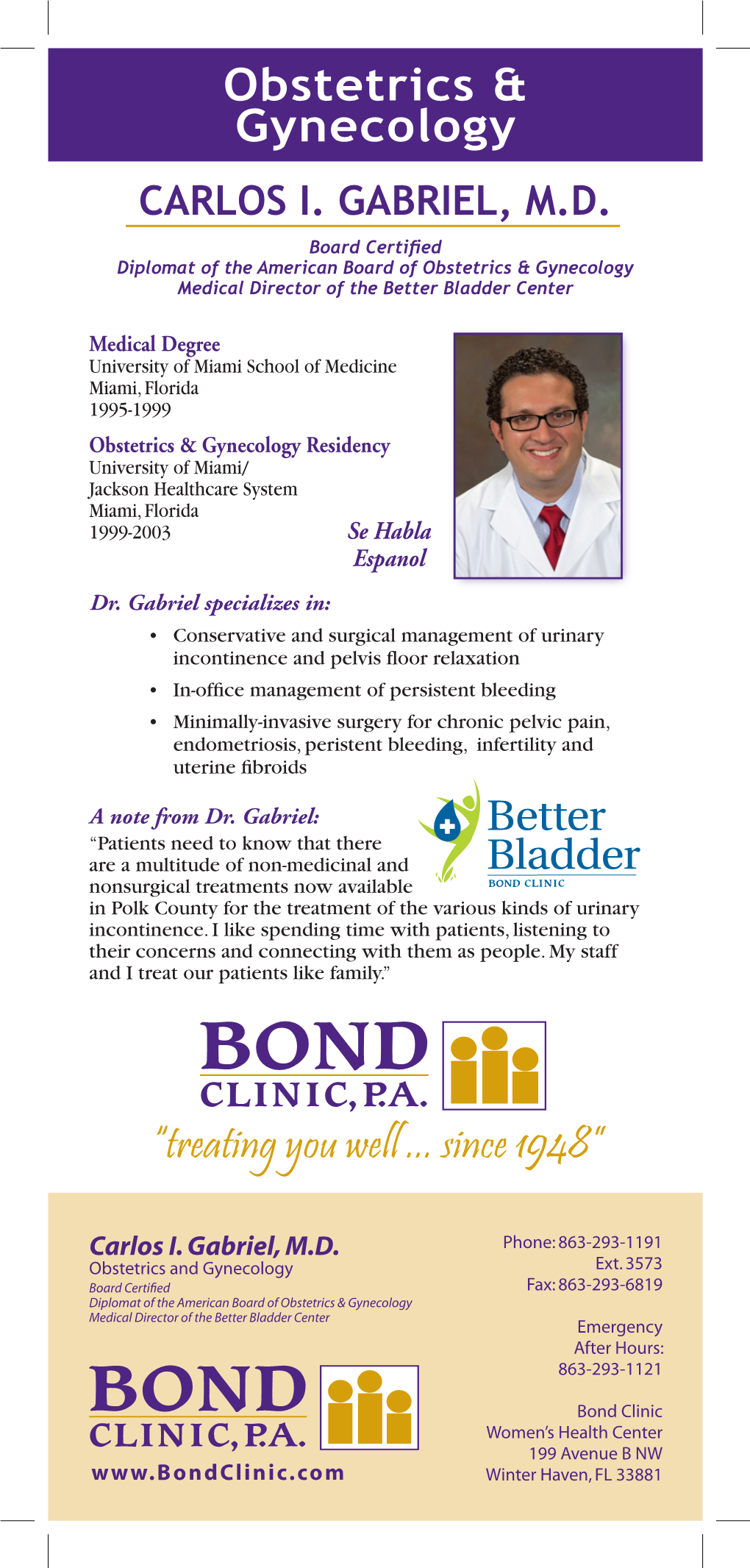
Obstetrics & Gynecology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hysteroscopy and Endometrial Ablation Using Novasure
Hysteroscopy and Endometrial Ablation Using Novasure What is a hysteroscopy and endometrial ablation using Novasure? This is a procedure where a doctor uses a thin tube with a tiny camera to look inside the uterus. There are no incisions. Saline solution is used to expand the uterus in order to look at the inside of the uterus. The Novasure device is then used to burn the lining of the uterus. When is this surgery used? To evaluate and or treat diseases of the uterus • Painful periods. • Heavy or irregular vaginal bleeding. How do I prepare for surgery? • Before surgery, a pre-op appointment will be scheduled with your doctor at their office or with a nurse practitioner or physician assistant at Domino Farms. • Depending on your health, we may ask you to see your primary doctor, a specialist, and/or an anesthesiologist to make sure you are healthy for surgery. • The lab work for your surgery must be done at least 3 days before surgery. • Some medications need to be stopped before the surgery. A list of medications will be provided at your pre-operative appointment. • Smoking can affect your surgery and recovery. Smokers may have difficulty breathing during the surgery and tend to heal more slowly after surgery. If you are a smoker, it is best to quit 6-8 weeks before surgery. If you are unable to stop smoking before surgery, your doctor can order a nicotine patch while you are in the hospital. Department of Obstetrics and Gynecology (734) 763-6295 - 1 - • You will be told at your pre-op visit whether you will need a bowel prep for your surgery and if you do, what type you will use. -

Sterilization and Abortion Policy Billing Instructions
Sterilization and Abortion Policy Billing Instructions Table of contents Table of contents ...................................................................................................................................... 1 Hysterectomy ............................................................................................................................................ 2 Acknowledgement forms ..................................................................................................................... 2 Prior authorization requirements ......................................................................................................... 2 Covered services ................................................................................................................................... 2 Intrauterine Devices and Subdermal Implants ......................................................................................... 4 Family planning: sterilization .................................................................................................................... 4 Prior authorization requirements ......................................................................................................... 5 Covered services ................................................................................................................................... 5 Abortion .................................................................................................................................................... 6 Claim -
OBGYN Student Guide 2014.Pdf
TABLE OF CONTENTS COMMON ABBREVIATIONS • 3 COMMON PRESCRIPTIONS • 4 OBSTETRICS • 5 What is a normal morning like on OB? • 5 What are good questions to ask a post-op/post-partum patient in the morning? • 6 How do I manage a post-partum patient? • 7 How should I organize and write my post-partum note? • 8 How do I present a patient on rounds? • 9 How do I evaluate a patient in triage/L&D? • 9 What are the most common complaints presented at triage/L&D? • 10 How should I organize and write my note for a triage H&P? • 12 What are the most common reasons people are admitted? • 13 How do I deliver a baby? • 13 What is my role as a student in a Cesarean section or tubal ligation procedure? • 15 How do I write up post-op orders? • 15 GYNECOLOGY/GYNECOLOGY ONCOLOGY • 17 What should I do to prepare for a GYN surgery? • 17 How do I manage a Gynecology/Gynecology Oncology patient? • 17 How should I organize and write my post-op GYN note? • 18 How do I write admit orders? • 19 What do routine post-op orders (Day #1) look like? • 19 What are the most common causes of post-operative fever? • 20 CLINIC • 21 What is my role as a student in clinic? • 21 What should I include in my prenatal clinic note? • 21 What should I include in my GYN clinic note? • 22 COMMON PIMP QUESTIONS • 23 2 COMMON ABBREVIATIONS 1°LTCS- primary low transverse cesarean LOF- leakage of fluid section NST- nonstress test AFI- amniotic fluid index NSVD- normal spontaneous vaginal delivery AROM- artificial rupture of membranes NT/NE- non-tender/non-engorged (breast BPP- biophysical -

Endometrial Ablation
PATIENT INFORMATION A publication of Jackson-Madison County General Hospital Surgical Services Endometrial Ablation As an alternative to hysterectomy, your doctor may recommend a procedure called an endometrial ablation. The endometrium is the lining of the uterus. The word ablation means destroy. This surgery eliminates the endometrial lining of the uterus. It is often used in cases of very heavy menstrual bleeding. Because this surgery causes a decrease in the chances of becoming pregnant, it is not recommended for women who still want to have children. The advantage of this procedure is that your recovery time is usually faster than with hysterectomy. Your doctor will use general anesthesia or spinal anesthesia to perform the procedure. He will talk with you about the type of anesthesia that will be used in your case. This surgery can be done in an outpatient setting. During the procedure, a narrow, lighted viewing tube (the size of a pencil) called a hysteroscope is inserted through the vagina and cervix into the uterus. A tiny camera that is attached shows the uterus on a monitor. There are several ways the endometrial lining can be ablated (destroyed). Those methods include laser, radio waves, electrical current, freezing, hot water (balloon), or heated loop. The instruments are inserted through the tube to perform the ablation. Your doctor may also do a laparoscopy at the same time to be sure there are not other conditions that might require treatment or further surgery. In a laparoscopy, a small, lighted scope is used to look at the other organs in the pelvis. -

Endometrial Ablation
AQ The American College of Obstetricians and Gynecologists FREQUENTLY ASKED QUESTIONS FAQ134 fSPECIAL PROCEDURES Endometrial Ablation • What is endometrial ablation? • Why is endometrial ablation done? • Who should not have endometrial ablation? • Can I still get pregnant after having endometrial ablation? • What techniques are used to perform endometrial ablation? • What should I expect after the procedure? • What are the risks associated with endometrial ablation? • Glossary What is endometrial ablation? Endometrial ablation destroys a thin layer of the lining of the uterus and stops the menstrual flow in many women. In some women, menstrual bleeding does not stop but is reduced to normal or lighter levels. If ablation does not control heavy bleeding, further treatment or surgery may be required. Why is endometrial ablation done? Endometrial ablation is used to treat many causes of heavy bleeding. In most cases, women with heavy bleeding are treated first with medication. If heavy bleeding cannot be controlled with medication, endometrial ablation may be used. Who should not have endometrial ablation? Endometrial ablation should not be done in women past menopause. It is not recommended for women with certain medical conditions, including the following: • Disorders of the uterus or endometrium • Endometrial hyperplasia • Cancer of the uterus • Recent pregnancy • Current or recent infection of the uterus Can I still get pregnant after having endometrial ablation? Pregnancy is not likely after ablation, but it can happen. If it does, the risk of miscarriage and other problems are greatly increased. If a woman still wants to become pregnant, she should not have this procedure. Women who have endometrial ablation should use birth control until after menopause. -

Ultrasound-Guided Reoperative Hysteroscopy: Managing Endometrial Ablation Failures
#424 Wortman FINAL Gynecology SURGICAL TECHNOLOGY INTERNATIONAL XXII Ultrasound-guided Reoperative Hysteroscopy: Managing Endometrial Ablation Failures MORRIS WORTMAN, MD, FACOG CLINICAL ASSOCIATE PROFESSOR OF GYNECOLOGY UNIVERSITY OF ROCHESTER MEDICAL CENTER DIRECTOR, CENTER FOR MENSTRUAL DISORDERS AND REPRODUCTIVE CHOICE ROCHESTER, NEW YORK ABSTRACT ndometrial ablation and hysteroscopic myomectomy and polypectomy are having an increasing impact on the care of women with abnormal uterine bleeding (AUB). The complications of these procedures Einclude the late onset of recurrent vaginal bleeding, cyclic lower abdominal pain, hematometra and the inability to adequately sample the endometrium in women with postmenopausal bleeding. According to the 2007 ACOG Practice Bulletin, approximately 24% of women treated with endometrial ablation will undergo hysterectomy within 4 years.1 By employing careful cervical dilation, a wide variety of gynecologic resectoscopes, and continuous sonographic guidance it is possible to explore the entire uterine cavity in order to locate areas of sequestered endometrium, adenomyosis, and occult hematometra. Sonographically guided reoperative hysteroscopy offers a minimally invasive technique to avoid hysterectomy in over 60% to 88% of women who experience endometrial ablation failures.2,3 The procedure is adaptable to an office-based setting and offers a very low incidence of operative complications and morbidity. In addition, the technique provides a histologic specimen, which is essential in adequately evaluating the endometrium in postmenopausal women or women at high risk for the development of adenocarcinoma of the endometrium. - 1 - #424 Wortman FINAL Ultrasound-guided Reoperative Hysteroscopy: Managing Endometrial Ablation Failures WORTMAN INTRODUCTION It is well known that of women who Troublesome vaginal bleeding, may undergo EA a significant number will occur months or years following EA and eventually require a hysterectomy. -

Laparoscopic Tubal Ligation
Laparoscopic Tubal Ligation – Permanent Birth Control UR Medicine Ob/Gyn How does a tubal ligation work? A fallopian tube is attached to each side of your uterus (womb). Tubal ligation is surgery to close your fallopian tubes. It is also called female sterilization or having your "tubes tied". Your surgeon uses a laparoscope to do the surgery. This scope is a long metal tube with a magnifying camera and a light on the end. It is put into your abdomen through one or more small incisions (cuts). How is a tubal ligation performed? During a tubal ligation, your fallopian tubes are burned shut, cut, or closed with a type of clip. Immediately after your tubes are closed, sperm will not be able to reach an egg and cause pregnancy. A tubal ligation is an effective and permanent (lifelong) form of birth control. Before having this surgery, you must be sure that you never want to become pregnant in the future. You will still have monthly periods after your tubal ligation. A tubal ligation will not protect you from sexually transmitted diseases. Are there any side effects or risks? There are always risks with surgery. During any surgery, you may bleed more than usual, have trouble breathing, or get an infection. Blood vessels or organs such as your bowel or bladder could be injured during surgery. Although pregnancy is unlikely after a tubal ligation, there is a small chance of it. If pregnancy does occur, there is an increased risk of having an ectopic pregnancy (pregnancy in the tubes). A tubal ligation can be reversed but it does not mean you will be able to get pregnant again. -

Tubal Ligation (Laparoscopic Sterilization)
AQ The American College of Obstetricians and Gynecologists FREQUENTLY ASKED QUESTIONS FAQ035 CONTRACEPTION Sterilization by Laparoscopy • What is sterilization? • What is laparoscopy? f • Does sterilization protect against sexually transmitted diseases (STDs)? • What should I consider before having sterilization? • Can all women have laparoscopic sterilization? • How is laparoscopic sterilization done? • What are the benefits of laparoscopic sterilization? • What are the risks of laparoscopic sterilization? • What should I expect after surgery? • Glossary What is sterilization? Sterilization is surgery performed to prevent a woman from getting pregnant. It is meant to be permanent. With tubal sterilization, both fallopian tubes are blocked by tying, sealing, or attaching a ring or clip to them. The egg then cannot move down the tube to the uterus and the sperm cannot reach the egg. This prevents pregnancy. Sterilization often is done with a technique called laparoscopy. What is laparoscopy? Laparoscopy is a way of doing surgery. In laparoscopy, a device like a small telescope called a laparoscope is inserted into the pelvic cavity through a small incision. Laparoscopy can be done as an outpatient procedure. This means you usually can go home the same day. Does sterilization protect against sexually transmitted diseases (STDs)? Sterilization does not protect against sexually transmitted diseases (STDs) (see the FAQ How to Prevent Sexually Transmitted Diseases). If you are at risk of getting an STD, you still need to protect yourself by using condoms. What should I consider before having sterilization? Sterilization is a permanent method of birth control. You and your partner must be certain that you do not want any more children—now or in the future. -

How Gynecologic Procedures and Pharmacologic Treatments Can Affect the Uterus
IMAGES IN GYN ULTRASOUND How gynecologic procedures and pharmacologic treatments can affect the uterus Understanding and identifying possible uterine changes caused by endometrial ablation and tamoxifen use can be important for subsequent treatment decisions. In addition, Asherman syndrome and cesarean scar defect clearly alter the uterus, but what are their signs on imaging? Michelle Stalnaker Ozcan, MD, and Andrew M. Kaunitz, MD ew technology, minimally invasive defect, and altered endometrium as a result surgical procedures, and medica‑ of tamoxifen use. In this article, we provide Ntions continue to change how physi‑ 2 dimensional and 3 dimensional sono‑ cians manage specific medical issues. Many graphic images of uterine presentations of IN THIS ARTICLE procedures and medications used by gyne‑ these 4 conditions. Additional case images can cologists can cause characteristic findings be found with the online version of this article on sonography. These findings can guide at obgmanagement.com. Foreword subsequent counseling and management by Steven R. decisions and are important to accurately Goldstein, MD interpret on imaging. Among these condi‑ Asherman syndrome page 19 tions are Asherman syndrome, postendome‑ Characterized by variable scarring, or intra‑ trial ablation uterine damage, cesarean scar uterine adhesions, inside the uterine cavity Uterine changes following endometrial trauma due to surgical postablation procedures, Asherman syndrome can cause Dr. Ozcan is Assistant Professor and menstrual changes and infertility. Should page 20 Co-Program Director, Obstetrics and Gynecology Residency, Department pregnancy occur in the setting of Asherman of Obstetrics and Gynecology, at syndrome, placental abnormalities may re‑ Endometrial the University of Central Florida 1 College of Medicine−Orlando. -

Endometrial Ablation
Endometrial Ablation Endometrial ablation is a surgical procedure that removes Each month a thickening of cells occurs to produce the superficial the inside layer (the endometrium) or lining of the uterus. The part. In a usual menstrual cycle, where pregnancy does not endometrium is the part that sheds each month as a period occur and without any hormone treatments (such as the oral (menstruation ).The endometrium consists of 2 parts: contraceptive pill), the superficial part is shed and menstruation 1. A deep part (called the basalis) occurs. The deep part is always present and does not shed to allow 2. A superficial part (called the superficialis) the process to be repeated in the following month. guarantee no bleeding following the procedure. Following an endometrial ablation there are four possible outcomes: 1. No periods at all (called amenorrhea) (40% of cases) 2. Very light periods/spotting (40% of cases) 3. Reduced bleeding to what is acceptable (10% of cases) 4. No change in menstrual bleeding (10% of cases) What happens in an endometrial ablation? Endometrial ablation can be performed using different methods. Scientific studies have not shown that one method is better than others, either in terms of outcomes or complications. The method recommended by your doctor will depend on your presenting symptoms, past history (such as a history of classical caesarean delivery) and other medical considerations (such as bleeding disorders). Other factors will include the type of ablation your Sometimes, there may be excessive bleeding (causing clots, doctor is familiar with and availability of specialised equipment. flooding and pain) at the time of menstruation. -
Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Laparoscopic Bilateral Tubal Ligation
501 19th Street, Trustee Towers FORT SANDERS WOMEN’S SPECIALISTS 1924 Pinnacle Point Way Suite 401, Knoxville Tn 37916 P# 865-541-1122 F# 865-541-1976 Suite 200, Knoxville Tn 37922 Dr. Curtis Elam, M.D., FACOG, AIMIS, Dr. David Owen, M.D., FACOG, Dr. Brooke Foulk, M.D., FACOG Dr. Dean Turner M.D., FACOG, ASCCP, Dr. F. Robert McKeown III, M.D., FACOG, AIMIS Dr. Steven Pierce M.D., Dr. G. Walton Smith, M.D., FACOG, Dr. Susan Robertson, M.D., FACOG LAPAROSCOPIC BILATERAL TUBAL LIGATION Please read and sign the following consent form when you feel that you completely understand the surgical procedure that is to be performed and after you have asked all of your questions. If you have any further questions or concerns, please contact our office prior to your procedure so that we may clarify any pertinent issues. Definition: Laparoscopic Bilateral Tubal Ligation (BTL) is a minimally invasive surgical procedure that enables the physician to permanently sterilize the patient through several small abdominal incisions instead of one large abdominal incision. The surgeon places a laparoscope (thin lighted telescope/camera) and surgical instruments inserted through small incisions to block the fallopian tubes. Procedure: After sedation from general anesthesia is achieved, the surgeon will make a small incision at or near your belly button for the laparoscope to be passed through and 1-2 additional incisions in your lower abdomen to insert necessary surgical instruments. Carbon dioxide gas will be used to inflate the abdomen to allow the doctor to insert the laparoscope and visualize the abdomen/pelvis.