Pigmented Contact Dermatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

Frequency of Different Types of Facial Melanoses Referring to the Department of Dermatology and Venereology, Nepal Medical Colle
Amatya et al. BMC Dermatology (2020) 20:4 https://doi.org/10.1186/s12895-020-00100-3 RESEARCH ARTICLE Open Access Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life Bibush Amatya* , Anil Kumar Jha and Shristi Shrestha Abstract Background: Abnormalities of facial pigmentation, or facial melanoses, are a common presenting complaint in Nepal and are the result of a diverse range of conditions. Objectives: The objective of this study was to determine the frequency, underlying cause and impact on quality of life of facial pigmentary disorders among patients visiting the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital (NMCTH) over the course of one year. Methods: This was a cross-sectional study conducted at the Department of Dermatology and Venereology, NMCT H. We recruited patients with facial melanoses above 16 years of age who presented to the outpatient department. Clinical and demographic data were collected and all the enrolled participants completed the validated Nepali version of the Dermatology Life Quality Index (DLQI). Results: Between January 5, 2019 to January 4, 2020, a total of 485 patients were recruited in the study. The most common diagnoses were melasma (166 patients) and post acne hyperpigmentation (71 patients). Quality of life impairment was highest in patients having melasma with steroid induced rosacea-like dermatitis (DLQI = 13.54 ± 1.30), while it was lowest in participants with ephelides (2.45 ± 1.23). Conclusion: Facial melanoses are a common presenting complaint and lead to substantial impacts on quality of life. -

Melasma on the Nape of the Neck in a Man
Letters to the Editor 181 Melasma on the Nape of the Neck in a Man Ann A. Lonsdale-Eccles and J. A. A. Langtry Sunderland Royal Hospital, Kayll Road, Sunderland SR4 7TP, UK. E-mail: [email protected] Accepted July 19, 2004. Sir, sunlight and photosensitizing agents may be more We report a 47-year-old man with light brown macular relevant. pigmentation on the nape of his neck (Fig. 1). It was The differential diagnosis for pigmentation at this site asymptomatic and had developed gradually over 2 years. includes Riehl’s melanosis, Berloque dermatitis and He worked outdoors as a pipe fitter on an oilrig module; poikiloderma of Civatte. Riehl’s melanosis typically however, he denied exposure at this site because he involves the face with a brownish-grey pigmentation; always wore a shirt with a collar that covered the biopsy might be expected to show interface change and affected area. However, on further questioning it liquefaction basal cell degeneration with a moderate transpired that he spent most of the day with his head lymphohistiocytic infiltrate, melanophages and pigmen- bent forward. This reproducibly exposed the area of tary incontinence in the upper dermis. It is usually pigmentation with a sharp cut off inferiorly at the level associated with cosmetic use and may be considered of his collar. He used various shampoos, aftershaves and synonymous with pigmented allergic contact dermatitis shower gels, but none was applied directly to that area. of the face (6, 7). Berloque dermatitis is considered to be His skin was otherwise normal and there was no family caused by a photoirritant reaction to bergapentin; it history of abnormal pigmentation. -

An Unusual Presentation of a Unilateral Asymptomatic Riehl's
ts & C por a e se R S l Michael, Med Rep Case Stud 2018, 3:1 t a u c d i i DOI: 10.4172/2572-5130.1000152 d e s e M + Medical Reports and Case Studies ISSN: 2572-5130 Case Report Open Access An Unusual Presentation of a Unilateral Asymptomatic Riehl’s Melanosis in a 45 Year Old Male Chan Kam Tim Michael* Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong *Corresponding author: Chan Kam Tim Michael, Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong, Tel: +85221282129; E-mail: [email protected] Received Date: Feb 12, 2018; Accepted Date: Mar 12, 2018; Published Date: Mar 21, 2018 Copyright: © 2018 Michael CKT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction but of post-inflammatory hyperpigmentation, Acquired unilateral Nevus (Hori’s Nevus), Riehl’s melanosis, Drug-induced Pigmented contact dermatitis (PCD), also known as Riehl’s hyperpigmentation, Lichenoid dermatitis; as well as Melasma and melanosis, is a rare facial hyperpigmentation usually secondary to Ochronosis. cosmetics. There are few documented reports in the literature, and many cases without proven diagnosis may have been treated with pigment lasers, especially in beauty parlour settings. We report a case referred from a private practitioner who has a special interest in dermatology. The patient was diagnosed subsequently as having Riehl’s melanosis and treated with non-tyrosinase inhibitor bleaching agents, sun avoidance and mandatory abstinence from over-the-counter cosmetic products. -

Poikiloderma of Civatte, Slapped Neck Solar Melanosis, Basal Melanin Stores
American Journal of Dermatology and Venereology 2019, 8(1): 8-13 DOI: 10.5923/j.ajdv.20190801.03 Slapped Neck Solar Melanosis: Is It a New Entity or a Variant of Poikiloderma of Civatte?? (Clinical and Histopathological Study) Khalifa E. Sharquie1,*, Adil A. Noaimi2, Ansam B. Kaftan3 1Department of Dermatology, College of Medicine, University of Baghdad 2Iraqi and Arab Board for Dermatology and Venereology, Dermatology Center, Medical City, Baghdad, Iraq 3Dermatology Center, Medical City, Baghdad, Iraq Abstract Background: Poikiloderma of Civatte although is a common complaint among population, especially European, still it was not reported in dark skin people as in Iraqi population. Objectives: To study all the clinical and histopathological features of Poikiloderma of Civatte in Iraqi population. Patients and Methods: This study is descriptive, clinical and histopathological study. It was carried out at the Dermatology Center, Medical City, Baghdad, Iraq, from September 2017 to October 2018. Thirty-one patients with Poikiloderma of Civatte were included and evaluated by history, physical examination, Wood’s light examination. Lesional skin biopsies were obtained from 9 patients, with histological examination of the sections stained with Hematoxylin and Eosin (H&E) and Fontana-Masson stain. Results: Thirty-one patients were included in this study, with mean age +/- SD was 53.32+/-10 years, and all patients were males. Twenty-six patients (84%) were with skin phenotype III&IV, The pigmentation was either mainly erythematous (22.5%), mainly dark brown pigmentation (29%), and mixed type of pigmentation (48.5%). These lesions were distributed on the sides of the neck and the face and the V shaped area of the chest. -
Hyperpigmentation on the Head and Neck
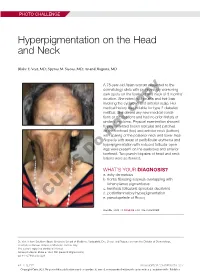
PHOTO CHALLENGE Hyperpigmentation on the Head and Neck Blake E. Vest, MD; Spyros M. Siscos, MD; Anand Rajpara, MD A 78-year-old Asian woman presented to the dermatology clinic with progressively worsening dark spots on the forehead and neck of 3 months’ duration. She noted mild pruritis and hair loss involving the eyebrows and anterior scalp. Her medical history was notable for type 2 diabetes mellitus. She deniedcopy any new medical condi- tions or medications and had no prior history of similar symptoms. Physical examination showed hyperpigmented brown macules and patches on the forehead (top) and anterior neck (bottom) withnot sparing of the posterior neck and lower face. Alopecia with areas of perifollicular erythema and hyperpigmentation with reduced follicular open- ings were present on the eyebrows and anterior Doforehead. Two punch biopsies of head and neck lesions were performed. WHAT’S YOUR DIAGNOSIS? a. ashy dermatosis b. frontal fibrosing alopecia overlapping with lichen planus pigmentosus c. keratosis follicularis spinulosa decalvans d. postinflammatory hyperpigmentation CUTIS e. pseudopelade of Brocq PLEASE TURN TO PAGE E3 FOR THE DIAGNOSIS Dr. Vest is from Southern Illinois University School of Medicine, Springfield. Drs. Siscos and Rajpara are from the Division of Dermatology, University of Kansas School of Medicine, Kansas City. The authors report no conflict of interest. Correspondence: Blake E. Vest, MD ([email protected]). doi:10.12788/cutis.0226 E2 I CUTIS® WWW.MDEDGE.COM/DERMATOLOGY Copyright Cutis 2021. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Frontal Fibrosing Alopecia Overlapping With Lichen Planus Pigmentosus icroscopic examination revealed focal dermal of the skin have been reported, including the entire pigmentation, papillary fibrosis, and epidermal scalp, eyebrows, and eyelashes. -

Pigmented Contact Dermatitis and Chemical Depigmentation
18_319_334* 05.11.2005 10:30 Uhr Seite 319 Chapter 18 Pigmented Contact Dermatitis 18 and Chemical Depigmentation Hideo Nakayama Contents ca, often occurs without showing any positive mani- 18.1 Hyperpigmentation Associated festations of dermatitis such as marked erythema, with Contact Dermatitis . 319 vesiculation, swelling, papules, rough skin or scaling. 18.1.1 Classification . 319 Therefore, patients may complain only of a pigmen- 18.1.2 Pigmented Contact Dermatitis . 320 tary disorder, even though the disease is entirely the 18.1.2.1 History and Causative Agents . 320 result of allergic contact dermatitis. Hyperpigmenta- 18.1.2.2 Differential Diagnosis . 323 tion caused by incontinentia pigmenti histologica 18.1.2.3 Prevention and Treatment . 323 has often been called a lichenoid reaction, since the 18.1.3 Pigmented Cosmetic Dermatitis . 324 presence of basal liquefaction degeneration, the ac- 18.1.3.1 Signs . 324 cumulation of melanin pigment, and the mononucle- 18.1.3.2 Causative Allergens . 325 ar cell infiltrate in the upper dermis are very similar 18.1.3.3 Treatment . 326 to the histopathological manifestations of lichen pla- 18.1.4 Purpuric Dermatitis . 328 nus. However, compared with typical lichen planus, 18.1.5 “Dirty Neck” of Atopic Eczema . 329 hyperkeratosis is usually milder, hypergranulosis 18.2 Depigmentation from Contact and saw-tooth-shape acanthosis are lacking, hyaline with Chemicals . 330 bodies are hardly seen, and the band-like massive in- 18.2.1 Mechanism of Leukoderma filtration with lymphocytes and histiocytes is lack- due to Chemicals . 330 ing. 18.2.2 Contact Leukoderma Caused Mainly by Contact Sensitization . -

SKIN HYPERPIGMENTATION DISORDERS and USE of HERBAL EXTRACTS: a REVIEW Priyam Goswami* and H
Current Trends in Pharmaceutical Research 2020 Vol 7 Issue 2 © Dibrugarh University www.dibru.ac.in/ctpr ISSN: 2319-4820 (Print) 2582-4783 (Online) Mini Review SKIN HYPERPIGMENTATION DISORDERS AND USE OF HERBAL EXTRACTS: A REVIEW Priyam Goswami* and H. K. Sharma Department of Pharmaceutical Sciences, Faculty of Science and Engineering, Dibrugarh University Abstract Background: Problems pertaining to the skin pigmentation is one of the major concerns that affect the quality of life of human beings especially women. The disturbances in the melanin production mainly results in skin pigmentation disorders. For centuries natural ingredients have been used in the treatment of skin hyperpigmentation disorders. Since synthetic cosmetic ingredients can have potential side effects, emphasis has been given on the herbal products, which are considered to be mild and biodegradable, exhibiting low toxicity. Objective: The objective of this review is to provide a brief understanding about the skin hyperpigmentation disorders and the use of various herbal extracts as a notable approach for its treatment. Methods: A narrative literature review was conducted with the extraction of information, which was analyzed from various databases viz. Google scholar, Science Direct, PubMed, Wiley Online Library etc., Results and Discussions: The preferences of the people for the use of herbal skin- lightening agents over the synthetic ones have gained wide spread popularity. Potentially active compounds that have been extracted from the plants have been identified which provide scope for its use a novel depigmenting agent. The improvement in the efficacy of the herbal extracts is mainly due to synergism, and hence this property yields great results when used in cosmetic formulations. -

Overview of Skin Whitening Agents: Drugs and Cosmetic Products
cosmetics Review Overview of Skin Whitening Agents: Drugs and Cosmetic Products Céline Couteau and Laurence Coiffard * Faculty of Pharmacy, Université de Nantes, Nantes Atlantique Universités, LPiC, MMS, EA2160, 9 rue Bias, Nantes F-44000, France; [email protected] * Correspondence: [email protected]; Tel.: +33-253484317 Academic Editor: Enzo Berardesca Received: 30 March 2016; Accepted: 13 July 2016; Published: 25 July 2016 Abstract: Depigmentation and skin lightening products, which have been in use for ages in Asian countries where skin whiteness is a major esthetic criterion, are now also highly valued by Western populations, who expose themselves excessively to the sun and develop skin spots as a consequence. After discussing the various possible mechanisms of depigmentation, the different molecules that can be used as well as the status of the products containing them will now be presented. Hydroquinone and derivatives thereof, retinoids, alpha- and beta-hydroxy acids, ascorbic acid, divalent ion chelators, kojic acid, azelaic acid, as well as diverse herbal extracts are described in terms of their efficacy and safety. Since a genuine effect (without toxic effects) is difficult to obtain, prevention by using sunscreen products is always preferable. Keywords: depigmenting agents; safety; efficacy 1. Introduction The allure of a pale complexion is nothing new and many doctors have been looking into this subject for some time, proposing diverse and varied recipes for eliminating all unsightly marks (freckles and liver spots were clearly targeted). Pliny the Elder (Naturalis Historia), Dioscoride (De Universa medicina), Castore Durante (Herbario nuove), and other authors from other time periods have addressed this issue. -

Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia
CASE REPORT Print ISSN 1738-6586 / On-line ISSN 2005-5013 J Clin Neurol 2014 Open Access Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia Fabrice C. Deprez,a Julie Coulier,b Denis Rommel,a Antonella Boschib aDepartments of Radiology and bOphthalmology, Cliniques Universitaires Saint-Luc, UCL, Brussels, Belgium BackgroundzzHorner syndrome (HS), also known as Claude-Bernard-Horner syndrome or Received August 5, 2013 oculosympathetic palsy, comprises ipsilateral ptosis, miosis, and facial anhidrosis. Revised April 15, 2014 Accepted April 21, 2014 Case ReportzzWe report herein the case of a 67-year-old man who presented with congenital HS associated with ipsilateral hypoplasia of the internal carotid artery (ICA), as revealed by Correspondence heterochromia iridis and confirmed by computed tomography (CT). Fabrice C. Deprez, MD Department of Radiology, ConclusionszzCT evaluation of the skull base is essential to establish this diagnosis and dis- Cliniques Universitaires Saint-Luc, tinguish aplasia from agenesis/hypoplasia (by the absence or hypoplasia of the carotid canal) or UCL, Avenue Hippocrate 10, from acquired ICA obstruction as demonstrated by angiographic CT. 1200 Woluwe-Saint-Lambert, J Clin Neurol 2014 Belgium Tel +32.472.93.34.80 Key Wordszzcongenital horner syndrome, internal carotid artery agenesis, Fax +32.81.42.35.05 heterochromia iridis, computed tomography. E-mail [email protected] Introduction spindly left ICA, which was misinterpreted as ICA thrombosis (Fig. 1). The left anterior cerebral artery and MCA were sup- Horner syndrome (HS), also known as Claude-Bernard-Horn- plied by a large posterior communicating artery from the bas- er syndrome or oculosympathetic palsy, comprises ipsilateral ilar artery. -

Table I. Genodermatoses with Known Gene Defects 92 Pulkkinen
92 Pulkkinen, Ringpfeil, and Uitto JAM ACAD DERMATOL JULY 2002 Table I. Genodermatoses with known gene defects Reference Disease Mutated gene* Affected protein/function No.† Epidermal fragility disorders DEB COL7A1 Type VII collagen 6 Junctional EB LAMA3, LAMB3, ␣3, 3, and ␥2 chains of laminin 5, 6 LAMC2, COL17A1 type XVII collagen EB with pyloric atresia ITGA6, ITGB4 ␣64 Integrin 6 EB with muscular dystrophy PLEC1 Plectin 6 EB simplex KRT5, KRT14 Keratins 5 and 14 46 Ectodermal dysplasia with skin fragility PKP1 Plakophilin 1 47 Hailey-Hailey disease ATP2C1 ATP-dependent calcium transporter 13 Keratinization disorders Epidermolytic hyperkeratosis KRT1, KRT10 Keratins 1 and 10 46 Ichthyosis hystrix KRT1 Keratin 1 48 Epidermolytic PPK KRT9 Keratin 9 46 Nonepidermolytic PPK KRT1, KRT16 Keratins 1 and 16 46 Ichthyosis bullosa of Siemens KRT2e Keratin 2e 46 Pachyonychia congenita, types 1 and 2 KRT6a, KRT6b, KRT16, Keratins 6a, 6b, 16, and 17 46 KRT17 White sponge naevus KRT4, KRT13 Keratins 4 and 13 46 X-linked recessive ichthyosis STS Steroid sulfatase 49 Lamellar ichthyosis TGM1 Transglutaminase 1 50 Mutilating keratoderma with ichthyosis LOR Loricrin 10 Vohwinkel’s syndrome GJB2 Connexin 26 12 PPK with deafness GJB2 Connexin 26 12 Erythrokeratodermia variabilis GJB3, GJB4 Connexins 31 and 30.3 12 Darier disease ATP2A2 ATP-dependent calcium 14 transporter Striate PPK DSP, DSG1 Desmoplakin, desmoglein 1 51, 52 Conradi-Hu¨nermann-Happle syndrome EBP Delta 8-delta 7 sterol isomerase 53 (emopamil binding protein) Mal de Meleda ARS SLURP-1 -

A Clinicoepidemiological Study of Facial Hypermelanosis Among Females of Reproductive Age Group
Our Dermatology Online Original Article A cclinicoepidemiologicallinicoepidemiological sstudytudy ooff ffacialacial hhypermelanosisypermelanosis aamongmong ffemalesemales ooff rreproductiveeproductive aagege ggrouproup Sameer Abrol1, Rohini Sharma2 1M.D. Medicine. GMC Jammu, Jammu and Kashmir, India, 2Assistant professor, Department of Dermatology, GMC Rajouri, Jammu and Kashmir, India Corresponding author: Dr. Rohini Sharma, E-mail: [email protected] ABSTRACT Background: Facial hypermelanosis has great psychological and aesthetic complications attached to it specially in females. A number of factors like genetic, environmental, systemic, work in consortium to give rise to various types of hypermelanosis. Women in the 15-49 years age group, which is the reproductive age group are influenced by various hormonal alterations along with external and systemic agents thus manifesting as various types of hypermelanosis. Aims and objectives: This study was undertaken to assess the clinical and epidemiological aspects of various types of facial hypermelanosis and various factors implicated. Material and methods: A total of 350 women in the age group of 15- 49 years were taken up for the study. A detailed clinical history, thorough examination was done in all patients. Relevant investigations were carried out. All the results were statistically analyzed and inferences were drawn. Results: A total of 350 women were taken up for study. Maximum patients (133,38%) were in the age group of 26 -35 years. Among various hypermelanosis, maximum women(128,36.5%) came with the complaint of melasma, 90(25.7%) women with post inflammatory hypermelanosis, 50(14.3%)females with periorbital hypermelanosis. In our study, melasma, post inflammatory hyperpigmentation due to acne, acanthosis nigricans formed a major share in the 15-49 years age group thus suggesting the role of hormonal alterations and rising PCOS.