Pharmacokinetics and Toxicokinetics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Health Toxicity Values for Perfluorobutane Sulfonic Acid (CASRN 375-73-5) and Related Compound Potassium Perfluorobutane Sulfonate (CASRN 29420 49 3)
EPA-823-R-18-307 Public Comment Draft Human Health Toxicity Values for Perfluorobutane Sulfonic Acid (CASRN 375-73-5) and Related Compound Potassium Perfluorobutane Sulfonate (CASRN 29420-49-3) This document is a Public Comment draft. It has not been formally released by the U.S. Environmental Protection Agency and should not at this stage be construed to represent Agency policy. This information is distributed solely for the purpose of public review. This document is a draft for review purposes only and does not constitute Agency policy. DRAFT FOR PUBLIC COMMENT – DO NOT CITE OR QUOTE NOVEMBER 2018 Human Health Toxicity Values for Perfluorobutane Sulfonic Acid (CASRN 375-73-5) and Related Compound Potassium Perfluorobutane Sulfonate (CASRN 29420 49 3) Prepared by: U.S. Environmental Protection Agency Office of Research and Development (8101R) National Center for Environmental Assessment Washington, DC 20460 EPA Document Number: 823-R-18-307 NOVEMBER 2018 This document is a draft for review purposes only and does not constitute Agency policy. DRAFT FOR PUBLIC COMMENT – DO NOT CITE OR QUOTE NOVEMBER 2018 Disclaimer This document is a public comment draft for review purposes only. This information is distributed solely for the purpose of public comment. It has not been formally disseminated by EPA. It does not represent and should not be construed to represent any Agency determination or policy. Mention of trade names or commercial products does not constitute endorsement or recommendation for use. i This document is a draft for review purposes only and does not constitute Agency policy. DRAFT FOR PUBLIC COMMENT – DO NOT CITE OR QUOTE NOVEMBER 2018 Authors, Contributors, and Reviewers CHEMICAL MANAGERS Jason C. -

Toxicological Review of Phenol
EPA/635/R-02/006 TOXICOLOGICAL REVIEW OF Phenol (CAS No. 108-95-2) In Support of Summary Information on the Integrated Risk Information System (IRIS) September 2002 U.S. Environmental Protection Agency Washington D.C. DISCLAIMER Mention of trade names or commercial products does not constitute endorsement or recommendation for use. Note: This document may undergo revisions in the future. The most up-to-date version will be made available electronically via the IRIS Home Page at http://www.epa.gov/iris. CONTENTS - TOXICOLOGICAL REVIEW FOR PHENOL (CAS No. 108-95-2) Foreword................................................................... vi Authors, Contributors and Reviewers.......................................... vii 1. INTRODUCTION ......................................................1 2. CHEMICAL AND PHYSICAL INFORMATION RELEVANT TO ASSESSMENTS........................................................2 3. TOXICOKINETICS RELEVANT TO ASSESSMENTS ......................5 3.1 Absorption ......................................................5 3.2 Distribution.....................................................10 3.3 Metabolism.....................................................12 3.4 Excretion .......................................................23 4. HAZARD IDENTIFICATION ...........................................24 4.1 Studies in Humans - Epidemiology, Case Reports, Clinical Controls .....25 4.1.1 Oral .....................................................25 4.1.2 Inhalation ................................................27 4.2 -
![The Sensitivity of Young Animals to Benzo[A]Pyrene-Induced Genotoxic Stress](https://docslib.b-cdn.net/cover/6072/the-sensitivity-of-young-animals-to-benzo-a-pyrene-induced-genotoxic-stress-686072.webp)
The Sensitivity of Young Animals to Benzo[A]Pyrene-Induced Genotoxic Stress
The sensitivity of young animals to benzo[a]pyrene-induced genotoxic stress RIVM report 340701002/2013 M. Luijten et al. National Institute for Public Health and the Environment P.O. Box 1 | 3720 BA Bilthoven www.rivm.com The sensitivity of young animals to benzo[a]pyrene-induced genotoxic stress RIVM Report 340701002/2013 RIVM Report 340701002 Colophon © RIVM 2013 Parts of this publication may be reproduced, provided acknowledgement is given to the 'National Institute for Public Health and the Environment', along with the title and year of publication. Mirjam Luijten Lya G. Hernández Edwin P. Zwart Peter M. Bos Harry van Steeg Jan van Benthem Contact: Mirjam Luijten Center for Health Protection [email protected] This investigation has been performed by order and for the account of the Netherlands Food and Consumer Product Safety Authority, within the framework of project V/340701 'CMRI-stoffen in het jonge kind'. RIVM Report 340701002 Abstract Young animals are more sensitive than adult animals to benzo[a]pyrene-induced genotoxic stress Experimental animals are more sensitive at a young age to the adverse effects induced upon benzo[a]pyrene exposure compared to adult animals. In research performed at the RIVM, higher amounts of DNA damage were observed when benzo[a]pyrene was given to experimental animals at a young age. Usually, potential adverse human health effects of environmental chemicals are evaluated in toxicity studies using adult laboratory animals. Children and adults, however, may differ in sensitivity to these adverse effects. Benzo[a]pyrene is commonly found in grilled and broiled foods, tobacco smoke and automobile exhaust fumes. -
TCEQ Guidelines to Develop 24-Hour Inhalation Reference Values
White Paper Final, June 16, 2014 TCEQ Guidelines to Develop 24-Hour Inhalation Reference Values Office of the Executive Director ___________________________________________________________ TEXAS COMMISSION ON ENVIRONMENTAL QUALITY 24-Hour Inhalation Reference Values Page i Document Description and Intended Use This document provides guidelines to develop chemical-specific 24-h reference values (ReVs). It is a supplement to the TCEQ Regulatory Guidance-442 (RG-442), TCEQ Guidelines to Develop Toxicity Factors. For chemicals evaluated in the TCEQ ambient air monitoring network, acute 1-h ReVs and chronic ReVs have generally been derived to evaluate 1-h measured concentrations of chemicals of interest or calculated annual average concentrations, respectively. These averaging times correspond to averaging times evaluated in air permitting. However, 24-h ambient air samples (e.g., 24-h canister samples collected every 3rd or 6th day) may be collected for special projects and also at permanent monitoring sites to calculate annual averages for comparison to chronic ReVs. A 24-h sample is an acute exposure duration significantly longer than 1-hr. Toxic effects induced by 24-h exposure may be governed by modes of action somewhat different than those influencing toxicity due to 1-h or chronic exposure. Therefore, it is not appropriate to use a short-term, 1-h ReV or long-term ReV to evaluate a 24-h ambient air sample. Thus, the development of a 24-h ReV would allow the TCEQ to fully evaluate 24-h air monitoring data for possible health concerns and could be used for risk communication purposes. In addition, this information is helpful to risk assessors for performing health effects reviews when 24-h air monitoring data exceed chronic ReVs. -

Tris – (1,3 – Dicholorisopropyl) Phosphate (TDCPP) Toxicological Summary Sheet Minnesota Department of Health April 2013
2013 Health Based Value for Groundwater Health Risk Assessment Unit, Environmental Health Division 651-201-4899 Web Publication Date: April 2013 Expiration Date: April 2018 Chemical Name: Tris – (1,3 – dicholorisopropyl) phosphate CAS: 13674-87-8 Synonyms: Tris(1,3-dichloro-2-propyl)phosphate; Tri[2-chloro-1-(chloromethyl)ethyl] phosphate; Fyrol FR 2; TDCPP; TDCP Acute Non-Cancer Health Based Value (nHBVAcute) = Not Derived (Insufficient Data) Short-term Non-Cancer Health Based Value (nHBVShort-term) = Not Derived (Insufficient Data) Subchronic Non-Cancer Health Based Value (nHBVSubchronic) = 20 ug/L = (Reference Dose, mg/kg/d) x (Relative Source Contribution) x (Conversion Factor) (Subchronic intake rate, L/kg-d) = (0.0067 mg/kg/d) x (0.2) x (1000 ug/mg) (0.077 L/kg-d) = 17 rounded to 20 ug/L Reference Dose/Concentration: 0.0067 mg/kg-d (mice) Source of toxicity value: MDH, 2013 Point of Departure: 15 mg/kg-d (NOAEL from 3 month dietary study by Kamata et al 1989) Human Equivalent Dose (MDH, 2011): 15 x 0.13 = 2.0 mg/kg-d (MDH 2011) Total uncertainty factor: 300 Uncertainty factor allocation: 3 for interspecies differences (for toxicodynamics), 10 for intraspecies variability, and 10 for database uncertainty (to address no or inadequate information regarding developmental/reproductive function, neurological, immune and endocrine effects) Critical effect(s): Increased liver and kidney weights Co-critical effect(s): None Additivity endpoint(s): Hepatic (liver) system, Renal (kidney) system TDCPP - 1 of 6 Chronic Non-Cancer Health Based -

Using in Vitro Toxcast Assays to Evaluate Mechanistic Plausibility
Using In vitro ToxCast Assays to Evaluate Mechanistic Plausibility and Build Confidence in the Selection of Analogues for Quantitative Read-Across: A Case Study on p,p’-Dichlorodiphenyldichloroethane Lucina E. Lizarraga, Jeffry L. Dean, J. Phillip Kaiser, Scott C. Wesselkamper, Jason C. Lambert, Elizabeth O. Owens, Belinda Hawkins, Q. Jay Zhao. National Center for Environmental Assessment (NCEA), U.S. Environmental Protection Agency, Cincinnati, Ohio 45268, USA Lucina E. Lizarraga l [email protected] l 513-487 2648 Overview Bioactivity Similarity Comparisons Evaluating Mechanistic Plausibility for Liver and Reproductive Toxicity • Deriving human health reference values for environmental chemicals has traditionally relied on toxicity data from humans and/or experimental animals p,p’-DDD and Analogues Exhibit Similarities in Cell-specific Responses and Target Gene p,p’-DDD and Analogues Exhibit Similar Upregulation of Steroid/Xenobiotic-sensing Pathways in In Vitro ToxCast Assays Conducted in Human Liver Cells Nuclear Receptors in In Vitro ToxCast Assays Conducted in Hepatoma HepG2 Cells • In the absence of in vivo toxicity data, new approach methodologies such as read-across can be used to fill data gaps for a target chemical using known information from a source analogue Figure 2. Bioactivity data for p,p’-DDD and Analogues in ToxCast Assays Conducted in • A read-across approach illustrated below (Figure 1) was applied to assist in screening-level Human Hepatoma HepG2 Cells and Primary assessment of noncancer oral toxicity for the target, p,p’-DDD, a data-poor chemical known to occur Human Hepatocytes. Scatterplots show AC50 and at contaminated sites in the U.S. scaled activity values for p,p’-DDD, p,p’-DDT, p,p’- DDE and methoxychlor from in vitro assays visualized according to the type of biological response or biological target. -

Studies to Evaluate the Safety of Residues of Veterinary Drugs in Human Food: General Approach to Establish an Acute Reference Dose (Arfd)
#232 STUDIES TO EVALUATE THE SAFETY OF RESIDUES OF VETERINARY DRUGS IN HUMAN FOOD: GENERAL APPROACH TO ESTABLISH AN ACUTE REFERENCE DOSE (ARFD) Guidance for Industry VICH GL54 Submit comments on this guidance at any time. Submit electronic comments to https://www.regulations.gov. Submit written comments to the Dockets Management Staff (HFA-305), Food and Drug Administration, 5630 Fishers Lane, Room 1061, Rockville, MD 20852. Identify all comments with the Docket No. FDA-2015-D-1804. For further information regarding this document, contact [email protected]. Additional copies of this guidance document may be requested from the Policy and Communications Staff (HFV-6), Center for Veterinary Medicine, Food and Drug Administration, 7500 Standish Place, Rockville, MD 20855, and may be viewed on the Internet at either https://www.fda.gov/AnimalVeterinary/default.htm or https://www.regulations.gov. U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine August 2017 Contains Non-Binding Recommendations VICH GL54 (SAFETY) – ARfD For Implementation at Step 7 STUDIES TO EVALUATE THE SAFETY OF RESIDUES OF VETERINARY DRUGS IN HUMAN FOOD: GENERAL APPROACH TO ESTABLISH AN ACUTE REFERENCE DOSE (ARFD) Adopted at Step 7 of the VICH Process by the VICH Steering Committee in November 2016 for implementation by November 2017. This Guidance has been developed by the appropriate VICH Expert Working Group and has been subject to consultation by the parties, in accordance with the VICH Process. At Step 7 of the Process the final draft is recommended for adoption to the regulatory bodies of the European Union, Japan and USA. -

Toxicological Principles Click to Edit Master Text Styles Module 2 Objectives
Accessible version can be found here: https://www.cdc.gov/nceh/hsb/elearning/toi/Mod2/ Toxicological Outbreak Investigation Course Module Two: Toxicological Principles Click to edit Master text styles Module 2 Objectives Distinguish characteristics of an outbreak caused by a toxic agent Define toxidromes Identify the factors affecting toxicity Describe toxicokinetic principles of absorption, distribution, metabolism, and elimination 2 Click to edit Master text styles Background Levels of Toxic Agents . People are continuously exposed to different toxic agents. Toxic agent exposures depend on… . Where you live. What you do. What you eat. 3 Click to edit Master text styles Hypothetical Laboratory Results from a Healthy Adult . If a person living in the United States is tested randomly for heavy metals, a portion of their results might look like this 4 Click to edit Master text styles Hypothetical Laboratory Results from a Healthy Adult (cont.) . Individuals may have detectable levels of chemicals indicating background exposures in the body without having any signs of illness. These background levels can vary depending on a person’s diet, occupation, and other factors. 5 Click to edit Master text styles Outbreak Scenario What is the cause? . You receive a phone call regarding a situation in Is this from a potentially which a dozen agricultural toxic exposure? workers are developing: . Nausea How might you be able to . Vomiting distinguish a toxic . Sweating exposure from other . Dizziness etiologies? . Difficulty breathing 6 Click to edit Master text styles How to Distinguish a Toxic Agent Outbreak . Outbreaks that are caused by a toxic agent usually share some key characteristics that may aid in distinguishing a toxicological etiology from other etiologies (i.e. -

Toxin Types, Toxicokinetics and Toxicodynamics
Chapter 16: Toxin types, toxicokinetics and toxicodynamics Andrew Humpage1,2,3 1Australian Water Quality Centre, PMB 3, Salisbury, Adelaide, SA 5108, Australia. 2Discipline of Pharmacology, School of Medical Sciences, Uni- versity of Adelaide, SA 5005, Australia. 3Cooperative Research Centre for Water Quality and Treatment, PMB 3, Salisbury, Adelaide, SA 5108, Aus- tralia. Introduction Cyanobacteria produce a wide array of bioactive secondary metabolites (see Table A.1 in Appendix A), some which are toxic (Namikoshi and Rinehart 1996; Skulberg 2000). Those toxic to mammals include the mi- crocystins, cylindrospermopsins, saxitoxins, nodularins, anatoxin-a, ho- moanatoxin-a, and anatoxin-a(s). It has been recently suggested that β- methylamino alanine (BMAA) may be a new cyanobacterial toxin (Cox et al. 2003; Cox et al. 2005). The public health risks of cyanotoxins in drink- ing water have recently been reviewed (Falconer and Humpage 2005b). The aim of this paper is to concisely review our current knowledge of their acute toxicity, mechanisms of action, toxicokinetics and toxicodynamics. Microcystins Microcystins (MCs) are a group of at least 80 variants based on a cyclic heptapeptide structure (Fig. 1). All toxic microcystin structural variants contain a unique hydrophobic amino acid, 3-amino-9-methoxy-10-phenyl- 2,6,8-trimethyl-deca-4(E),6(E)-dienoic acid (ADDA). The prototype- compound is MC-LR, which has leucine and arginine at the two hypervari- able positions in the ring structure (X and Y, respectively, in Fig. 1). Sub- 384 A. Humpage stitution of other amino acids at these sites, or methylation of residues at other sites, leads to wide structural variability (Namikoshi et al. -
Quantitative Structure-Activity Relationships for Organophosphates Binding to Trypsin and Chymotrypsin
Wright State University CORE Scholar Browse all Theses and Dissertations Theses and Dissertations 2010 Quantitative Structure-Activity Relationships for Organophosphates Binding to Trypsin and Chymotrypsin Christopher Daniel Ruark Wright State University Follow this and additional works at: https://corescholar.libraries.wright.edu/etd_all Part of the Pharmacology, Toxicology and Environmental Health Commons Repository Citation Ruark, Christopher Daniel, "Quantitative Structure-Activity Relationships for Organophosphates Binding to Trypsin and Chymotrypsin" (2010). Browse all Theses and Dissertations. 350. https://corescholar.libraries.wright.edu/etd_all/350 This Thesis is brought to you for free and open access by the Theses and Dissertations at CORE Scholar. It has been accepted for inclusion in Browse all Theses and Dissertations by an authorized administrator of CORE Scholar. For more information, please contact [email protected]. QUANTITATIVE STRUCTURE-ACTIVITY RELATIONSHIPS FOR ORGANOPHOSPHATES BINDING TO TRYPSIN AND CHYMOTRYPSIN A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science By CHRISTOPHER DANIEL RUARK B.S., Miami University, 2007 2010 Wright State University WRIGHT STATE UNIVERSITY SCHOOL OF GRADUATE STUDIES June 28, 2010 I HEREBY RECOMMEND THAT THE THESIS PREPARED UNDER MY SUPERVISION BY Christopher D. Ruark ENTITLED Quantitative Structure-Activity Relationships for Organophosphates Binding to Trypsin and Chymotrypsin BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF Master of Science. ____________________ Jeffery Gearhart, Ph.D. Thesis Director ____________________ James Lucot, Ph.D. Thesis Co-Director ____________________ Mariana Morris, Ph.D. Department Chair Pharmacology and Toxicology Committee on Final Examination: __________________________ Jeffery Gearhart, Ph.D. Thesis Director __________________________ James Lucot, Ph.D. -

Toluene Toxicological Summary August 2020
Health Based Guidance for Water Health Risk Assessment Unit, Environmental Health Division 651-201-4899 Web Publication Date: August 2020 Toxicological Summary for: Toluene CAS: 108-88-3 Synonyms: methyl-Benzene, methylbenzol, monomethyl benzene, phenylmethane, Tol, Toluol, tolu-sol Acute Non-Cancer Health-Based Value (nHBVAcute) = Not Derived (Insufficient Data) Short-term Non-Cancer Health-Based Value (nHBVShort-term) = 70 μg/L (Reference Dose, mg/kg-d) x (Relative Source Contribution) x (Conversion Factor) (Short-term Intake Rate, L/kg-d) = (0.10 mg/kg-d) x (0.2)* x (1000 µg/mg) (0.290 L/kg-d)** = 68.9 rounded to 70 µg/L *Relative Source Contribution: MDH 2008, Section IV.E.1. **Intake Rate: MDH 2008, Section IV.E.1. and US EPA 2019, Exposure Factors Handbook, Tables 3-1, 3-3 and 3-5. Reference Dose/Concentration: HED/Total UF = 3.08/30 = 0.10 mg/kg-d (CD-1 mice) Source of toxicity value: Determined by MDH in 2019 Point of Departure (POD): 22 mg/kg-d (NOAEL; Hsieh, 1989) Dose Adjustment Factor (DAF): 0.14, Body weight scaling, default (USEPA, 2011b) (MDH, 2017) Human Equivalent Dose (HED): POD x DAF = 22 mg/kg-d x 0.14 = 3.08 mg/kg-d Total uncertainty factor (UF): 30 Uncertainty factor allocation: 3 for interspecies differences (for toxicodynamics) and 10 for intraspecies variability Critical effect(s): Immunosuppression Co-critical effect(s): behavior changes due to nervous system effects, neurotransmitter level changes in the brain, changes in immune response Additivity endpoint(s): Immune system, Nervous system Subchronic Non-Cancer Health-Based Value (nHBVSubchronic) = nHBVShort-term = 70 µg/L (Reference Dose, mg/kg-d) x (Relative Source Contribution) x (Conversion Factor) (Subchronic Intake Rate, L/kg-d) Toluene - 1 = (0.18 mg/kg-d) x (0.2)* x (1000 µg/mg) (0.074 L/kg-d)** = 486 rounded to 500 µg/L *Relative Source Contribution: MDH 2008, Section IV.E.1. -
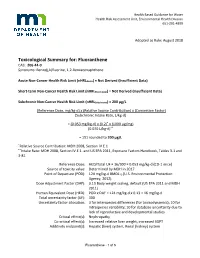
Toxicological Summary for Fluoranthene (PDF)
Health Based Guidance for Water Health Risk Assessment Unit, Environmental Health Division 651-201-4899 Adopted as Rule: August 2018 Toxicological Summary for: Fluoranthene CAS: 206-44-0 Synonyms: Benzo(j,k)fluorine, 1,2-Benzacenaphthene Acute Non-Cancer Health Risk Limit (nHRLAcute) = Not Derived (Insufficient Data) Short-term Non-Cancer Health Risk Limit (nHRLShort-term) = Not Derived (Insufficient Data) Subchronic Non-Cancer Health Risk Limit (nHRLSubchronic) = 200 µg/L (Reference Dose, mg/kg-d) x (Relative Source Contribution) x (Conversion Factor) (Subchronic Intake Rate, L/kg-d) = (0.053 mg/kg-d) x (0.2)* x (1000 µg/mg) (0.070 L/kg-d)** = 151 rounded to 200 µg/L *Relative Source Contribution: MDH 2008, Section IV.E.1. **Intake Rate: MDH 2008, Section IV.E.1. and US EPA 2011, Exposure Factors Handbook, Tables 3-1 and 3-81 Reference Dose: HED/Total UF = 16/300 = 0.053 mg/kg-d (CD-1 mice) Source of toxicity value: Determined by MDH in 2017 Point of Departure (POD): 124 mg/kg-d BMDL10 (U.S. Environmental Protection Agency, 2012) Dose Adjustment Factor (DAF): 0.13 Body weight scaling, default (US EPA 2011 and MDH 2011) Human Equivalent Dose (HED): POD x DAF = 124 mg/kg-d x 0.13 = 16 mg/kg-d Total uncertainty factor (UF): 300 Uncertainty factor allocation: 3 for interspecies differences (for toxicodynamics); 10 for intraspecies variability; 10 for database uncertainty due to lack of reproductive and developmental studies Critical effect(s): Nephropathy Co-critical effect(s): Increased relative liver weight, increased SGPT Additivity endpoint(s): Hepatic (liver) system, Renal (kidney) system Fluoranthene - 1 of 5 Chronic Non-Cancer Health Risk Limit (nHRLChronic) = 70 µg/L (Reference Dose, mg/kg-d) x (Relative Source Contribution) x (Conversion Factor) (Chronic Intake Rate, L/kg-d) = (0.016 mg/kg-d) x (0.2)* x (1000 µg/mg) (0.044 L/kg-d)** = 72.7 rounded to 70 µg/L *Relative Source Contribution: MDH 2008, Section IV.E.1.