYSACCHARIDES PURPOSE: Alcian Blue Stains Acid Mucosubstances and Acetic Mucins
SURGICAL PATHOLOGY - HISTOLOGY Date: STAINING MANUAL - CARBOHYDRATES Page: 1 of 2 ALCIAN BLUE pH2.5 - ACID MUCOPOLYSACCHARIDES PURPOSE: Alcian blue stains acid mucosubstances and acetic mucins. Excessive amounts of non-sulfated acidic mucosubstances are seen in mesotheliomas, certain amounts occur normally in blood vessel walls but increase in early lesions of atherosclerosis. PRINCIPLE: Alcian blue is a group of polyvalent basic dyes that are water soluble. The blue color is due to the presence of copper in the molecule. The 3% acetic acid solution (pH2.5), Alcian blue stains both sulfated and carboxylated acid mucopolysaccharides and sulfated and carboxylated sialomucins (glycoproteins). It is believed to form salt linkages with the acid groups of acid mucopolysaccharides. CONTROL: Small intestine, appendix, or colon. FIXATIVE: 10% NBF, Bouin’s, or Hollande's. TECHNIQUE: 4m paraffin sections. EQUIPMENT: Rinse glassware in DI water. Coplin jars, pH meter, microwave. REAGENTS: 3% Glacial Acetic Acid Nuclear Fast Red (Kernechtrot): Acetic acid 3.0 ml Aluminum sulfate 25.0 gm Distilled water 100.0 ml Distilled water 500.0 ml Nuclear fast red 0.5 gm Solution is stable for 1 year. Dissolve the aluminum sulfate in CAUTION: Contains acid. the water. Add the nuclear fast red, Alcian Blue Solution: dissolve with aid of heat. Filter, 3% glacial acetic acid 100.0 ml add a crystal of thymol. Stable for Alcian blue 8GX 1.0 gm 1 year. Mix, adjust pH to 2.5, using acetic CAUTION: IRRITANT avoid contact and inhalation acid. Filter, add a crystal of thymol, label with initial and date. Solution is stable for 2 to 6 months. -

Immunofluorescence Staining
ptglab.com 1 The Complete Guide To Optimizing IMMUNOFLUORESCENCE STAINING www.ptglab.com 2 The Complete Guide To Optimizing Immunofluorescence Staining ptglab.com 3 FOREWORD Immunofluorescence (IF) staining is a widely used technique in biological research and clinical diagnostics. IF utilizes fluorescent-labeled antibodies in order to detect specific target antigens. Followed by imaging, it is a very direct technique as you can actually see something. Although it is a well-established tool, multiple factors have to be considered and various optimization steps have to be taken to ensure successful staining. This guide provides not only an introduction to immunofluorescence staining, but also includes protocols and detailed troubleshooting. We discuss and present useful tips for preparing optimal samples that produce the best signal-to-noise ratios for immunofluorescence staining signals. What’s Inside 6–8 General Protocols 9–10 Sample Preparation 11–12 Signal-To-Noise Ratios 13–14 Visualization 15 IF Staining Controls 16 Afterword 17–18 FAQs and Tips 19 Contact Us 4 The Complete Guide To Optimizing Immunofluorescence Staining THE BENCHMARK IN ANTIBODIES Since the day it was founded, Proteintech®* has been making all of its products to the highest standards possible whilst taking complete responsibility for the quality of each product. • Proteintech makes every single antibody in its 12,000+ catalog. • Each Proteintech product is unique and cannot be bought under a different label. • Antibodies are detected with siRNA-treated samples to demonstrate specificity. • It works in every single species and application or get a full money-back refund. Proteintech has over 12,000 antibodies in its extensive catalog, all fully validated and available for next day delivery. -

Acid-Fast Bacteria
SURGICAL PATHOLOGY - HISTOLOGY Date: STAINING MANUAL - MICROORGANISMS Page: 1 of 3 ACID-FAST BACTERIA - ZIEHL-NEELSEN STAIN (AFB) PURPOSE: Used in the demonstration of acid-fast bacteria belonging to the genus 'mycobacterium', which include the causative agent for tuberculosis. PRINCIPLE: The lipoid capsule of the acid-fast organism takes up carbol- fuchsin and resists decolorization with a dilute acid rinse. The lipoid capsule of the mycobacteria is of such high molecular weight that it is waxy at room temperature and successful penetration by the aqueous- based staining solutions (such as Gram's) is prevented. CONTROL: Any tissue containing acid-fast organisms. Use Millipore™ filtered water in the waterbath and staining procedure. FIXATIVE: 10% formalin TECHNIQUE: Cut paraffin sections at 4-5 microns. EQUIPMENT: Rinse all glassware in DI water, coplin jars, microwave oven. REAGENTS: Ziehl-Neelsen Carbol-Fuchsin 1% Acid Alcohol: Solution: Hydrochloric acid 10.0 ml Basic fuchsin 2.5 gm 70% Alcohol 990.0 ml Distilled water 250.0 ml Mix well, label with date and 100% alcohol 25.0 ml initials, stable for 1 year. Phenol crystals, melted 12.5 ml CAUTION: Corrosive. Mix well, filter into brown bottle. Label bottle with date and initials, solution is stable for 1 year. CAUTION: Carcinogen, toxin. MICROOGANISMS ZIEHL-NEELSEN-AFB Page: 2 of 3 Methylene Blue Methylene Blue Stock Solution: Working Solution: Methylene blue 0.7 gm Methylene Blue Stock 5.0 ml Distilled water 50.0 ml Distilled water 45.0 ml Mix well, filter into bottle. Label Pour into coplin jar, stable for 2 with date and initials, stable for 1 months. -

Giemsa: the Universal Diagnostic Stain Shalmica Jackson, Phd1; Daniela Grabis, BS2; Caroline Manav, BS2 1Milliporesigma, St
Giemsa: The Universal Diagnostic Stain Shalmica Jackson, PhD1; Daniela Grabis, BS2; Caroline Manav, BS2 1MilliporeSigma, St. Louis, MO, USA; 2Merck KGaA, Darmstadt, Germany Introduction This poster demonstrates the versatility of the Giemsa stain due to its use in a wide variety of applications, Giemsa is a versatile polychromatic stain, which is including hematology, histology, cytology, bacteriology, suitable for staining a diverse range of specimens. and cytogenetics. In the early 1900s, Gustav Giemsa designed the Giemsa stain to detect parasites such as malaria and Giemsa Applications Treponema pallidum in blood smears. He developed Blood Lavages a “secret” oxidation process using a unique mixture of methylene azure, methylene blue, and eosin, with Bone marrow FNAB (fine needle aspiration biopsy) glycerol added as a stabilizing agent. Sputum Touch preps Paraffin sections (e.g. stomach biopsy for Microorganisms such as Histoplasma, Leishmania, Urine detection of H. pylori) Toxoplasma, and Pneumocystis can also be detected with Giemsa, and in gastric tissues Helicobacter pylori Body effusions Lymph nodes (H. pylori) appear thin and distinctly blue. Giemsa’s Spleen samples Tonsils stain is frequently used for diagnostic purposes in Cytogenetics Karyotyping hematology to differentiate nuclear and cytoplasmic morphology of platelets, RBCs, WBCs, and parasites. It is frequently used in combination with other dye solutions: May-Grünwald’s solution for Pappenheim (MGG) and Wright-Giemsa. The resulting stain can vary Materials and Methods depending on the influence of fixation, staining times, Reagents: Giemsa’s azure methylene blue solution; and the pH values of the solutions or buffers. methanol; 2-propanol; buffer tablets (pH 6.4, 6.8 and 7.2) acc.