Short-Term Effects of Salt Restriction Via Home Dishes Do Not Persist In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Editorial Board
Editorial Board Editor in Chief Susumu Kumagai University of Tokyo / FSCJ Itsuko Horiguchi FSCJ Hiroshi Satoh FSCJ Yasushi Yamazoe FSCJ Associate Editors Katsue Ishii FSCJ Shigeki Yamamoto FSCJ Midori Yoshida FSCJ Masatsune Murata FSCJ Editorial Board Yasunobu Aoki National Institute for Environmental Atsushi Ono Okayama University, Japan Studies, Japan Hiroaki Aoyama The Institute of Environmental Hiroshi Ozaki University of Tokyo, Japan Toxicology, Japan Satoshi Asano International University of Health Yoshihiro Ozeki Tokyo University of Agriculture and Welfare, Japan and Technology, Japan Ginji Endo The Ohara Memorial Institute for Junzo Saegusa Japanese Association for Science of Labour, Japan Laboratory Animal Science, Japan Yukihiro Goda National Institute of Health Sciences, Jun-ichi Sawada Pharmaceuticals and Medical Devices Japan Agency, Japan Ryuichi Hasegawa Pharmaceuticals and Medical Devices Tsutomu Sekizaki University of Tokyo, Japan Agency, Japan Akira Hiratsuka Tokyo University of Pharmacy and Makoto Shibutani Tokyo University of Agriculture Life Sciences, Japan and Technology, Japan Akihiko Hirose National Institute of Health Sciences, Makoto Shimizu Tokyo University of Agriculture, Japan Japan Masao Horimoto Chiba Institute of Science, Japan Vittorio Silano Medical School, II University of Rome, Italy Toshio Imai National Cancer Center, Japan Tomotaka Sobue Osaka University, Japan Katsumi Imaida Kagawa University, Japan Yoshiko Sugita-Konishi Azabu University, Japan Toru Kawanishi National Institute of Health Sciences, -

Azabu University
University Accreditation Results (Results for Certified Evaluation and Accreditation for university) Azabu University Basic Information of the Institution Ownership: Private Location: Kanagawa, Japan Accreditation Status Year of the Review: 2017 Accreditation Status: accredited (Accreditation Period: April.01.2018 – March.31.2025) 2 Certified Evaluation and Accreditation Results for Azabu University Overview Azabu University (hereafter, the University) began as Tokyo Veterinary Training School in 1890 and was established as Azabu Veterinary College in 1950. It was renamed Azabu University in April 1980 and is currently organized into two faculties (School of Veterinary Medicine and School of Life and Environmental Science) and two graduate schools (Graduate School of Veterinary Science and Graduate School of Environmental Health) with the campus located in Sagamihara City, Kanagawa Prefecture. After its accreditation review by Japan University Accreditation Association (JUAA) in 2010, the University formulated its “Third Mid-term Targets and Plan” (2015-2020) in 2015 with the objective to act on its founding spirit “explore academically and practice conscientiously” and has been making improvements such as clarifying the role of the faculty council and board of councilors in administration. As part of its social cooperation and social contribution activities, the University opened The Life Museum of Azabu University where it displays information about the university’s history as well as zoology, environmental studies and other fields in an easy-to-understand manner. It is also holding and expanding the “small animal clinical seminar” meant for veterinarians by leveraging the Azabu University Veterinary Teaching Hospital. This effort is commendable for strengthening relations between the community and persons related to veterinary services. -

The Sensitivity of Commercial Kits in Detecting the Genes of Pathogenic Bacteria in Venison
NOTE Public Health The sensitivity of commercial kits in detecting the genes of pathogenic bacteria in venison Akiko YAMAZAKI1)#, Mioko HONDA2)#, Naoki KOBAYASHI3,4), Naoto ISHIZAKI3), Hiroshi ASAKURA5) and Yoshiko SUGITA-KONISHI3,4)* 1)Department of Veterinary Sciences, University of Iwate, 3-18-8, Ueda, Morioka, Iwate 020-8550, Japan 2)Department of Animal Nursing Science, Yamazaki Gakuen University, 4-7-2 Minami Osawa, Hachioji, Tokyo 192-0364, Japan 3)Department of Food and Life Science, Azabu University, 1-17-71 Fuchinobe, Chuo, Sagamihara, Kanagawa 252-5201, Japan 4)Graduate School of Life and Environmental Sciences, Azabu University, 1-17-71 Fuchinobe, Chuo, Sagamihara, Kanagawa 252-5201, Japan 5)Division of Biomedical Food Research, National Institute of Health Sciences, 1-18-1 Kamiyoga, Setagaya-ku, Tokyo 158-8501, Japan J. Vet. Med. Sci. ABSTRACT. The expansion of the wild deer population is a major problem for the Japanese farm 80(4): 706–709, 2018 and forestry industries because their damage to farm products and vegetation results in huge economic loss. To promote game meat consumption, hygiene inspections should be performed doi: 10.1292/jvms.17-0530 to detect main bacterial pathogens before products are shipped. In this study, we aimed to evaluate the ability of commercial test kits to genetically detect EHEC, Salmonella and Listeria monocytogenes in venison. Our results demonstrated that the kits for three pathogens could be Received: 29 September 2017 useful for venison as well as other domestic meat products. Our comparative study showed that Accepted: 8 February 2018 the LAMP kits were more sensitive than the RT-qPCR kits in the detection of all of these pathogens. -

List of English and Native Language Names
LIST OF ENGLISH AND NATIVE LANGUAGE NAMES ALBANIA ALGERIA (continued) Name in English Native language name Name in English Native language name University of Arts Universiteti i Arteve Abdelhamid Mehri University Université Abdelhamid Mehri University of New York at Universiteti i New York-ut në of Constantine 2 Constantine 2 Tirana Tiranë Abdellah Arbaoui National Ecole nationale supérieure Aldent University Universiteti Aldent School of Hydraulic d’Hydraulique Abdellah Arbaoui Aleksandër Moisiu University Universiteti Aleksandër Moisiu i Engineering of Durres Durrësit Abderahmane Mira University Université Abderrahmane Mira de Aleksandër Xhuvani University Universiteti i Elbasanit of Béjaïa Béjaïa of Elbasan Aleksandër Xhuvani Abou Elkacem Sa^adallah Université Abou Elkacem ^ ’ Agricultural University of Universiteti Bujqësor i Tiranës University of Algiers 2 Saadallah d Alger 2 Tirana Advanced School of Commerce Ecole supérieure de Commerce Epoka University Universiteti Epoka Ahmed Ben Bella University of Université Ahmed Ben Bella ’ European University in Tirana Universiteti Europian i Tiranës Oran 1 d Oran 1 “Luigj Gurakuqi” University of Universiteti i Shkodrës ‘Luigj Ahmed Ben Yahia El Centre Universitaire Ahmed Ben Shkodra Gurakuqi’ Wancharissi University Centre Yahia El Wancharissi de of Tissemsilt Tissemsilt Tirana University of Sport Universiteti i Sporteve të Tiranës Ahmed Draya University of Université Ahmed Draïa d’Adrar University of Tirana Universiteti i Tiranës Adrar University of Vlora ‘Ismail Universiteti i Vlorës ‘Ismail -
Double Virus Vector Infection to the Prefrontal Network of the Macaque Brain
RESEARCH ARTICLE Double Virus Vector Infection to the Prefrontal Network of the Macaque Brain Mineki Oguchi1☯, Miku Okajima2☯, Shingo Tanaka1, Masashi Koizumi1, Takefumi Kikusui3, Nobutsune Ichihara3, Shigeki Kato4, Kazuto Kobayashi4, Masamichi Sakagami1* 1 Brain Science Institute, Tamagawa University, Machida, Tokyo, Japan, 2 Graduate School of Arts and Sciences, The University of Tokyo, Meguro, Tokyo, Japan, 3 School of Veterinary Medicine, Azabu University, Sagamihara, Kanagawa, Japan, 4 Department of Molecular Genetics, Institute of Biomedical Sciences, Fukushima Medical University, Fukushima, Fukushima, Japan a11111 ☯ These authors contributed equally to this work. * [email protected] Abstract To precisely understand how higher cognitive functions are implemented in the prefrontal OPEN ACCESS network of the brain, optogenetic and pharmacogenetic methods to manipulate the signal Citation: Oguchi M, Okajima M, Tanaka S, Koizumi transmission of a specific neural pathway are required. The application of these methods, M, Kikusui T, Ichihara N, et al. (2015) Double Virus however, has been mostly restricted to animals other than the primate, which is the best ani- Vector Infection to the Prefrontal Network of the mal model to investigate higher cognitive functions. In this study, we used a double viral Macaque Brain. PLoS ONE 10(7): e0132825. doi:10.1371/journal.pone.0132825 vector infection method in the prefrontal network of the macaque brain. This enabled us to express specific constructs into specific neurons that constitute a target pathway without Editor: Joseph Charles Glorioso, University of Pittsburgh School of Medicine, UNITED STATES use of germline genetic manipulation. The double-infection technique utilizes two different virus vectors in two monosynaptically connected areas. -

プログラム(英語)English Programme
Presentation Program Day 1 (Saturday, May 18 at Kyoto Seika University) Room A : L201 Room B : L101 Room C : L102 Room D : L103 Room E : L002 9:00 10:00 Registration 10:00 1 Nobuko YAMAZAKI Forum Yuji ATAKA Atsuki SHIBATA Kyoto University 'African History in Broader PersPective: Kwansei Gakuin University Graduate School of Letters, Kyoto Univ. Some Dimensions in 19th and 20th Practice of Integrated Physical Forum Conflicts and (Forced) Migration at Century' Security Measures by Local Residents in GeograPhy on SPatial Recognition of 'EXPansion of Green Grabbing' Borderland: A Case Study of West Nile Southwest Madagascar: Current Status Hunter-Gatherer in Kalahari Sub-Region in Uganda and Future ProsPects Yukino IWAI (Waseda University) Suzuki, Hideaki (National Museum of 'Contesting the Border on the Serengeti Ethnology) Teshirogi, Koki 10:15 2 Yukiko KONDO Mei NAKAZAWA Erika MIYAKE, A. TAKADA National Park in Tanzania' 'African DiasPora in the 20th Century Nihon Fukushi University Persian Gulf: Preliminary Observations CAAS, Kyoto University ASAFAS, Kyoto University Kyoko NAKAMURA (Toyo University) Memories of Violence: with Slave Narratives' Land Use and Its Influence on the 'Community Breakdown Brought by Sagawa, Sagawa, Toru PeoPle’s Affection and Imagination for Land Enclosure by High Income Class in “Community Conservancy”: A Case of Ikeno, Jun RelationshiP between San and Others’ Sufferings in Post-Genocide Anthony A. Lee (UCLA) Suburban Area in Southern Uganda Ovawambo in North-Central Namibia Kenyan Pastoral Community' Rwanda -

1. Japanese National, Public Or Private Universities
1. Japanese National, Public or Private Universities National Universities Hokkaido University Hokkaido University of Education Muroran Institute of Technology Otaru University of Commerce Obihiro University of Agriculture and Veterinary Medicine Kitami Institute of Technology Hirosaki University Iwate University Tohoku University Miyagi University of Education Akita University Yamagata University Fukushima University Ibaraki University Utsunomiya University Gunma University Saitama University Chiba University The University of Tokyo Tokyo Medical and Dental University Tokyo University of Foreign Studies Tokyo Geijutsu Daigaku (Tokyo University of the Arts) Tokyo Institute of Technology Tokyo University of Marine Science and Technology Ochanomizu University Tokyo Gakugei University Tokyo University of Agriculture and Technology The University of Electro-Communications Hitotsubashi University Yokohama National University Niigata University University of Toyama Kanazawa University University of Fukui University of Yamanashi Shinshu University Gifu University Shizuoka University Nagoya University Nagoya Institute of Technology Aichi University of Education Mie University Shiga University Kyoto University Kyoto University of Education Kyoto Institute of Technology Osaka University Osaka Kyoiku University Kobe University Nara University of Education Nara Women's University Wakayama University Tottori University Shimane University Okayama University Hiroshima University Yamaguchi University The University of Tokushima Kagawa University Ehime -
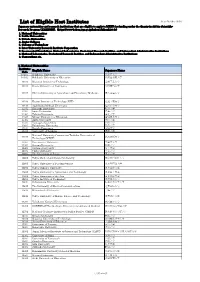
List of Eligible Host Institutes
List of Eligible Host Institutes As of October 2018 Japanese universities and research institutions that are eligible to apply to MEXT for funding under the Grants-in-Aid for Scientific- Research Program (KAKENHI ). (https://www-kaken.jsps.go.jp/kaken1/kikanList.do) 1. National Universities 2. Public Universities 3. Private Universities 4. Junior Colleges 5. Colleges of Technology 6. Inter-University Research Institute Corporation 7. Incorporated Foundations, National Laboratories, Prefectural Research Instities, and Independent Administrative Institutions 8. National Laboratories, Prefectural Research Instities, and Independent Administrative Institutions 9. Corporations etc. 1. National Universities Institutes English Name Japanese Name Code 10101 Hokkaido University 北海道大学 10102 Hokkaido University of Education 北海道教育大学 10103 Muroran Institute of Technology 室蘭工業大学 10104 Otaru University of Commerce 小樽商科大学 10105 Obihiro University of Agriculture and Veterinary Medicine 帯広畜産大学 10106 Kitami Institute of Technology (KIT) 北見工業大学 10107 Asahikawa Medical University 旭川医科大学 11101 Hirosaki University 弘前大学 11201 Iwate University 岩手大学 11301 Tohoku University 東北大学 11302 Miyagi University of Education 宮城教育大学 11401 Akita University 秋田大学 11501 Yamagata University 山形大学 11601 Fukushima University 福島大学 12101 Ibaraki University 茨城大学 12102 University of Tsukuba 筑波大学 National University Corporation Tsukuba University of 12103 筑波技術大学 Technology (NTUT) 12201 Utsunomiya University 宇都宮大学 12301 Gunma University 群馬大学 12401 Saitama University 埼玉大学 12501 Chiba University -

1 WELCOME Welcome to the 16Th Annual Meeting of the International
WELCOME Welcome to the 16th annual meeting of the International Society for Anthrozoology held in Tokyo on the 4th and 5th of October, 2007. I am honored to host the very first ISAZ meeting in Asia and hoping that many of you enjoy a new and different atmosphere at this year’s meeting in the metropolitan big city, Tokyo. The topic of this year’s meeting is ―The Power of Animals: Approaches to Identifying New Roles for Animals in Society‖. Today, people are relying on animals to serve increasingly more varied and complex roles, and these new dependencies both broaden and complicate our conception of human-animal relationships. Increased social integration, intimacy, and dependence upon animals raise unique issues that have no precedent. Despite the modern trend toward decreased contact with nature, humans and animals are still vulnerable to natural and manmade disasters and, despite incredible advances in the field of medicine, people continue to suffer from intractable diseases. Working animals are called upon to assist in disasters, diagnose disease, locate bombs and narcotics, and to help people with disabilities to lead more productive and satisfying lives. In light of the incredibly important roles played by these animals, and those yet to be discovered, better understanding of the potential abilities of animals is needed. In this conference, the changes in the role and perception of animals in society will be addressed especially through the two plenary talks on the first day. Professor Kasey Grier will talk about the importance of historical approaches to understand the modern human-animal relationships, whereas Professor Mitsuaki Ohta, the current president of the Society for the Study of Human Animal Relations in Japan will talk on his unique scientific research on animals’ ability to anticipate earthquakes. -

Higher Education in Asia: Expanding Out, Expanding Up
REPUBLIC OF KOREA China, Hong Kong MYANMAR China, Macao LAO PDR HIG HER EDUCATION STATISTICS IN ASIA: for Expanding Out, Expanding Up BRUNEI DARUSSALAM The rise of graduate education and university research INSTITUTE INSTITUTE UNESCO HIGHER EDUCATION IN ASIA: Expanding Out, Expanding Up The rise of graduate education and university research UNITED NATIONS UNIVERSITY UNU-IIST International Institute International Institute for for Educational Planning Software Technology UNESCO The constitution of the United Nations Educational, Scientific and Cultural Organization (UNESCO) was adopted by 20 countries at the London Conference in November 1945 and entered into effect on 4 November 1946. The Organization currently has 195 Member States and 9 Associate Members. The main objective of UNESCO is to contribute to peace and security in the world by promoting collaboration among nations through education, science, culture and communication in order to foster universal respect for justice, the rule of law, and human rights and fundamental freedoms that are affirmed for the peoples of the world, without distinction of race, sex, language or religion, by the Charter of the United Nations. To fulfill its mandate, UNESCO performs five principal functions: 1) prospective studies on education, science, culture and communication for tomorrow’s world; 2) the advancement, transfer and sharing of knowledge through research, training and teaching activities; 3) standard-setting actions for the preparation and adoption of internal instruments and statutory recommendations; 4) expertise through technical co-operation to Member States for their development policies and projects; and 5) the exchange of specialised information. UNESCO is headquartered in Paris, France. The UNESCO Institute for Statistics The UNESCO Institute for Statistics (UIS) is the statistical office of UNESCO and is the UN depository for global statistics in the fields of education, science and technology, culture and communication. -
Partnering Universities and Colleges List(As of January 1, 2021)
■Partnering Universities and Colleges list(As of January 1, 2021) No. Prefectures Name No. Prefectures Name No. Prefectures Name 1 Hokkaido Asahikawa Medical University 81 Fukushima Koriyama Women's University 161 Chiba Kameda College of Health Sciences 2 Hokkaido Otaru University of Commerce 82 Fukushima Higashi Nippon International University 162 Chiba Kawamura Gakuen Women's University 3 Hokkaido Obihiro University of Agriculture and Veterinary Medicine 83 Fukushima Iwaki Junior College 163 Chiba Kanda University of International Studies 4 Hokkaido Kitami Institute of Technology 84 Fukushima Koriyama Women's College 164 Chiba Keiai University 5 Hokkaido Hokkaido University of Education 85 Ibaraki Ibaraki University 165 Chiba International Budo University 6 Hokkaido Hokkaido University 86 Ibaraki Tsukuba University of Technology 166 Chiba Shumei University 7 Hokkaido Muroran Institute of Technology 87 Ibaraki University of Tsukuba 167 Chiba Shukutoku University 8 Hokkaido Sapporo Medical University 88 Ibaraki Ibaraki Prefectural University of Health Sciences 168 Chiba Josai International University 9 Hokkaido Sapporo City University 89 Ibaraki Ibaraki Christian University 169 Chiba Seitoku University 10 Hokkaido Asahikawa University 90 Ibaraki Tsukuba Gakuin University 170 Chiba Seiwa University 11 Hokkaido Sapporo Gakuin University 91 Ibaraki Tsukuba International University 171 Chiba Chiba Institute of Science 12 Hokkaido Sapporo International University 92 Ibaraki Tokiwa University 172 Chiba Chiba Keizai University 13 Hokkaido Sapporo -
Prospective Memory in Nonhuman Primates
The 74th Annual Meeting of the Japanese Society for Animal Psychology July 19th(Sat)- 21st(Mon), 2014, Inuyama Hosted by the Primate Research Institute, Kyoto University Organizing Committee Tetsuro Matsuzawa (Kyoto University), President Masaki Tomonaga (Kyoto University), Vice President Ikuma Adachi (Kyoto University), General Secretary Misato Hayashi (Kyoto University) Yuko Hattori (Kyoto University) Fumito Kawakami (Kyoto University) Makiko Uchikoshi (Kyoto University) Michiko Sakai (Kyoto University) Yoko Ohyabu (Kyoto University) Yukari Okumura (Kyoto University) Naoko Mizuno (Kyoto University) Advisory Committee Toshikazu Hasegawa (University of Tokyo) Takefumi Kikusui (Azabu University) Shigeru Kitazawa (Osaka University) Kazuo Fujita (Kyoto University) Satoshi Hirata (Kyoto University) Shoji Itakura (Kyoto University) Fumihiro Kano (Kyoto University) Tadamichi Morisaka (Tokai University) Tadatoshi Ogura (Kitazato University) Yu Mizuno (Chubu Gakuin University & Collage) Aya Saito (Chubu Gakuin University & Collage) Foreword Dear friends and colleagues, It is my very great pleasure and honor to welcome you to the 74th annual congress of the Japanese Society for Animal Psychology. Society members can feel proud to belong to such a long-established and well-regarded organization, but one still willing to embrace change. For the very first time, all presentations at this society meeting will be given in English. This is also the first congress to be hosted by Kyoto University Primate Research Institute (KUPRI). Given the extra challenge and effort required for non-native speakers to present in English, we are delighted and encouraged to have received such a large number of high quality applicants. Over the three-day conference schedule we are proud to offer over 100 presentations (plenary, oral and poster presentations) covering a huge variety of fascinating topics.