B.Pharm 5Th Semester Pharmacology-Ii
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tachykinins in the Gut. Part II. Roles in Neural Excitation, Secretion and Inflammation
Pfxnma~ol.Ther. Vol. 73, No. 3, pp. 219-263, 1997 ISSN 0163-7258197$32.00 CopyrIght0 1997 ElsevierScience Inc. PI1 SO163-7258(96)00196-9 ELSEVIER A.wciate Editor: 1. We&r Tachykinins in the Gut. Part II. Roles in Neural Excitation, Secretion and Inflammation Peter Holzer” and Ulrike Holw-er-Pets&e DEPARTMENT0FEXPERIMENTALANDCLINlCALPHARMACOLOGY,UNIVERSlTYOFGRAZ,UNlVERSITiiTSPLATZ4,A-8010GRAZ,AUSTRIA ABSTRACT. The preprotachykinin-A gene-derived peptides substance (substance P; SP) and neurokinin (NK) A are expressed in intrinsic enteric neurons, which supply all layers of the gut, and extrinsic primary afferent nerve fibers, which innervate primarily the arterial vascular system. The actions of tachykinins on the digestive effector systems are mediated by three different types of tachykinin receptor, termed NK,, NKr and NK, receptors. Within the enteric nervous system, SP and NKA are likely to mediate, or comediate, slow synaptic transmission and to modulate neuronal excitability via stimulation of NK, and NK, receptors. In the intestinal mucosa, tachykinins cause net secretion of fluid and electrolytes, and it appears as if SP and NKA play a messenger role in intramural secretory reflex pathways. Secretory processes in the salivary glands and pancreas are likewise influenced by tachykinins. The gastrointestinal arterial system may be dilated or constricted by tachykinins, whereas constriction and an increase in the vascular permeability are the only effects seen in the venous system. Various gastrointestinal disorders are associated with distinct changes in the tachykinin system, and there is increasing evidence that tachykinins participate in the hypersecretory, vascular and immunological disturbances associated with infection and inflammatory bowel disease. In a therapeutic perspective, it would seem conceivable that tachykinin antagonists could be exploited as antidiarrheal, anti- inflammatory and antinociceptive drugs. -

Eicosanoids & Platelet Activating Factor
Eicosanoids & Platelet Activating Factor Prof. Sanjay Khattri Dept. of Pharmacology & Therapeutics King George’s Medical University, Lucknow 1 Autacoid These are the substances produced by wide variety of cells that act locally at the site of production. (local hormones) 2 Mediators of Inflammation and Immune reaction 1. Vasoactive amines (Histamine and Serotonin) 2.Eicosanoids 3.Platlet Activating Factor 4.Bradykinins 4.Nitric Oxide 5.Neuropeptides 6.Cytokinines 3 EICOSANOIDS PGs, TXs and LTs are all derived from eicosa (referring to 20 C atoms) tri/tetra/ penta enoic acids. Therefore, they can be collectively called eicosanoids. Major source: 5,8,11,14 eicosa tetraenoic acid (arachidonic acid). Other eicosanoids of increasing interest are: lipoxins and resolvins. The term prostanoid encompasses both prostaglandins and thromboxanes. 4 EICOSANOIDS Contd…. In most instances, the initial and rate-limiting step in eicosanoid synthesis is the liberation of intracellular arachidonate, usually in a one-step process catalyzed by the enzyme phospholipase A2 (PLA2). PLA2 generates not only arachidonic acid but also lysoglyceryl - phosphorylcholine (lyso-PAF), the precursor of platelet activating factor (PAF). 5 EICOSANOIDS Contd…. Corticosteroids inhibit the enzyme PLA2 by inducing the production of lipocortins (annexins). The free arachidonic acid is metabolised separately (or sometimes jointly) by several pathways, including the following: Cyclo-oxygenase (COX)- Two main isoforms exist, COX-1 and COX-2 Lipoxygenases- Several subtypes, which -

Histamine and Antihistamines Sites of Action Conditions Which Cause Release Aron H
Learning Objectives I Histamine Pharmacological effects Histamine and Antihistamines Sites of action Conditions which cause release Aron H. Lichtman, Ph.D. Diagnostic uses Associate Professor II Antihistamines acting at the H1 and H2 receptor Pharmacology and Toxicology Pharmacological effects Mechanisms of action Therapeutic uses Side effects and drug interactions Be familiar with the existence of the H3 receptor III Be able to describe the main mechanism of action of cromolyn sodium and its clinical uses Histamine Pharmacology First autacoid to be discovered. (Greek: autos=self; Histamine Formation akos=cure) Synthesized in 1907 Synthesized in mammalian tissues by Demonstrated to be a natural constituent of decarboxylation of the amino acid l-histidine mammalian tissues (1927) Involved in inflammatory and anaphylactic reactions. Local application causes swelling redness, and edema, mimicking a mild inflammatory reaction. Large systemic doses leads to profound vascular changes similar to those seen after shock or anaphylactic origin Histamine Stored in complex with: Heparin Chondroitin Sulfate Eosinophilic Chemotactic Factor Neutrophilic Chemotactic Factor Proteases 1 Conditions That Release Histamine 1. Tissue injury: Any physical or chemical agent that injures tissue, skin or mucosa are particularly sensitive to injury and will cause the immediate release of histamine from mast cells. 2. Allergic reactions: exposure of an antigen to a previously sensitized (exposed) subject can immediately trigger allergic reactions. If sensitized by IgE antibodies attached to their surface membranes will degranulate when exposed to the appropriate antigen and release histamine, ATP and other mediators. 3. Drugs and other foreign compounds: morphine, dextran, antimalarial drugs, dyes, antibiotic bases, alkaloids, amides, quaternary ammonium compounds, enzymes (phospholipase C). -
The Value of Urotensin II in Patients with Left-Sided Rheumatic Valvular Regurgitation
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector The Egyptian Heart Journal (2016) xxx, xxx–xxx HOSTED BY Egyptian Society of Cardiology The Egyptian Heart Journal www.elsevier.com/locate/ehj www.sciencedirect.com The value of urotensin II in patients with left-sided rheumatic valvular regurgitation Ibrahim Elmadbouh a,*, Mahmoud Ali Soliman b, Ahmed Abdallah Mostafa c, Haitham Ahmed Heneish d a Biochemistry Department, Faculty of Medicine, Menoufia University, Egypt b Cardiology Department, Faculty of Medicine, Menoufia University, Egypt c Cardiology Department, Police Academy Hospital, Egypt d Cardiology Department, Nasser Institute Hospital, Egypt Received 20 May 2016; accepted 24 September 2016 KEYWORDS Abstract Aims: Rheumatic valve diseases are most common etiological valve diseases in develop- Urotensin II; ing countries. Urotensin II is cardiovascular autacoid/hormone and may be associated with patients Mitral regurgitation; of heart valve diseases. The present study was to measure plasma urotensin II concentrations in Cardiovascular autacoid patients with left-sided rheumatic valve diseases such as mitral regurgitation (MR) and aortic regur- hormone gitation (AR), and to examine its correlation with severity of valve impairment, function (New York Heart association, NYHA) class and pulmonary artery pressure (PAP). Methods and results: Sixty patients with moderate to severe rheumatic left-sided valve regurgitation and 20 healthy controls were selected after performing the echocardiography. Plasma urotensin II level was measured in all subjects. The patients with MR and AR were significantly increased of left ventricular end diastolic dimension (LVEDD), left ventricular end systolic dimension (LVESD), left atrial diameter, PAP, but decreased of EF% versus the controls. -

Purinergic Regulation of Vascular Tone and Remodelling
Autonomic & Autacoid Pharmacology Autonomic & Autacoid Pharmacology REVIEW 2009, 29, 63–72 Purinergic regulation of vascular tone and remodelling G. Burnstock Correspondence: Autonomic Neuroscience Centre, Royal Free and University College Medical School, Rowland Hill Street, London NW3 2PF, G. Burnstock United Kingdom Summary 1 Purinergic signalling is involved both in short-term control of vascular tone and in longer- term control of cell proliferation, migration and death involved in vascular remodelling. 2 There is dual control of vascular tone by adenosine 5¢-triphosphate (ATP) released from perivascular nerves and by ATP released from endothelial cells in response to changes in blood flow (shear stress) and hypoxia. 3 Both ATP and its breakdown product, adenosine, regulate smooth muscle and endothelial cell proliferation. 4 These regulatory mechanisms are important in pathological conditions, including hyper- tension, atherosclerosis, restenosis, diabetes and vascular pain. Keywords: atherosclerosis, adenosine 5¢-triphosphate, hypertension, pain, purinergic, reste- nosis recognized as a cotransmitter in sympathetic, Introduction parasympathetic, sensory-motor and enteric nerves Purinergic signalling, i.e. adenosine 5¢-triphos- (Burnstock, 1976). There was early resistance to phate (ATP) acting as an extracellular signalling this concept (see Burnstock, 2006a,b), but the roles molecule, was proposed by Burnstock in 1972 of nucleotides and nucleosides as extracellular when evidence was presented that ATP was the signalling molecules -

Hereditary Angioedema: a Bradykinin-Mediated Swelling Disorder
368 Theme Issue Article Hereditary angioedema: a bradykinin-mediated swelling disorder Jenny Björkqvist1,2; Anna Sala-Cunill1,3,4; Thomas Renné1,2 1Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm, Sweden; 2Center of Molecular Medicine, Karolinska Institutet, Stockholm, Sweden; 3Allergy Section, Internal Medicine Department, Hospital Universitari Vall d´Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain; 4Allergy Research Unit, Allergy Department, Institut de Recerca Vall d’Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain IVBM 2012 Summary be life-threatening involving the skin, the oropharyngeal, laryngeal, Edema is tissue swelling and is a common symptom in a variety of dis- and gastrointestinal mucosa. Three different types of hereditary an- eases. Edema form due to accumulation of fluids, either through re- giodema exist in patients. The review summarises current knowledge duced drainage or increased vascular permeability. There are multiple on the pathophysiology of hereditary angiodema and focuses on re- vascular signalling pathways that regulate vessel permeability. An im- cent experimental and pharmacological findings that have led to a portant mediator that increases vascular leak is the peptide hormone better understanding and new treatments for the disease. bradykinin, which is the principal agent in the swelling disorder hered- itary angioedema. The disease is autosomal dominant inherited and Keywords presents clinically with recurrent episodes of acute swelling that can Contact -

Bradykinin-Induced Secretion of Insulin, Glucagon and Somatostatin Chi Yang Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1996 Bradykinin-induced secretion of insulin, glucagon and somatostatin Chi Yang Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Animal Sciences Commons, Pharmacology Commons, Physiology Commons, Veterinary Physiology Commons, and the Veterinary Toxicology and Pharmacology Commons Recommended Citation Yang, Chi, "Bradykinin-induced secretion of insulin, glucagon and somatostatin " (1996). Retrospective Theses and Dissertations. 11504. https://lib.dr.iastate.edu/rtd/11504 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. INFORMATION TO USERS This manuscr^t has been reproduced firom the microfihn master. UMI films the text directfy firom the original or copy submitted. Thus, some thesis and dissertation copies are in Q^writer &ce, while others may be from any type of conq)uter printer. Tlie quality of this reprodnction is dqsendent upon the quali^ of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bieedthrough, substandard Tnarginqj and in^oper alignment can adverse^ affect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyii^t material had to he removed, a note vnll indicate the deletion. Oversize materials (e.g., m^s, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand comer and continuing from1^ to right in equal sections with small overlq>s. -
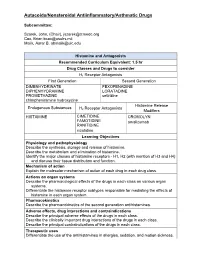
5-Autacoids FINAL
Autacoids/Nonsteroidal Antiinflammatory/Asthmatic Drugs Subcommittee: Szarek, John, (Chair), [email protected] Cox, Brian [email protected] Malik, Asrar B. [email protected] Histamine and Antagonists Recommended Curriculum Equivalent: 1.5 hr Drug Classes and Drugs to consider H1 Receptor Antagonists First Generation Second Generation DIMENHYDRINATE FEXOFENADINE DIPHENHYDRAMINE LORATADINE PROMETHAZINE cetirizine chlorpheniramine hydroxyzine Histamine Release Endogenous Substances H Receptor Antagonists 2 Modifiers HISTAMINE CIMETIDINE CROMOLYN FAMOTIDINE omalizumab RANITIDINE nizatidine Learning Objectives Physiology and pathophysiology Describe the synthesis, storage and release of histamine. Describe the metabolism and elimination of histamine. Identify the major classes of histamine receptors - H1, H2 (with mention of H3 and H4) and discuss their tissue distribution and function. Mechanism of action Explain the molecular mechanism of action of each drug in each drug class. Actions on organ systems Describe the pharmacological effects of the drugs in each class on various organ systems. Differentiate the histamine receptor subtypes responsible for mediating the effects of histamine in each organ system. Pharmacokinetics Describe the pharmacokinetics of the second generation antihistamines. Adverse effects, drug interactions and contraindications Describe the principal adverse effects of the drugs in each class. Describe the clinically important drug interactions of the drugs in each class. Describe the principal contraindications of the drugs in each class. Therapeutic uses Differentiate the use of the antihistamines in allergies, sedation, and motion sickness. Clinical Pharmacology Of the first generation antihistamines, chlorpheniramine is the least sedating and is often preferred because of this characteristic Dimenhydrinate and diphenhydramine have a relatively narrow therapeutic index and are often used recreationally as over-the-counter hallucinogens. -

Independent Mechanisms in Midazolam-Induced Vasodilation
Hypertension Research (2011) 34, 929–934 & 2011 The Japanese Society of Hypertension All rights reserved 0916-9636/11 www.nature.com/hr ORIGINAL ARTICLE Involvement of endothelium-dependent and -independent mechanisms in midazolam-induced vasodilation Gian Luca Colussi, Alessandro Di Fabio, Cristiana Catena, Alessandra Chiuch and Leonardo A Sechi Benzodiazepine (BDZ) infusion has been shown to reduce blood pressure in both humans and animals. Although the inhibitory effects of BDZ on the central nervous system have been well documented, less is known about the direct effects of BDZ on the vascular bed. The aims of this study were to assess the effects of the BDZ midazolam on the vascular system in C57/BL6 mouse aortic rings and to investigate the mechanisms of its direct vascular action. We found that midazolam induced reversible, dose-dependent vasodilation in potassium- and phenylephrine-precontracted rings. In rings that were precontracted with potassium or phenylephrine, treatment with 10 lmol lÀ1 midazolam increased vasodilation by 15 and 60%, respectively, compared with baseline. Vasodilation increased by 80 and 87%, respectively, after treatment with 50 lmol lÀ1 midazolam. Only the low concentration of midazolam (10 lmol lÀ1) induced endothelium-dependent vasodilation in phenylephrine-precontracted rings. Vasodilation increased by 60% in rings with endothelium and by 20% in rings without endothelium. Conversely, only the À1 high concentration of midazolam (50 lmol l ) reduced the CaCl2-induced vasoconstriction of aortic rings with EC50 (the concentration giving 50% of the maximal effect) values of 1 and 6 mmol lÀ1 for vehicle- and midazolam-treated rings, respectively. Furthermore, the incubation of phenylephrine-precontracted rings with an inhibitor of the nitric oxide synthase (NOS) NG-nitro-L-arginine methyl ester or the inhibitors of central or peripheral type BDZ receptors (flumazenil or PK 11195, respectively) produced no change in midazolam-induced vasodilation. -

Pharmacology
PHARMACOLOGY • Autacoids : Angiotensin, Plasma Kinins • Dr. Vandana Roy Professor Department of Pharmacology Maulana Azad Medical College & associated Hospitals New Delhi-110 002 (10-12-2007) CONTENTS Introduction Angiotensin Angiotensinogen Angiotensin Peptides Angiotensinases Kinins Kininogens Kallikreins Bradykinin Receptors Vasoactive Intestinal Peptide Neurotensin Substance P Calcitonin Gene Related Peptide Lipid Derived Autacoids : Eicosanoids Platelet Activating Factor Keywords Angiotensin, renin, angiotensin converting enzyme inhibitor, ACE, angiotensin receptor blockers, bradykinin, vasoactive intestinal peptide, neurotensin, substance P, calcitonin gene related peptide, arachidonic acid, eicosanoids, prostaglandins, prostacyclin, thromboxane, platelet activating factor, 1 Introduction Autacoids are substances of diverse nature normally present in the body or may be formed there. The word autacoid is derived from the Greek word autos (self) and akos (medical agent or remedy). Thus the word autacoids was used for substances that act within restricted, local areas near their site of synthesis, unlike hormones that are produced by specific cells and then transferred by circulation to distant sites of action. Thee substances usually have a brief lifetime. Heterogeneous substances have been included as autacoids. These are: Amine Derived Histamine 5 Hydroxytryptamine Lipid derived Prostanoids (prostaglandins, thromboxanes) Leukotrienes Platelet Derived Factor Peptide Angiotensin Kinins (Bradykinin, kallidin) Vasoactive intestinal -

The Value of Urotensin II in Patients with Left-Sided Rheumatic Valvular Regurgitation
The Egyptian Heart Journal (2016) xxx, xxx–xxx HOSTED BY Egyptian Society of Cardiology The Egyptian Heart Journal www.elsevier.com/locate/ehj www.sciencedirect.com The value of urotensin II in patients with left-sided rheumatic valvular regurgitation Ibrahim Elmadbouh a,*, Mahmoud Ali Soliman b, Ahmed Abdallah Mostafa c, Haitham Ahmed Heneish d a Biochemistry Department, Faculty of Medicine, Menoufia University, Egypt b Cardiology Department, Faculty of Medicine, Menoufia University, Egypt c Cardiology Department, Police Academy Hospital, Egypt d Cardiology Department, Nasser Institute Hospital, Egypt Received 20 May 2016; accepted 24 September 2016 KEYWORDS Abstract Aims: Rheumatic valve diseases are most common etiological valve diseases in develop- Urotensin II; ing countries. Urotensin II is cardiovascular autacoid/hormone and may be associated with patients Mitral regurgitation; of heart valve diseases. The present study was to measure plasma urotensin II concentrations in Cardiovascular autacoid patients with left-sided rheumatic valve diseases such as mitral regurgitation (MR) and aortic regur- hormone gitation (AR), and to examine its correlation with severity of valve impairment, function (New York Heart association, NYHA) class and pulmonary artery pressure (PAP). Methods and results: Sixty patients with moderate to severe rheumatic left-sided valve regurgitation and 20 healthy controls were selected after performing the echocardiography. Plasma urotensin II level was measured in all subjects. The patients with MR and AR were significantly increased of left ventricular end diastolic dimension (LVEDD), left ventricular end systolic dimension (LVESD), left atrial diameter, PAP, but decreased of EF% versus the controls. Urotensin II level was highly sig- nificant in patients with MR (1.83 ± 0.92 ng/ml, P <0.001) and AR (0.79 ± 0.3 ng/ml, P < 0.05) versus the controls (0.48 ± 0.13 ng/ml). -

Autocoids: a Brief Review
wjpmr, 2020,6(12), 369-377 SJIF Impact Factor: 5.922 WORLD JOURNAL OF PHARMACEUTICAL Review Article Awasthi et al. World Journal of Pharmaceutical and Medical Research AND MEDICAL RESEARCH ISSN 2455-3301 www.wjpmr.com WJPMR AUTOCOIDS: A BRIEF REVIEW Prof. D. K. Awasthi*1 and Gyanendra Awasthi2 1Department of Chemistry Sri J.N.M.P.G. College, Lucknow, U.P. India. 2Department of Bio-Chemistry Dolphin Institute, Dehradun U.K. India. *Corresponding Author: Prof. D. K. Awasthi Department of Chemistry Sri J.N.M.P.G. College, Lucknow, U.P. India. Article Received on 21/11/2020 Article Revised on 11/12/2020 Article Accepted on 01/12/2020 ABSTRACT Autacoids or "autocoids" are biological factors which act like local hormones, have a brief duration, and act near the site of synthesis. The word autacoid comes from the Greek "Autos" and "Acos". The effects of autacoids are mostly localized but large amounts can be produced and moved into circulation. Autacoids may thus have systemic effect by being transported via circulation. These regulating molecules are also metabolized locally. So the compounds are produced locally, they act locally and are metabolised locally. Autacoids can have many different biological actions including modulation of the activity of smooth muscles, glands, nerves, platelets and other tissues. Some other autacoids are primarily characterized by the effect they have upon different tissues, such as smooth muscle. With respect to vascular smooth muscle, there are both vasoconstrictor and vasodilator autacoids. Vasodilator autacoids can be released during periods of exercise. Their main effect is seen in the skin, allowing for heat loss.