Melioidosis Fact Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2012 Case Definitions Infectious Disease
Arizona Department of Health Services Case Definitions for Reportable Communicable Morbidities 2012 TABLE OF CONTENTS Definition of Terms Used in Case Classification .......................................................................................................... 6 Definition of Bi-national Case ............................................................................................................................................. 7 ------------------------------------------------------------------------------------------------------- ............................................... 7 AMEBIASIS ............................................................................................................................................................................. 8 ANTHRAX (β) ......................................................................................................................................................................... 9 ASEPTIC MENINGITIS (viral) ......................................................................................................................................... 11 BASIDIOBOLOMYCOSIS ................................................................................................................................................. 12 BOTULISM, FOODBORNE (β) ....................................................................................................................................... 13 BOTULISM, INFANT (β) ................................................................................................................................................... -
AMD Projects: Deadly Disease Databases
CDC’s AMD Program AMD Projects Innovate • Transform • Protect CDC’s Advanced Molecular Detection (AMD) program fosters scientific innovation in genomic sequencing, epidemiology, and bioinformatics to transform public health and protect people from disease threats. AMD Project: Deadly Disease Databases Whole genome analysis and database development for anthrax (Bacillus anthracis), melioidosis (Burkholderia pseudomallei), and Brucellosis (Brucella spp.) Epidemiologists and forensic professionals can use whole genome sequencing – a way of determining an organism’s complete, detailed genome – and large databases to determine the source of dangerous germs. Having a large, accessible collection of disease pathogens could help scientists quickly find out if a certain illness is naturally occurring or the result of bioterrorism. CDC is establishing a public database where scientists from around the world can share information about these potentially deadly CDC is establishing public databases so that diseases. CDC scientists have begun sequencing the organisms that scientists from around the world can share information about deadly diseases like cause anthrax (Bacillus anthracis), brucellosis (Brucella spp.), and anthrax, brucellosis, and melioidosis. melioidosis (Burkholderia pseudomallei), three pathogens that could occur naturally or as the result of bioterrorism. Current methods of determining the genetic structure of these organisms are not standardized and sometimes not effective. Using whole genome sequencing for these pathogens will allow scientists www.cdc.gov/amd Updated: May 2017 to accurately and quickly find the geographic origin of the isolates and will improve overall knowledge and understanding of them. Having a detailed database of these genomes will also ensure quicker and more effective responses to outbreaks. For more information on anthrax, please visit www.cdc.gov/anthrax/index.html. -
Insights Into the Pathogenicity of Burkholderia Pseudomallei
REVIEWS Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei W. Joost Wiersinga*, Tom van der Poll*, Nicholas J. White‡§, Nicholas P. Day‡§ and Sharon J. Peacock‡§ Abstract | Burkholderia pseudomallei is a potential bioterror agent and the causative agent of melioidosis, a severe disease that is endemic in areas of Southeast Asia and Northern Australia. Infection is often associated with bacterial dissemination to distant sites, and there are many possible disease manifestations, with melioidosis septic shock being the most severe. Eradication of the organism following infection is difficult, with a slow fever-clearance time, the need for prolonged antibiotic therapy and a high rate of relapse if therapy is not completed. Mortality from melioidosis septic shock remains high despite appropriate antimicrobial therapy. Prevention of disease and a reduction in mortality and the rate of relapse are priority areas for future research efforts. Studying how the disease is acquired and the host–pathogen interactions involved will underpin these efforts; this review presents an overview of current knowledge in these areas, highlighting key topics for evaluation. Melioidosis is a serious disease caused by the aerobic, rifamycins, colistin and aminoglycosides), but is usually Gram-negative soil-dwelling bacillus Burkholderia pseu- susceptible to amoxicillin-clavulanate, chloramphenicol, domallei and is most common in Southeast Asia and doxycycline, trimethoprim-sulphamethoxazole, ureido- Northern Australia. Melioidosis is responsible for 20% of penicillins, ceftazidime and carbapenems2,4. Treatment all community-acquired septicaemias and 40% of sepsis- is required for 20 weeks and is divided into intravenous related mortality in northeast Thailand. Reported cases are and oral phases2,4. Initial intravenous therapy is given likely to represent ‘the tip of the iceberg’1,2, as confirmation for 10–14 days; ceftazidime or a carbapenem are the of disease depends on bacterial isolation, a technique that drugs of choice. -
Antigen Detection Assay for the Diagnosis of Melioidosis
PI: Title: Antigen Detection assay for the Diagnosis of Melioidosis Received: 12/05/2013 FOA: PA10-124 Council: 05/2014 Competition ID: ADOBE-FORMS-B1 FOA Title: NIAID ADVANCED TECHNOLOGY STTR (NIAID-AT-STTR [R41/R42]) 2 R42 AI102482-03 Dual: Accession Number: 3650491 IPF: 3966401 Organization: INBIOS INTERNATIONAL, INC. Former Number: Department: IRG/SRG: ZRG1 IDM-V (12)B AIDS: N Expedited: N Subtotal Direct Costs Animals: N New Investigator: N (excludes consortium F&A) Humans: Y Early Stage Investigator: N Year 3: Clinical Trial: N Year 4: Current HS Code: E4 Year 5: HESC: N Senior/Key Personnel: Organization: Role Category: Always follow your funding opportunity's instructions for application format. Although this application demonstrates good grantsmanship, time has passed since the grantee applied. The sample may not reflect the latest format or rules. NIAID posts new samples periodically: https://www.niaid.nih.gov/grants-contracts/sample-applications The text of the application is copyrighted. You may use it only for nonprofit educational purposes provided the document remains unchanged and the PI, the grantee organization, and NIAID are credited. Note on Section 508 conformance and accessibility: We have reformatted these samples to improve accessibility for people with disabilities and users of assistive technology. If you have trouble accessing the content, please contact the NIAID Office of Knowledge and Educational Resources at [email protected]. Additions for Review Accepted Publication Accepted manuscript news Post-submission supplemental material. Information about manuscript accepted for publication. OMB Number: 4040-0001 Expiration Date: 06/30/2011 APPLICATION FOR FEDERAL ASSISTANCE 3. DATE RECEIVED BY STATE State Application Identifier SF 424 (R&R) 1. -
Disease Control Newsletter Is Available on the MDH IDCN Web Site: (
ISEASE ONTROL EWSLETTER DVolume 46, Number 1 (pages 1-30) C N 2019 Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2018 Introduction Anaplasmosis Assessment of the population’s health is a core public health function. Anaplasmosis, caused by Anaplasma Surveillance for communicable diseases is one type of assessment. Epidemiologic phagocytophilum, is transmitted surveillance is the systematic collection, analysis, and dissemination of health by bites from Ixodes scapularis, data for the planning, implementation, and evaluation of health programs. the blacklegged tick. Although the The Minnesota Department of Health (MDH) collects information on infectious organism that causes anaplasmosis diseases for the purposes of determining disease impact, assessing trends in was previously known by other disease occurrence, characterizing affected populations, prioritizing control names and thought to be a part of efforts, and evaluating prevention strategies. Prompt reporting allows outbreaks the genus Ehrlichia, anaplasmosis and to be recognized in a timely fashion when control measures are most likely to be ehrlichiosis (due to E. chaffeensis) are effective in preventing additional cases. distinct diseases caused by different rickettsial species. The same tick vector In Minnesota, communicable disease reporting is centralized, whereby reporting also transmits the etiologic agents of sources submit standardized reports to MDH. Cases of disease are reported Lyme disease, babesiosis, ehrlichiosis pursuant to Minnesota Rules Governing Communicable Diseases (Minnesota (due to E. muris), and Powassan Rules 4605.7000 -4605.7800). The diseases listed in Table 1 must be reported virus. In rare circumstances, A. to MDH. As stated in the rules, physicians, health care facilities, laboratories, phagocytophilum may be transmitted veterinarians, and others are required to report these diseases. -
Monthly Reportable Diseases Summary
Monthly Reportable Diseases Summary June 2021 The data in the Monthly Disease Reports are provisional, based on current reports in the Michigan Disease Surveillance System (MDSS) made by local public health departments. The MDSS is a dynamic, continually active system; counts of disease are constantly changing as cases are investigated, confirmed as cases, or ruled out as not meeting the case definition. Each Monthly Disease Report reflects this constant activity as the numbers may slightly fluctuate each month. Therefore, it should be kept in mind that numbers in the Monthly Disease Reports are NOT final and should be used only to generally monitor Ottawa County trends over time. Unknown, suspect, probable and confirmed cases of the reportable condition are included in the report. An updated report is published each month. Specific data requests and questions should be directed to the following: Compiled by Derick N. Chia, MPH Epidemiologist [email protected] We value your feedback. Please use this QR code or click on the link below to tell us what you think of this report: Link to Survey 12251 James Street Holland, MI 49424-9661 www.miottawa.org/healthdata June 2021 Reportable conditions that are italicized have an accompanying graph at the end of the monthly section. Cases Reported in Last 4 Months** Year Total Through June Year End Disease Group Reportable Condition Mar-21 Apr-21 May-21 Jun-21 2018 2019 2020 2021 2020 Foodborne Amebiasis - 1 - - - - - 1 - Botulism - Foodborne - - - - - - - - - Campylobacter 2 4 1 6 33 29 16 22 -

Scientific Consultation Summary
GLOBAL ANTIBIOTIC RESEARCH AND DEVELOPMENT (GARD) PARTNERSHIP Developing new antibiotic treatments, promoting responsible SCIENTIFIC use, and ensuring access for all A joint WHO/DNDi initiative incubated by DNDi in CONSULTATION support of the Global Action Plan for Antimicrobial Resistance SUMMARY Institut Pasteur, France / 29 February 2016 Background Following recommendations made during the technical consultation meeting in November 2015 at the World Health Organization, GARD rapidly undertook an informal process of scoping for potential initial project proposals. A set of general selection criteria was established and a basic template was circulated to GARD’s scientific contacts and networks. This was not a broad call for proposals as GARD is currently at the very early stages of incubation and would require greater resources in order to manage such a process. The template is now online. This process, which began late December 2015 and is still ongoing, rendered 10 project proposals that were discussed during the meeting after briefings with each of the project proposers as the projects were being developed. The aim of this initial scientific consultation was to help GARD evolve from the initial scientific strategy articulated in the initial and revised GARD concept notes, determine priority areas and short- to medium-term projects to be launched within one year. Longer-term (upstream) projects will also be considered as GARD builds its R&D pipeline. Summary of discussions The following aims to provide a summary of the discussions of the 29 February meeting. Introductory presentations were made in order to provide a common context in which the projects were to be discussed, including the respective roles of DNDi and WHO in GARD, the work of WHO, the emphasis on embedding conservation and access in each project from the outset, and the need to consider diagnostics in the R&D equation. -

Development of Diagnostic Assays for Melioidosis, Tularemia, Plague And
University of Nevada, Reno Development of Diagnostic Assays for Melioidosis, Tularemia, Plague and COVID19 A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Cellular and Molecular Biology By Derrick Hau Dr. David P. AuCoin / Dissertation Advisor December 2020 THE GRADUATE• SCHOOL We recommend that the dissertation prepared under our supervision by entitled be accepted in partial fulfillment of the requirements for the degree of Advisor Committee Member Committee Member Committee Member Graduate School Representative David W. Zeh, Ph.D., Dean Graduate School December 2020 i Abstract Infectious diseases are caused by pathogenic organisms which can be spread throughout communities by direct and indirect contact. Burkholderia pseudomallei, Francisella tularenisis, and Yersinia pestis are the causative agents of melioidosis, tularemia and plague, respectively. These bacteria pertain to the United States of America Federal Select Agent Program as they are associated with high mortality rates, lack of medical interventions and are potential agents of bioterrorism. The novel coronavirus disease (COVID-19) has resulted in a global pandemic due to the highly infectious nature and elevated virulence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Proper diagnosis of these infections is warranted to administer appropriate medical care and minimize further spreading. Current practices of diagnosing melioidosis, tularemia, plague and COVID-19 are inadequate due to limited resources and the untimely nature of the techniques. Commonly, diagnosing an infectious disease is by the direct detection of the causative agent. Isolation by bacterial culture is the gold standard for melioidosis, tularemia and plague infections; detection of SAR-CoV-2 nucleic acid by real-time polymerase chain reaction (RT-PCR) is the gold standard for diagnosing COVID-19. -
Guidelines for the Evaluation of Transfusion-Associated Infections
New York State Council on Human Blood and Transfusion Services GUIDELINES FOR THE EVALUATION OF TRANSFUSION-ASSOCIATED INFECTIONS Third Edition 2007 New York State Council on Human Blood and Transfusion Services New York State Department of Health Wadsworth Center Empire State Plaza; P.O. Box 509 Albany, New York 12201-0509 Third Edition 2007, Second Edition 1996, First Edition 1994 Requests for copies of this publication may be directed to: Blood and Tissue Resources Program New York State Department of Health Wadsworth Center Empire State Plaza P.O. Box 509 Albany, New York 12201-0509 Telephone: (518) 485-5341 Fax: (518) 485-5342 E-mail: [email protected] Website: www.wadsworth.org/labcert/blood_tissue NEW YORK STATE COUNCIL ON HUMAN BLOOD AND TRANSFUSION SERVICES Membership Roster – 2007 Donna Skerrett, M.D., M.S., Chairperson Kathleen Grima, M.D. Director Director Transfusion Medicine and Cellular Therapy New York Blood Center Clinical Services New York Presbyterian Hospital - White Plains, New York Weill Cornell Medical Center New York, New York Nadia Rajsz, M.S., MT(ASCP) Glen Spey, New York Joseph Chiofolo, D.O. Medical Director Lazaro Rosales, M.D. Transfusion Service Director Winthrop University Hospital Blood Bank Mineola, New York SUNY Health Science Center at Syracuse Robert A. Dracker, M.D., M.H.A. Syracuse, New York Medical Director Summerwood Pediatrics and Richard F. Daines, M.D. Infusacare Medical Services (Ex-officio) Liverpool, New York Commissioner New York State Department of Health William Fricke, M.D. Albany, New York Director Transfusion Service & Hematology Laboratory Jeanne V. Linden, M.D., M.P.H. -

Medicine Review Course Animal Bites (Dogs, Cats, Monkeys)
Medicine review course Animal bites (dogs, cats, monkeys) 8/7/17 Assessment of a bite (the crude history) 1) Where (the circumstances) did the bite occur? 2) Where (on the body) did the bite occur? 3) Time from bite to presentation? 4) Extent of wound? 5) Host immunocompetence? 6) Host vaccination history? The answers to these questions will provide……. Assessment of a bite (the refined history) 1) The potential organisms (from the animal’s surroundings, from the animal’s flora, from the patient’s skin) 2) The need to image deeper tissues and activate more than the ID-on-call (Ortho, GS, vascular, ….) 3) The maximal potential extent of this injury 4) Wound treatment, antibiotics, vaccination and follow-up required. Dogs and cats 1) Potential organisms -Consider rabies in wild dogs, in non-rabies free countries, in unprovoked attacks. -Consider soil derived organisms(clostridium tetanus, melioidosis) in wild dogs -Consider bacillus anthracis in farm dogs -Consider capnocytophaga carnimorsus and pasteurella species in exams! 2) Deeper tissues imaging -Consider bone and joint involvement if wound is deep -Look out for presence of prosthetic joints. -cats can bite deep. Small wound can be deeply punctured 3) Maximal potential -Melioidosis in poorly controlled DM -Deeper infection in breast cancer patients post axillary clearance -Disseminated capnocytophaga carnimorsus in asplenia -Tetanus and rabies in bites close to face Rabies Duration (% of Stage Associated Findings Cases) <30 d (25%) 30-90 d (50%) Incubation period None. 90 d to 1 y (20%) >1 y (5%) Paresthesias or pain at the Prodrome and early wound site; fever; malaise; 2-10 d symptoms anorexia; nausea and vomiting. -
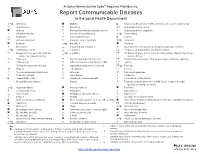
Report Communicable Diseases to the Local Health Department
Arizona Administrative Code Requires Providers to: Report Communicable Diseases to the Local Health Department *O Amebiasis Glanders O Respiratory disease in a health care institution or correctional facility Anaplasmosis Gonorrhea * Rubella (German measles) Anthrax Haemophilus influenzae, invasive disease Rubella syndrome, congenital Arboviral infection Hansen’s disease (Leprosy) *O Salmonellosis Babesiosis Hantavirus infection O Scabies Basidiobolomycosis Hemolytic uremic syndrome *O Shigellosis Botulism *O Hepatitis A Smallpox Brucellosis Hepatitis B and Hepatitis D Spotted fever rickettsiosis (e.g., Rocky Mountain spotted fever) *O Campylobacteriosis Hepatitis C Streptococcal group A infection, invasive disease Chagas infection and related disease *O Hepatitis E Streptococcal group B infection in an infant younger than 90 days of age, (American trypanosomiasis) invasive disease Chancroid HIV infection and related disease Streptococcus pneumoniae infection (pneumococcal invasive disease) Chikungunya Influenza-associated mortality in a child 1 Syphilis Chlamydia trachomatis infection Legionellosis (Legionnaires’ disease) *O Taeniasis * Cholera Leptospirosis Tetanus Coccidioidomycosis (Valley Fever) Listeriosis Toxic shock syndrome Colorado tick fever Lyme disease Trichinosis O Conjunctivitis, acute Lymphocytic choriomeningitis Tuberculosis, active disease Creutzfeldt-Jakob disease Malaria Tuberculosis latent infection in a child 5 years of age or younger (positive screening test result) *O Cryptosporidiosis -
DEPARTMENT of VETERANS AFFAIRS 8320-01 38 CFR Part 4
This document is scheduled to be published in the Federal Register on 06/18/2019 and available online at https://federalregister.gov/d/2019-12682, and on govinfo.gov DEPARTMENT OF VETERANS AFFAIRS 8320-01 38 CFR Part 4 RIN 2900-AQ43 Schedule for Rating Disabilities; Infectious Diseases, Immune Disorders, and Nutritional Deficiencies AGENCY: Department of Veterans Affairs. ACTION: Final rule. SUMMARY: This document amends the Department of Veterans Affairs (VA) Schedule for Rating Disabilities (VASRD) by revising the portion of the schedule that addresses infectious diseases, immune disorders, and nutritional deficiencies. The effect of this action is to ensure that the rating schedule uses current medical terminology and to provide detailed and updated criteria for evaluation of infectious diseases, immune disorders, and nutritional deficiencies for disability rating purposes. DATES: Effective Date: This final rule is effective August 11, 2019. FOR FURTHER INFORMATION CONTACT: Ioulia Vvedenskaya, M.D., M.B.A., Medical Officer, Part 4 VASRD Regulations Staff (211C), Compensation Service, Veterans Benefits Administration, Department of Veterans Affairs, 810 Vermont Avenue, NW, Washington, DC 20420, [email protected], (202) 461- 9700 (This is not a toll-free telephone number). SUPPLEMENTARY INFORMATION: VA published a proposed rule in the Federal Register at 84 FR 1678 on February 5, 2019, to amend 38 CFR 4.88a and 4.88b, the portion of the VASRD dealing with infectious diseases, immune disorders, and nutritional deficiencies. VA provided a 60-day public comment period, and interested persons were invited to submit written comments on or before April 8, 2019. VA received 32 comments. One commenter supported VA’s intent to eliminate obsolete terminology and substitute the most up-to-date terms and definitions for conditions such as Chronic Fatigue Syndrome.