UP CRM Final Draft Report 03.12.12
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
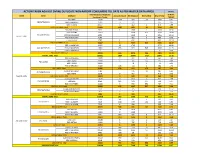
Action Taken Against Dvvnl Duplicate Non-Rapdrp Consumers Till Date As Per Master Data Apr20 in Nos
ACTION TAKEN AGAINST DVVNL DUPLICATE NON-RAPDRP CONSUMERS TILL DATE AS PER MASTER DATA APR20 IN NOS. Total Suspected Duplicate % W.R.T. ZONE Circle DivName Account Closed Bill Stopped Dismantled Grand Total Consumers Target TARGET EDD-BAH 17047 1116 289 28 1433 8.41 EDCFATEHABAD EDD-ETMADPUR 10405 75 232 307 2.95 EDD-III AGRA 23657 6 462 2 470 1.99 EDCFATEHABAD Total 51109 1197 983 30 2210 4.32 EDD-FIROZABAD 9032 1 1566 1 1568 17.36 EDD-JASRANA 14167 3408 826 4234 29.89 EDC-FIROZABAD EDD-SHIKOHABAD 6292 1449 6 1455 23.12 AGRA 1 ZONE EDD-SHIRSAGANJ 7149 482 3 485 6.78 S EDD-TUNDLA 4787 1 632 1 634 13.24 EDC-FIROZABAD Total 41427 2 7537 837 8376 20.22 EDD-II MAINPURI 16327 32 1745 1777 10.88 EDC-MAINPURI EDD-III MAINPURI 13681 433 629 546 1608 11.75 EUDD-1 MAINPURI 7 0 0.00 EDC-MAINPURI Total 30015 465 2374 546 3385 11.28 AGRA 1 ZONE Total 122551 1664 10894 1413 13971 11.40 EDD KHERAGARH 12877 7 322 32 361 2.80 EDD-I AGRA 27184 5 105 133 243 0.89 EDC-IAGRA EDD-II AGRA 24091 78 1 79 0.33 EDD-IV KIRAWALI 15183 146 114 4 264 1.74 EDC-IAGRA Total 79335 158 619 170 947 1.19 EDD-III MATHURA 7781 476 11 487 6.26 EDC-IIMATHURA EDD-MATH 5270 9 467 476 9.03 AGRA 2 ZONE EDC-IIMATHURA Total 13051 9 943 11 963 7.38 EDD GOVERDHAN 13014 7 613 2 622 4.78 EDCMATHURA EDD KOSI 8099 185 171 144 500 6.17 EDD-I MATHURA 10226 3 333 391 727 7.11 EDCMATHURA Total 31339 195 1117 537 1849 5.90 EUDD-II VRINDAVAN 1432 3 225 228 15.92 EUDCMATHURA EUDD-III MATHURA 453 2 4 6 1.32 EUDCMATHURA Total 1885 5 229 234 12.41 AGRA 2 ZONE Total 125610 367 2908 718 3993 3.18 EDD-I -

Drishti IAS Coaching in Delhi, Online IAS Test Series & Study Material
Drishti IAS Coaching in Delhi, Online IAS Test Series & Study Material drishtiias.com/printpdf/uttar-pradesh-gk-state-pcs-english Uttar Pradesh GK UTTAR PRADESH GK State Uttar Pradesh Capital Lucknow Formation 1 November, 1956 Area 2,40,928 sq. kms. District 75 Administrative Division 18 Population 19,98,12,341 1/20 State Symbol State State Emblem: Bird: A pall Sarus wavy, in Crane chief a (Grus bow–and– Antigone) arrow and in base two fishes 2/20 State State Animal: Tree: Barasingha Ashoka (Rucervus Duvaucelii) State State Flower: Sport: Palash Hockey Uttar Pradesh : General Introduction Reorganisation of State – 1 November, 1956 Name of State – North-West Province (From 1836) – North-West Agra and Oudh Province (From 1877) – United Provinces Agra and Oudh (From 1902) – United Provinces (From 1937) – Uttar Pradesh (From 24 January, 1950) State Capital – Agra (From 1836) – Prayagraj (From 1858) – Lucknow (partial) (From 1921) – Lucknow (completely) (From 1935) Partition of State – 9 November, 2000 [Uttaranchal (currently Uttarakhand) was formed by craving out 13 districts of Uttar Pradesh. Districts of Uttar Pradesh in the National Capital Region (NCR) – 8 (Meerut, Ghaziabad, Gautam Budh Nagar, Bulandshahr, Hapur, Baghpat, Muzaffarnagar, Shamli) Such Chief Ministers of Uttar Pradesh, who got the distinction of being the Prime Minister of India – Chaudhary Charan Singh and Vishwanath Pratap Singh Such Speaker of Uttar Pradesh Legislative Assembly, who also became Chief Minister – Shri Banarsidas and Shripati Mishra Speaker of the 17th Legislative -

ORIGINAL ARTICLE Pissn 0976 3325│Eissn 2229 6816 Open Access Article
ORIGINAL ARTICLE pISSN 0976 3325│eISSN 2229 6816 Open Access Article www.njcmindia.org ASSESSMENT OF MAGNITUDE AND THE CO-MORBIDITIES OF OVERWEIGHT AND OBESITY IN URBAN AND RURAL AREAS OF KANPUR Naresh Pal Singh1, Pankaj K Jain2, R P Sharma3, Suresh Chandra4, Seema Nigam4, Anamika Singh5 Financial Support: None declared Conflict of interest: None declared ABSTRACT Copy right: The Journal retains the copyrights of this article. However, reproduction of this article in the Background: Obesity is emerging as a global epidemic with part or total in any form is permis- growing threat to health in both developed and developing coun- sible with due acknowledgement of tries. It has become a major health concern for almost all the age the source. groups of the society. Objectives of the study is assess the preva- How to cite this article: lence and co-morbidities of overweight and obesity among per- Singh NP, Jain PK, Sharma RP, sons 15 years and above in urban and rural areas of Kanpur, UP. Chandra S, Nigam S, Singh A. As- Methods: For this cross-sectional study, multistage random sam- sessment of Magnitude and the Co- pling technique was used to select one colony in urban and one morbidities of Overweight and Obesity in Urban and Rural areas of village in rural area of Kanpur district. The desired sample size Kanpur. Natl J Community Med. was 2200. Detailed socio-demographic information was collected 2015; 6(1):1-5. on a pre-designed and pre-tested questionnaire. After anthropo- metric examination, Body Mass Index (BMI) was used to assess Author’s Affiliation: the overweight and obesity status. -

Farrukhabad, Etah and Hardoi Districts
78°0'0"E 78°30'0"E 79°0'0"E 79°30'0"E 80°0'0"E 80°30'0"E GEOGRAPHICAL AREA FARRUKHABAD, N ETAH AND HARDOI DISTRICTS " 0 ' 0 3 ° 8 ± 2 KEY MAP UTTAR PRADESH N " 0 ' 0 ° 8 2 Total Geographical Area (Sq Km) 10598 N No. of Charge Area 11 " 0 ' 0 ° Total Household 1328856 8 2 Total Population 7752529 CHARGE AREA ID NAME !( Jinhaira CA1 JALESAR !( !( !( !( CA2 ETAH Barai Bahbal Pur Jamura Mahmoodpur Saraiyan !( !( !( !( !( !( !( !( !( Udhranpur ManauraSongaraPilua Neorai Abdulla Nagar !( CA3 ALIGANJ Rarpatti !( !( !( Rabha !( Shahabad !( N !( ManjhilaKarawan X !( X Tumurki !( !( " !( Etah Bar!.thar !( Dahelia 0 !( !( Sahori !( ' Rafatnagar Senthara !( 0 !( Shitalpur !( CA4 KAIMGANJ !( Khadaua CA8 Itara 3 !( Kunwakhera Wazir Alam K!(han !( !( X ° Gahetu E T A H Raipur Khas Bagwala !( !( 7 Katiya Pithna Pur SHAHABAD !( !( CA2 Kansuri !( Parauli Suhagpur !( !( Kumhraur !( 2 Etah !( CA3 ChilouliM!(aursidabad !( Babasa !( Narainamau X Majhiya CA1 !( ETAH !( Dhumari Bharkhani Karim Nagar CA5 FARRUKABAD X !( X Jaithara ALIGANJ !( JALESAR Basundhara Angraiya Jamunai CA4 Amritpur Mansoor Nagar !( Khiriya Nagar S!(hah!( !( !( !( !( !( Malawan Targawan Aliganj (Dehat) KAIMGANJ !( Shahnagar Timarua !( Awagarh !( CA6 AMRITPUR Munder Behta Gokul !( !( Burrakalan X Chilsara !( CA6 !( Kurseli Shakrauli Lalpur N Jarani Khurd Kalan Tolwa Antdanpur " !( !( !( !( 0 !( AMRITPUR ' CA7 SAWAYAJPUR !( !( !( Umai Asadnagar X 0 Tikathar !( Pilkhana !( Bartal !( Rohina Mirzapur Khinmini !( !( 3 Nadraala ° !( Kurar Pura Bahadur F A R R U K H A B A D Kaurha 7 !( Farrukhabad -

Head, Department of Neurosurgery
1 Full Bio-data in 106 Pages PROF. (DR.) RAJ KUMAR Head, Department of Neurosurgery Co-chairman, United Nation Affair (World Kabaddi Federation) Sanjay Gandhi Post Graduate Institute of Medical Sciences Raebareli Road, Lucknow Ex-In charge Apex Trauma Centre, SGPGIMS Ex-Vice Chancellor Uttar Pradesh University of Medical Sciences, Saifai, Etawah Ex-Director All India Institute of Medical Sciences Rishikesh, Uttarakhand, India 2021 2 DR. RAJ KUMAR B.Sc., M.B.B.S., M.S., M.Ch., Ph.D., M.R.C.S., F.R.C.S., F.A.M.S., F.N.S., M.A.M.S, M.N.A.Sc., F.A.S.E.T, D.Sc. Profile __________________________________________________________________________ Personal Details: OFFICIAL ADDRESS : HOD, Department of Neurosurgery Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow (UP)-226014, India Contact Numbers : 0522-249-4735,0522-249-4771 Email : [email protected] PERMANENT ADDRESS : A/82, Omaxe city, Saheed Path, Opposite Ramabai Chauki & Ambedkar University, Lucknow, Uttar Pradesh, India-226025 E-mail : [email protected], Website : www.profrajkumar.com PERSONAL INFORMATION Father’s Name : Late Sri Chhote Lal Date of Birth : 15th December, 1959 Place of Birth : Village- Paman, Kanpur (Dehat), UP, India Nationality : Indian Marital Status : Married 3 OBJECTIVES As Professor: 1. To achieve excellence in medical and super speciality of Neurosurgery. 2. To render quality medical training, medical research & quality patient care. 3. To enhance reputation of country by relevant research in medical field of Neurosciences. 4. To develop centers of excellence in medical field. 5. Social awareness in young doctors and bright minds for developing International standard of patient care and health care system. -

District Census Handbook, Etawah, Part XIII-B, Series-22, Uttar Pradesh
,CENSUS' 1981 ·;"Ttl XIII - ~ I ' . , ~/SERIES·22i 'lff,"~' MqVfifl .... S1~~ ~~ ~ UTTAR'· ·PRADESH, Pt1rt XIII· B . PRIMARY CENSUS J,SST,RACl Nr'll {GmT !!tan ~"~T ·DISTlUCT ~~~~l ETAWAH DISTRICT CENSUS . HANDBOOK ~~ ~ ~vf.r" ftr ~;~~~, Qtlft, 1. SR=QTq.fT i-il 2. ' srrlf!fi'{<i' v-vi 3. f~~ <fiT ~T;rf",o;r ix-x 4. ~~~<11uf ari'Cfi~ s. fGfCifT Gf'flTll'f<rT ~R=;Cfir <fir qf~:qlf xi-xiii 6. f~T smrf1{Cfi iif~Hm: ~~Flt iif;:r~~t1T 18-17 7• ar~w:qcr iifrfcr~ ~ f¥i SlNf1{Cf) \ifiM''''<i'r~T~ 18-2,; 8, ~f.qij ;;t'f-~ffftff ~ full" 'SfNf'f'li iif;WIl'fi'f'Tl(fT, 26-33 9. ~1{)Jr/.'I1TU7.f ~T'rl'1{Cfi \jj;:r~lIFfHn, (;:r~'3Tm ~ UllIT c:f'fT 'f11'if it i(ri ~ ~~) 3S-lSl 1. t!~T q~" (i) CT~"r(:f1{r;;f," (ii) llnrl <fiT qllfliiiif q:;ft 36-39 (Iii)' 'n~T1Jf ~r~fq<fi iifif'l'olTifrrn 44-73 (iv) • <T'l1;Tll srr~f;r~ iifif~UFtRf" (~trSfT ;:r~~q'ffi;cy;T)' 74-75 ( v) ~cTqT iI1T~cnf(1Cfir <fiT qf~f~ 77-82 (vi) <T~Utr ~Tt:rf1{Cfi iifil1T1Jfi(f'lr, (iifijef"..crtilR iI1T,\q'rf(:f'Pr) 84-85 (vii) iifq<l~CA'IJ'\ ;:r~Cfrf.;;fCfir 'fiT q-f~f~c 87-88 (viii) iI1Ti'rlt ~r~f'fCfi ;r.pJ'G'fifmT-: (~f~~ ;;1H ~"I') 98-91 (i:l) ~f~~ .;,,~ ~"I' 'fir q'f'\f~c 93 2. ~,1AJ CI'~~" (i) tT~«~ ;rA'Rr-t (n) llnrl <tr q~ifilf q:qT 96-99 (iii) llr;rT1Jf ~~fqCfi Gfif~I!T'lHr~ 194-129 (iv) if~Tlt ~l'{flfCfi ~iI1T1Jfi(Tm\ (~n:''f;rr "I~\q'rf~'fiT) 139-131· (v) 'll~~ if~ \.qTf~lflr 'fiT qf,~ 132-133 (vi) 'Wf'rtr ~T'ff~ ~JFtT'3r'\ (~T iI1T{ ~"I') (vii) ~~ iflJ'\ ~'Jt Cfir qf(f~c ii 3. -

Vidhayak Nidhi
jkT;&m0izz0 MONTH -: NOVEMBER,2015 ¼/kujkf'k :0 esa½ 1 BALAMAU/ SHRI ANIL VERMA,MLA 330.430 1 HOUSE OF SHYAM LAL PASI 2015-16 4.9801 HOUSE OF SHYAM LAL 2015-16 4.980 2.980 2.980 GP,MAHRI HARDOI HOUSE OF SANTRAM IN PASI HOUSE OF SANTRAM GRAM MAHRI CC ROAD & IN GRAM MAHRI CC ROAD NALI & NALI 2 CONS. OF SCHOOL ROOMS & 2015-16 10.4402 CONS. OF SCHOOL 2015-16 10.440 10.440 10.440 MANAGER VARANDA IN SHRI ROOMS & VARANDA IN DEVIDAYAL INTER SHRI DEVIDAYAL INTER COLEGE,SHUBHAN KHERA COLEGE,SHUBHAN KHERA 3 CONS. OF ROOMS & 2015-16 15.0003 CONS. OF ROOMS & 2015-16 15.000 9.000 8.100 MANAGER VARANDA IN FATIMA VARANDA IN FATIMA DEGREE COLLEGE,SUBBA DEGREE COLLEGE,SUBBA KHERA GAURI KHALSA KHERA GAURI KHALSA 4 CONS.OF SCHOOL ROOMS & 2015-16 10.0804 CONS.OF SCHOOL ROOMS 2015-16 10.080 6.050 2.350 MANAGER VARANDA IN DR.BHEEMRAO & VARANDA IN AMBEDKAR SIKSHAN DR.BHEEMRAO SANSTHAN,PADRI AMBEDKAR SIKSHAN SANSTHAN,PADRI 5 CONS.OF SCHOOL ROOMS 2015-16 8.2905 CONS.OF SCHOOL ROOMS 2015-16 8.290 4.970 4.070 MANAGER IN SHRI DEVI DAYAL INTER IN SHRI DEVI DAYAL COLEGE,SHUBHAN KHERA INTER COLEGE,SHUBHAN KHERA 6 CONS. OF SCHOOL ROOMS 2015-16 10.0006 CONS. OF SCHOOL 2015-16 10.000 6.000 5.000 MANAGER IN JAI SHUBHAS MAHABALI ROOMS IN JAI SHUBHAS JUNIOR HIGH MAHABALI JUNIOR HIGH SCHOOL,DALEL NAGAR SCHOOL,DALEL NAGAR 7 CONS. OF SCHOOL ROOMS 2015-16 8.5007 CONS. -

Primary Educaticn Boys and Girls
REPORT PRIMARY EDUCATICN FOR BOYS AND GIRLS IN THE United Provinces o f Agra and Oudh WITH SPECIAL (REFERENCE TO UNECONOMICAL & SUPERFLUOUS SCHOOLS BY R. S. WEIR, M.A., B.SC., LE S., Assi.stant Director of Public Instruction, United Province;. -IOD-3J1 10037724 ALLAHABAD: ?KKmBO ABB StATIONEB?, DnTTID PeOTTNCES 372.9542 19 3 4 UNIP-P, 1934 X O D - 'I! CONTENTS Pages allysis ot Chapters . .. ■ .. v-vi VIPTKB I.—Introduction 1-4 II.—Trie Maps and the Statements 5 III.—Supsrduous and Uneconomical Schools 6-19 IV .—Training of Teachers 20-24 V .—School Buildings 25-31 VI.—Compulsory Mmary Education for Boys 32-41 ATTI.-Fees 42-46 V III.— Closure of Schools 47-49 IX .—Girls’ Sshools 50-54 X .—Schools for special classes 55-61 X I.—^Miscellaneous 62-65 X II.—Summary of recommendations 66-71 APPENDICES APPENDIX “ A ” —TABLES TabIuB I.—Statement showing number of institutions teaching up to pri mary and preparatory standard (with enrolment) main tained or aided by district boards on 31st October, 1933, (including schools for Maslims and depressed classes) 2 a II.—Statement showing number of primary and preparatory schools for boys, maintained or aided by district boards on 31st October, 1933, (including schools for Muslims and ■depressed classes) arranged according to enrolment 3a III.—^Statement showing number of primary schools for boys, maintained or aided by district boards on 31st October, 1933 (including schools for Muslims and depressed classes) with details of enrolment in class IV 4a IV.—Statement showing number of primary and preparatory schools for boys, maintained or aided by district boards, on 31st October, 1933 (including schools for Muslims and depressed classes) according to the number of teachers . -

List of Common Service Centres Established in Uttar Pradesh
LIST OF COMMON SERVICE CENTRES ESTABLISHED IN UTTAR PRADESH S.No. VLE Name Contact Number Village Block District SCA 1 Aram singh 9458468112 Fathehabad Fathehabad Agra Vayam Tech. 2 Shiv Shankar Sharma 9528570704 Pentikhera Fathehabad Agra Vayam Tech. 3 Rajesh Singh 9058541589 Bhikanpur (Sarangpur) Fatehabad Agra Vayam Tech. 4 Ravindra Kumar Sharma 9758227711 Jarari (Rasoolpur) Fatehabad Agra Vayam Tech. 5 Satendra 9759965038 Bijoli Bah Agra Vayam Tech. 6 Mahesh Kumar 9412414296 Bara Khurd Akrabad Aligarh Vayam Tech. 7 Mohit Kumar Sharma 9410692572 Pali Mukimpur Bijoli Aligarh Vayam Tech. 8 Rakesh Kumur 9917177296 Pilkhunu Bijoli Aligarh Vayam Tech. 9 Vijay Pal Singh 9410256553 Quarsi Lodha Aligarh Vayam Tech. 10 Prasann Kumar 9759979754 Jirauli Dhoomsingh Atruli Aligarh Vayam Tech. 11 Rajkumar 9758978036 Kaliyanpur Rani Atruli Aligarh Vayam Tech. 12 Ravisankar 8006529997 Nagar Atruli Aligarh Vayam Tech. 13 Ajitendra Vijay 9917273495 Mahamudpur Jamalpur Dhanipur Aligarh Vayam Tech. 14 Divya Sharma 7830346821 Bankner Khair Aligarh Vayam Tech. 15 Ajay Pal Singh 9012148987 Kandli Iglas Aligarh Vayam Tech. 16 Puneet Agrawal 8410104219 Chota Jawan Jawan Aligarh Vayam Tech. 17 Upendra Singh 9568154697 Nagla Lochan Bijoli Aligarh Vayam Tech. 18 VIKAS 9719632620 CHAK VEERUMPUR JEWAR G.B.Nagar Vayam Tech. 19 MUSARRAT ALI 9015072930 JARCHA DADRI G.B.Nagar Vayam Tech. 20 SATYA BHAN SINGH 9818498799 KHATANA DADRI G.B.Nagar Vayam Tech. 21 SATYVIR SINGH 8979997811 NAGLA NAINSUKH DADRI G.B.Nagar Vayam Tech. 22 VIKRAM SINGH 9015758386 AKILPUR JAGER DADRI G.B.Nagar Vayam Tech. 23 Pushpendra Kumar 9412845804 Mohmadpur Jadon Dankaur G.B.Nagar Vayam Tech. 24 Sandeep Tyagi 9810206799 Chhaprola Bisrakh G.B.Nagar Vayam Tech. -

Uttar Pradesh University of Medical Sciences, Saifai, Etawah
Uttar Pradesh University of Medical Sciences, Saifai, Etawah Faculty of Medicine/Dental (UG (MBBS) and PG (MD/MS/MDS) Academic Calendar (Terminal/University Examinations & Vacations) Year 2020 Sl Activity Tentative Dates Remarks PG (MD/MS/MDS) 1 Submission of Synopsis for JR-1 (admitted batch) Last date for submission 31.10.2020 2 Submission of Thesis for JR-3 (final year) 3 University Examination (MAIN) 13.04.2020 to 17.04.2020 Dates of practical exam will be finalized by HODs 4 University Examination (SUPP.) 05.10.2020 to 09.10.2020 Dates of practical exam will be finalized by HODs MBBS First Year (ANATOMY, PHYSIOLOGY, BIOCHEMISTRY) 1 1st Terminal for 1st Prof. ( 1st Semester) 27.01.2020 to 04.02.2020 - 2 2nd Terminal for 1st Prof (2nd Semester) 20.04.2020 to 28.04.2020 - 3 Pre University Exam for 1st Prof (2nd Semester) 05.08.2020 to 13.08.2020 - 4 FIRST RPOF EXAM 01.09.2020 to 08.09.2020 Dates of practical exam will be finalized by HODs 5 FIRST RPOF EXAM (SUPP.) 11.12.2020 to 18.12.2020 Dates of practical exam will be finalized by HODs MBBS Second Year (PATHOLOGY, MICROBIOLOGY, PHARMACOLOGY, FORENSIC MEDICINE) 1 1st Terminal for 2nd Prof (3rd and 4th semester) 19.08.2020 to 27.08.2020 Exam held in Morning Session 2 2nd Terminal for 2nd Prof (5th semester) 28.01.2020 to 06.02.2020 - 3 SECOND PROF EXAM 17.03.2020 to 26.03.2020 Dates of practical exam will be finalized by HODs 4 SECOND PROF EXAM (SUPP.) 11.09.2020 to 21.09.2020 Dates of practical exam will be finalized by HODs MBBS Third Year (COMMUNITY MEDICINE, E.N.T., OPHTHALMOLOGY) 1st Terminal for Final Prof. -

Hardoi Dealers Of
Dealers of Hardoi Sl.No TIN NO. UPTTNO FIRM - NAME FIRM-ADDRESS 1 09153800008 HD0047653 TANDAN TUVELS CINEMA ROAD HARDOI 2 09153800013 HD0002472 RAJ MADICAL HALL CINEMA ROAD HARDOI 3 09153800027 HD0013596 RAKESH MEDICINE ARYA KANYA PATHASHALA HARDOI 4 09153800032 HD0009363 AGARWAL KIRANA STORS RAILWAYGANJ HARDOI 5 09153800046 HD0001175 BANWARI LAL ANANTRAM SADAR BAZAR HARDOI 6 09153800051 HD0024972 PUBLIC GENRRAL STORE CINAMA ROAD HARDOI 7 09153800065 HD0043341 MAHENDRA PRATAP SINGH P.W.D LUCKNOW ROAD HARDOI CONT. 8 09153800070 HD0030017 MOHANLAL SATAYPARKASH RAILWAY GANJ HARDOI. 9 09153800079 HD0032398 RAJ BRICK FIELD JADSARA SANDILA 10 09153800084 HD0032349 RAMSHAY RAKESH KUMAR NAVIN MANDI HARDOI 11 09153800107 HD0036941 MUNGIA BRICK FIELD SANDILA HARDOI 12 09153800112 HD0038201 BEAUTY CENTER SANDILA HARDOI 13 09153800126 HD0033251 JAGAT TRADINGS MEDICAL STORES BENIGANJ HARDOI 14 09153800131 HD0039619 PREM PRAKAS AGRWAL CONTRACTOR KACHAUNA HARDOI 15 09153800145 HD0041223 QUILTY RADIO ADN WATCH EMPORAM SANDILA HARDOI 16 09153800150 HD0040221 U.P. STATE SUGER CORPO.LTD.UNITE RLY GANJ HARDOI 17 09153800164 HD0042844 RAM VILASH BAJPAI CONTRACTOR SARAY THOAK PACHIMI HARDOI 18 09153800178 HD0044817 MOHD.HANIF SANDILA HARDOI 19 09153800197 HD0045713 BHARAT SABUN BHANDAR RAILWAY GANJ HARDOI 20 09153800206 HD0046209 M.S.TRADERS SANDILA HARDOI 21 09153800211 HD0046210 AJANTA TRADERS ANAND TALKIES KA PAS HARDOI 22 09153800225 HD0047826 PEKAL TRADERS DHARMSHALA ROAD HAROI 23 09153800230 HD0047881 UDAT PRAKASH AND CO.GALLA NAVIN MANDI STHAL HARDOI BYAPARI 24 09153800239 HD0052339 NEERAJ KUMAR GUPTA PITAMBAR GANJ HARDOI 25 09153800244 HD0044476 PANDAY BRICK FIELD THEKUNNI SANDILA 26 09153800258 HD0048667 MADAN MODERN RICE & DAL MILL SANDILA HARDOI 27 09153800263 HD0048756 NAVNEET KIRANA STORE BAGHAULI BAZAR HARDOI 28 09153800277 HD0040367 NEW INDIA FERMITICALS ALU THOK HARDOI 29 09153800282 HD0050853 PRATAK TIMBER KAINAL ROAD HARDOI 30 09153800296 HD0050032 SHRI KRISHNA GUPTA MINI RICE MIL HARDOI 31 09153800305 HD0051034 KHANNA RADIO AND WATCH CO. -

Automatic Weather Station Network of Uttar Pradesh
AUTOMATIC WEATHER STATION NETWORK OF UTTAR PRADESH S.No. District AWS Station Address 1. Agra Agra Dir I/C FMO, Hydrogen Factory, Agra 2. Aigarh Aligarh ADM, Finance, Aligarh. (Collectorate) 3. Etah Etah DM, Etah (Collectorate) 4. Etawah Etawah Baba Saheb Dr. B.R.A. College of Agriculture Engineering & Technology, Etawah. 5. Hathras Hathras DM, Hathras. (Collectorate) 6. Mainpuri Mainpuri Tehshildar Sadar, Mainpuri 7. Mathura Mathura DM, Mathura (Collectorate) 8. Allahabad Allahabad Dean, College of Forestry, Allahabad Agricultural Institute, Allahabad 9. Chitrakoot Karwi ADM (Relief) Sonepur,Karwi, Chitrakoot 10. Faizabad Faizabad DM, Firozabad ( Collectorate) 11. Fatehpur Fatehpur Officer In-Charge Nazarat, Fatehpur 12. Kaushambi Kokhraj Farm Suprientendent, Govt. Agri. Farm, Khokhraj, Kaushambi. 13. Meerut Meerut Chaudhry Charan Singh University campus, Meerut c/o M.O.Meerut 14. Bulandshahar Bulandshahar Marathwada Institute,Dhamerchola ,Bulandshahar 15. Lucknow Lucknow Director I/C, Met Centre, Lucknow 16. Aurraiya Aurraiya D.M. Aurraiya (Collectorate) 17. Bharaich Bahraich Officer In-charge, Crop Research Station, N.D. University of Agri & Tech, Baharaich. 18. Gonda Gonda ADM, Gonda 19. Kannauj Kannauj D.M. kannauj. (Collectorate) 20. Kanpur City Kanpur Dept. of Agronomy, Chandra Shekhar Azad University of Agriculture, Kanpur 21. Kanpur Dehat Akabarpur DM Kanpur Dehat, (Akabarpur) 22. Raebareili Fursatganj Senior ATC Officer , IGRUA, Fursatganj, Raebareli C/o M.O.Fursatganj 23. Sultanpur Sultanpur Krishi Vigyan Kendra, C/o Met. Office K.N.I.T.,Sultanpur C/O M.O.Sultanpur 24. Unnao Unnao Dy. Dir Agri. Unnao 25. Bareilly Bareilly DM, Barailly (Collectorate) 26. Badaun Badaun DM, Badaun (Collectorate) 27. Lakhimpur Kheri Palliakalan BDO, Vikash Khand Bhawan, Paliakalan, Lakhimpurkheri.