(RNAO) – Risk Assessment & Prevention of Pressure Ulcers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Arterial Leg Ulcer Clinical Pathway
Waterloo Wellington Integrated Wound Care Program Evidence-Based Wound Care Arterial Leg Ulcer Clinical Pathway 0-7 Days Expected Outcomes Notes Most Responsible Physician(MRP)/Nurse Practitioner (NP) Refer patient to ‘Care Connects’ if no responsible practitioner currently involved with patient identified/informed Determine if MRP/NP is part of Family Health Team (FHT) or Community Health Centre (CHC) and consider additional supports available Medical/surgical history and co-morbidity management Risk factors include: Chronic renal disease considered within care plan Smoking Congestive heart failure Diabetes mellitus Impaired liver function Hyperlipidemia Use of systemic steroids, Hypertension immunosuppressive and chemotherapy Coronary artery disease >70 years of age History of cerebral vascular accident Age 50-69 years with history of diabetes (CVA) or smoking Low hemoglobin < 50 years with diabetes and one other Obesity atherosclerotic factor Poor nutrition History of vascular surgery or deep vein Decreased thyroid function thrombosis Psoriasis Bleeding disorders Autoimmune diseases Family history of arterial disease Medication reconciliation and their impact on wound healing Prescription, non-prescription, naturopathic and illicit drug use (including e-cigarettes, reviewed inhaled substances and nicotine replacement therapy) Medications that can affect healing include: chemotherapy, anticoagulants, antiplatelets, corticosteroids, vasoconstrictors, antihypertensives, diuretics and immunosepressive drugs Other -
Assessment Module
Assessment Module 1 | Page Assessment May 2017 Table of Contents About this Module/Overview/Objectives……………………………………………...Page 3 Pre-test…………………………………………………………………………………Pages 4-5 Chapter 1……………………………………………………………………………....Pages 6-12 Overview Focused Assessment vs. Comprehensive Assessment Considerations in preparing for a physical exam Geriatric Assessment Nursing Components Considerations in Elderly Residents Chapter 2……………………………………………………………………………...Pages 12-14 Root Cause of Behaviors Physiologic Social Environmental Psychosocial Chapter 3……………………………………………………………………………...Pages 14-16 Risk Assessment Eyes Ears Hemiparesis Paraplegia Where to place the resident in the room Chapter 4……………………………………………………………...………………Pages 16-18 Texas Board of Nursing and Assessments Federal Nursing Facility Regulations F272: Comprehensive Assessments State Nursing Facility Regulations Chapter 5………………………………………………………………………….......Pages 18-19 Resources “This is me” “This is me: My Care Passport” Alternate Communication Boards Pain, Pain Go Away Presentation Appendices……………………………………………………………………………Pages 20-48 2 | Page Assessment May 2017 About this Module: Assessment is a key component of nursing practice, required for planning and the provision of resident and family centered care. Information that is obtained from an accurate assessment serves as the foundation for age-appropriate nursing care, enhancing the residents’ quality of life and independence. The LVN must have a specific set of skills in order to adequately and effectively assess the resident, including: a physical assessment; a functional assessment; and any additional information about the resident that would be used to develop the care plan. This module will provide you with all of the information necessary to ensure adequate assessments are completed for each resident in the facility, meeting the state and federal requirements for resident assessment. Overview: Conditions such as functional impairment and dementia are common in nursing home residents. -

Nursing Students' Perspectives on Telenursing in Patient Care After
Clinical Simulation in Nursing (2015) 11, 244-250 www.elsevier.com/locate/ecsn Featured Article Nursing Students’ Perspectives on Telenursing in Patient Care After Simulation Inger Ase Reierson, RN, MNSca,*, Hilde Solli, RN, MNSc, CCNa, Ida Torunn Bjørk, RN, MNSc, Dr.polit.a,b aFaculty of Health and Social Studies, Institute of Health Studies, Telemark University College, 3901 Porsgrunn, Norway bFaculty of Medicine, Institute of Health and Society, Department of Nursing Science, University of Oslo, 0318 Oslo, Norway KEYWORDS Abstract telenursing; Background: This article presents the perspectives of undergraduate nursing students on telenursing simulation; in patient care after simulating three telenursing scenarios using real-time video and audio nursing education; technology. information and Methods: An exploratory design using focus group interviews was performed; data were analyzed us- communication ing qualitative content analysis. technology; Results: Five main categories arose: learning a different nursing role, influence on nursing assessment qualitative content and decision making, reflections on the quality of remote comforting and care, empowering the pa- analysis tient, and ethical and economic reflections. Conclusions: Delivering telenursing care was regarded as important yet complex activity. Telenursing simulation should be integrated into undergraduate nursing education. Cite this article: Reierson, I. A., Solli, H., & Bjørk, I. T. (2015, April). Nursing students’ perspectives on telenursing in patient care after simulation. Clinical Simulation in Nursing, 11(4), 244-250. http://dx.doi.org/ 10.1016/j.ecns.2015.02.003. Ó 2015 International Nursing Association for Clinical Simulation and Learning. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/ by-nc-nd/4.0/). -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -
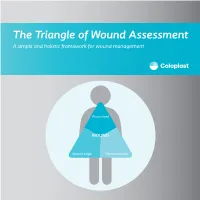
The Triangle of Wound Assessment a Simple and Holistic Framework for Wound Management
The Triangle of Wound Assessment A simple and holistic framework for wound management Wound bed WOUND Wound edge Periwound skin We asked healthcare professionals around the world about their priorities ? for wound care We found that most people Respondents said that treating wounds are not protecting the periwound specialists in a hospital1 skin is very important1 Approximately Up to 79% of wounds are 70% of being treated in wounds are the community2 surrounded by unhealthy skin3 2 ...none However, in a recent met all of the study of 14 wound criteria for assessment tools ... optimal wound assessment4 The Triangle of Wound Assessment is a holistic framework that allows practitioners üto assess and manage all areas of the wound, including the periwound skin. It is a simple and systematic approach that guides the user Wound bed from complete wound WOUND assessment to setting management goals, and Wound edge Periwound skin selecting the optimal treatment. 3 The Triangle of Wound Assessment offers a systematic approach to wound management Optimal wound management starts with a holistic wound assessment. This will help to more efficiently set management goals, which will increase the potential for better treatment outcomes. Assessment Management Goals Treatment 4 This is achieved through a holistic framework The Triangle of Wound Assessment provides a framework to assess all three areas of the wound while remembering the patient behind the wound within their social context. Patient Wound bed Social context WOUND Wound Wound edge Periwound skin 5 It’s not just about the wound but also the patient behind the wound Optimal management of the wound starts with assessing the patient behind the wound, and the social context in which the patient lives. -

Guideline: Wound Bed Preparation for Healable and Non Healable Wounds
British Columbia Provincial Nursing Skin and Wound Committee Guideline: Wound Bed Preparation for Healable and Non Healable Wounds Developed by the BC Provincial Nursing Skin and Wound Committee in collaboration with Wound Clinicians from: / TITLE Guideline: Wound Bed Preparation for Healable and Non-Healable Wounds in Adults & Children1 Practice Level Nurses in accordance with health authority and agency policy. Conservative sharp wound debridement (CSWD) is a restricted activity according to the Nurse’s (Registered) and Nurse Practitioner Regulation. 2 CRNBC states that registered nurses must successfully complete additional education and follow an established guideline when carrying out CSWD. Biological debridement therapy is a restricted activity according to the Nurse’s (Registered) and Nurse Practitioner Regulation. 3 CRNBC states that registered nurses must follow an established guideline when carrying out biological debridement. Clients 4 with wounds needing wound bed preparation require an interprofessional approach to provide comprehensive, evidence-based assessment and treatment. This clinical practice guideline focuses solely on the role of the nurse, as one member of the interprofessional team providing care to these clients. Background Factors affecting wound healability include the presence of adequate circulation in the area of the wound, wound related factors such as the size and duration of the wound, the ability to treat the cause of the wound and the presence of risk factors impacting wound healing. While many wounds heal, others are determined to be non-healing or slow-to-heal based on the presence or absence of these factors. Wound healability must be determined prior to debridement and moist wound healing. Although wound healing normally occurs in a predictable fashion, wound healing trajectories can be heterogeneous and non- uniform resulting is delayed wound healing for some clients. -

Use of Nursing Diagnosis in CA Nursing Schools
USE OF NURSING DIAGNOSIS IN CALIFORNIA NURSING SCHOOLS AND HOSPITALS January 2018 Funded by generous support from the California Hospital Association (CHA) Copyright 2018 by HealthImpact. All rights reserved. HealthImpact 663 – 13th Street, Suite 300 Oakland, CA 94612 www.healthimpact.org USE OF NURSING DIAGNOSIS IN CALIFORNIA NURSING SCHOOLS AND HOSPITALS INTRODUCTION As part of the effort to define the value of nursing, a common language continues to arise as a central issue in understanding, communicating, and carrying out nursing's unique role in identifying and treating patient response to illness. The diagnostic process and evidence-based interventions developed and subsequently implemented by a practice discipline describe its unique contribution, scope of accountability, and value. The specific responsibility registered nurses (RN) have in assessing patient response to health and illness and determining evidence-based etiology is within the realm of nursing’s autonomous scope of practice, and is referred to as nursing diagnosis. It is an essential element of the nursing process and is followed by implementing specific interventions within nursing’s scope of practice, providing evidence that links professional practice to health outcomes. Conducting a comprehensive nursing assessment leading to the accurate identification of nursing diagnoses guides the development of the plan of care and specific interventions to be carried out. Assessing the patient’s response to health and illness encompasses a wide range of potential problems and actual concerns to be addressed, many of which may not arise from the medical diagnosis and provider orders alone, yet can impede recovery and impact health outcomes. Further, it is critically important to communicate those problems, potential vulnerabilities and related plans of care through broadly understood language unique to nursing. -

How to Conduct a Medical Record Review
How to Conduct a Medical Record Review WHITE PAPER Summary: This paper defines a recommended process for medical record review. This includes the important first step of defining the “why” behind the review, and marrying the review outcome to organizational goals. Medical record review is perhaps the core responsibility of the CDI profession- z FEATURES al. Although the numbers vary by facility, CDI specialists review an average of 16–24 patient charts daily, a task that compromises the bulk of their workday Aligning record reviews to (ACDIS, 2016).1 During the review, CDI professionals comb the chart for incom- organizational goals .................2 plete, imprecise, illegible, conflicting, or absent documentation of diagnoses, Principles of record procedures, and treatments, as well as supporting clinical indicators. Their review .......................................3 goal is to cultivate a medical record that stands alone as an accurate story of a ED/EMS notes ..........................5 patient encounter, providing a full picture of the patient’s illness and record of History and physical (H&P) ......6 treatment. A complete record allows for continuity of care, reliable collection of Operative note or bedside mortality and morbidity data, quality statistics, and accurate reimbursement. procedures ...............................7 Diagnostics and medications ...8 In their review of the medical record, CDI professionals aim to reconstruct the Progress notes, consults, and patient story from admission to discharge by examining, understanding, and nursing documentation ............9 synthesizing many puzzle pieces from disparate systems and people. This Initial vs. subsequent process requires considerable clinical acumen, critical thinking akin to detective reviews .....................................9 work, and knowledge of coding guidelines and quality measure requirements. -
Rules and Regulations of Licensed Practical Nurses
RULES OF THE TENNESSEE BOARD OF NURSING CHAPTER 1000-02 RULES AND REGULATIONS OF LICENSED PRACTICAL NURSES TABLE OF CONTENTS 1000-02-.01 Licensure by Examination 1000-02-.09 Schools - Curriculum, Instruction, Evaluation 1000-02-.02 Licensure Without Examination: Interstate 1000-02-.10 Schools - Educational Facilities Endorsement 1000-02-.11 Definitions 1000-02-.03 Biennial Registration (Renewal) 1000-02-.12 Fees 1000-02-.04 Discipline of Licensees, Unauthorized Practice of 1000-02-.13 Unprofessional Conduct and Negligence, Practical Nursing, Civil Penalties, Screening Habits or Other Cause Panels, Subpoenas, Advisory Rulings, Declaratory 1000-02-.14 Standards of Nursing Competence Orders, and Assessment of Costs 1000-02-.15 Scope of Practice 1000-02-.05 Schools - Approval 1000-02-.16 Interstate Nurse Licensure 1000-02-.06 Schools - Philosophy, Purpose, Administration, 1000-02-.17 Free Health Clinic and Volunteer Practice Organization and Finance Requirements 1000-02-.07 Schools - Faculty 1000-02-.18 Advertising 1000-02-.08 Schools - Students 1000-02-.01 LICENSURE BY EXAMINATION. (1) Application - The application form provided by the Board is to be completed in part by the applicant, signed by him, and attested by a notary public. (a) The name as signed by the applicant will be the name carried in the records of the Board. (See 1000-02-03 (3) for name change regulation.) (b) Part of this application is to be completed by an official of the school of practical nursing from which the applicant graduated. (c) The completed application, accompanied by the statutory fee, shall be submitted to the Board. A filing date for the application is set by the Board for each scheduled examination. -

A Focus on the Triangle of Wound Assessment — Addressing the Gap Challenge and Identifying Suspected Biofilm in Clinical Practice
Clinical practice A focus on the Triangle of Wound Assessment — addressing the gap challenge and identifying suspected biofilm in clinical practice Authors: Wound assessment should be comprehensive, systematic and evidence- Caroline Dowsett, Terry Swanson and Tonny Karlsmark based (World Union of Wound Healing Societies [WUWHS], 2016a). The Triangle of Wound Assessment offers clinicians a framework to assess the patient and their wound, taking into consideration the wound bed, wound edge and periwound skin (Dowsett et al, 2015). The framework can be adapted to incorporate new developments and new challenges in wound care such as the ‘gap challenge’ and biofilm prevention and management. Using the framework can assist in determining the status of the wound bed and support clinical decision making to prevent problems associated with exudate pooling at the wound bed and the potential for biofilm formation. he Triangle of Wound Assessment This article will discuss how the Triangle of was established in 2014 and provides Wound Assessment identifies infection and T a systematic approach to wound biofilm, tackles the gap challenge, and how assessment and in setting management goals, this framework can be developed for new to guide optimal treatment choice (Dowsett et challenges in wound care. al, 2015), ensuring that the periwound skin is incorporated into the assessment. Periwound The importance of holistic assessment skin can be a significant problem in patients Wounds are a significant source of cost to with chronic wounds, with between 60–70% patients, as well as to the health economy. of wounds found to be surrounded by either Chronic wounds are often hard to heal problematic or unhealthy periwound skin resulting in a cycle of pain, anxiety and (Cartier et al, 2014). -

Clinician Assessment Tools for Patients with Diabetic Foot Disease: a Systematic Review
Journal of Clinical Medicine Review Clinician Assessment Tools for Patients with Diabetic Foot Disease: A Systematic Review Raúl Fernández-Torres 1 , María Ruiz-Muñoz 1,* , Alberto J. Pérez-Panero 1 , Jerónimo C. García-Romero 2 and Manuel Gónzalez-Sánchez 3 1 Department of Nursing and Podiatry, University of Málaga, Arquitecto Francisco Peñalosa, s/n. Ampliación Campus de Teatinos, 29071 Málaga, Spain; [email protected] (R.F.-T.); [email protected] (A.J.P.-P.) 2 Medical School of Physical Education and Sports, University of Málaga, C/Jiménez Fraud 10. Edificio López de Peñalver, 29010 Málaga, Spain; [email protected] 3 Department of Physiotherapy, University of Málaga, Arquitecto Francisco Peñalosa, s/n. Ampliación campus de Teatinos, 29071 Málaga, Spain; [email protected] * Correspondence: [email protected]; Tel.: +34-951953215 Received: 10 April 2020; Accepted: 12 May 2020; Published: 15 May 2020 Abstract: The amputation rate in patients with diabetes is 15 to 40 times higher than in patients without diabetes. To avoid major complications, the identification of high-risk in patients with diabetes through early assessment highlights as a crucial action. Clinician assessment tools are scales in which clinical examiners are specifically trained to make a correct judgment based on patient outcomes that helps to identify at-risk patients and monitor the intervention. The aim of this study is to carry out a systematic review of valid and reliable Clinician assessment tools for measuring diabetic foot disease-related variables and analysing their psychometric properties. The databases used were PubMed, Scopus, SciELO, CINAHL, Cochrane, PEDro, and EMBASE. The search terms used were foot, ankle, diabetes, diabetic foot, assessment, tools, instruments, score, scale, validity, and reliability. -
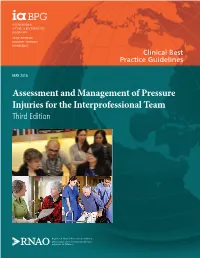
Assessment and Management of Pressure Injuries for the Interprofessional Team Third Edition Disclaimer
Clinical Best Practice Guidelines MAY 2016 Assessment and Management of Pressure Injuries for the Interprofessional Team Third Edition Disclaimer Th ese guidelines are not binding on nurses, other health care professionals, or the organizations that employ them. Th e use of these guidelines should be fl exible, and based on individual needs and local circumstances. Th ey neither constitute a liability nor discharge from liability. While every eff ort has been made to ensure the accuracy of the contents at the time of publication, neither the authors nor the Registered Nurses’ Association of Ontario (RNAO) gives any guarantee as to the accuracy of the information contained in them or accepts any liability with respect to loss, damage, injury, or expense arising from any such errors or omissions in the contents of this work. Copyright With the exception of those portions of this document for which a specifi c prohibition or limitation against copying appears, the balance of this document may be produced, reproduced, and published in its entirety, without modifi cation, in any form, including in electronic form, for educational or non-commercial purposes. Should any adaptation of the material be required for any reason, written permission must be obtained from RNAO. Appropriate credit or citation must appear on all copied materials as follows: Registered Nurses’ Association of Ontario (2016). Assessment and Management of Pressure Injuries for the Interprofessional Team, Th ird Edition. Toronto, ON: Registered Nurses’ Association of Ontario. Th is work is funded by the Ontario Ministry of Health and Long-Term Care. All work produced by RNAO is editorially independent from its funding source.