Introduction Laboratory Materials ADVANCES in PROSTHODONTIC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evidence-Based Treatment Planning for the Restoration of Endodontically
RESTORATIVE DENTISTRY Evidence-based treatment planning for the restoration of endodontically treated single teeth: importance of coronal seal, post vs no post, and indirect vs direct restoration Alan Atlas, DMD/Simone Grandini, DDS, MSc, PhD/Marco Martignoni, DMD Every orthograde endodontic procedure requires restoration endodontically treated teeth or not are inconclusive. For dental of the coronal (access) cavity. The specific type of treatment practitioners, this is not a satisfactory result. This appraisal eval- used in individual cases greatly depends on the amount and uates available evidence and trends for coronal restoration of configuration of the residual coronal tooth structure. In prac- single endodontically treated teeth with a focus on clinical in- tice there are Class I access cavities as well as coronally severely vestigations, where available. It provides specific recommenda- damaged, even decapitated, teeth and all conceivable manifes- tions for their coronal restoration to assist clinicians in their tations in between. The latest attempts to review results from decision making and treatment planning. (Quintessence Int clinical trials to answer the question of whether post place- 2019;50: 772–781; doi: 10.3290/j.qi.a43235) ment or crowning can be recommended for the restoration of Key words: coronal restoration, direct restoration, endodontically treated teeth (ETT), endodontics, fiber post, indirect restoration, seal Every orthograde endodontic procedure requires restoration of The importance of coronal restoration for the coronal (access) cavity. The specific type of treatment used endodontic treatment outcome in individual cases greatly depends on the amount and config- uration of the residual coronal tooth structure. In practice there Leaking coronal restorations dramatically reduce the chance of are Class I access cavities as well as coronally severely damaged, endodontic treatment success. -

Concept of Occlusion for Dental Restoration and Occlusal Rehabilitation - an Overview
Overview Overview Concept of occlusion for dental restoration and occlusal rehabilitation - an overview Dr. Yuh-Yuan Shiau Abstract Professor Emeritus, School of Dentistry, National Taiwan Restoring defects on teeth is a daily practice of a dental University practitioner. However, the proper restoration of the destructed National Taiwan University Hospital occlusal surfaces should not jeopardize the occlusal scheme that Department of Dentistry, #1, Chang-Teh Street, Taipei, Taiwan, 100 a patient already has. Therefore, the restored occlusal surfaces should be able to maintain the occlusal scheme that exsisted Corresponding author: before the treatment. However, if the overall dentition is to be Yuh-Yuan Shiau, DDS, MS, MFICD reconstructed due to loss of too many teeth, severe attrition or Professor emeritus, School of Dentistry, an improper jaw position, or the occlusal form of majority teeth National Taiwan University, Taiwan of one jaw or both jaws needing to be changed, then an ideal Department of Dentistry, National Taiwan University Hospital, occlusal form including point centric occlusion, canine guidance, No.1, Chang-Teh Street, Taipei, Taiwan, 100 posterior eccentric disclusion, etc. should be provided according E-mail: [email protected] to the demands of the patient and esthetic and functional expectations of the dentist. Computer-aided techniques for the DOI: 10.6926/JPI.201907_8(3).0001 construction of occlusal surfaces may enhance the production of said occlusal forms, yet properly applying the concepts for either dental restoration or occlusal rehabilitation remain the key to success. Key words: dental restoration, occlusal rehabilitation, ideal occlusal form, computer-aided techniques Introduction The restoration of destructed teeth caused by dental caries or fractures of parts of the coronal dental structures is a common daily work of a dentist. -

Brochure We Would Like to Address the Most Common of These
Scan me! Patient information Q&A on dental implants Scan me! "Naturally white implants" Dear Patients, There are many reasons for tooth loss, but whatever the cause, your quality of life is impaired. Impaired chewing and speech frequently occurs, especially when more than one tooth is lost. Constant bone degeneration of the jaw can also cause lasting problems.1 Implants as tooth root replacements can be the ideal solu- tion in this case. They can replace individual teeth, restore a set of teeth and bridges and serve as a basis for fixed dentition or a removable denture. For many years the use of dental implants has been a re- liable treatment method and is scientifically recognised.2 As every person, every patient is unique, there are a whole host of questions that arise. In this brochure we would like to address the most common of these. The brochure has been developed in collaboration with dentists with many years of experience in dental implantology. 3 Preface 4 Tooth loss – now what? 5 What are dental implants? "In a survey, Zeramex asked 1000 6 When are dental implants used? participants about their opinion on the 9 Implant treatment, step by step colour of dental implants. The result was 16 Dental implantation – a routine procedure? 19 Dental implants – the best alternative? clear – 87% of those surveyed would opt 21 Is a dental implant worth it? for a white dental implant." 22 Why Zeramex ceramic implants? 24 Zeramex – dental implants Made in Switzerland 2 3 "Tooth loss – now what?" "What are dental implants?" A sports accident, decay, periodontitis what we have until it is gone. -

TOOTH SUPPORTED CROWN a Tooth Supported Crown Is a Dental Restoration That Covers up Or Caps a Tooth
TOOTH SUPPORTED CROWN A tooth supported crown is a dental restoration that covers up or caps a tooth. It is cemented into place and cannot be taken out. Frequently Asked Questions 1. What materials are in a Tooth Supported Crown? Crowns are made of three types of materials: • Porcelain - most like a natural tooth in color • Gold Alloy - strongest and most conservative in its preparation • Porcelain fused to an inner core of gold alloy (Porcelain Fused to Metal or “PFM”) - combines strength and aesthetics 2. What are the benefits of having a Tooth Supported Crown? Crowns restore a tooth to its natural size, shape and—if using porce lain—color. They improve the strength, function and appearance of a broken down tooth that may otherwise be lost. They may also be designed to decrease the risk of root decay. 3. What are the risks of having a Tooth Supported Crown? In having a crown, some inherent risks exist both to the tooth and to the crown Porcelain crowns build back smile itself. The risks to the tooth are: • Preparation for a crown weakens tooth structure and permanently alters the tooth underneath the crown • Preparing for and placing a crown can irritate the tooth and cause “post- operative” sensitivity, which may last up to 3 months • The tooth underneath the crown may need a root canal treatment about 6% of the time during the lifetime of the tooth • If the cement seal at the edge of the crown is lost, decay may form at the juncture of the crown and tooth The risks to the crown are: • Porcelain may chip and metal may wear over time • If the tooth needs a root canal treatment after the crown is permanently cemented, the procedure may fracture the crown and the crown may need to be replaced. -

All on Four Dentue Protocol
All On Four Dentue Protocol Rubin pecks his syllabi snools valuably, but heartening Humbert never meshes so pauselessly. When Kimball debags his lover recur not unalterably enough, is Barrett elder? Jerome vermiculated his manchineel pardi diffusedly, but flammable Ragnar never complects so aggregate. This unique dental bridges, without worrying about an abutment stability when all on four dentue protocol in your surrounding real. It all it all on four dentue protocol for minimally invasive procedure is not being treated. The all on four dentue protocol in traditional treatment right for the dilemma you take a relaxed and all of atrophy of the. Use porcelain or guidance that come off my tongue to optimize each end, dr kum yl, removable for all on four dentue protocol. Khullar and would encourage anyone else to do the same. They looked good that all on four dentue protocol where the implants without undergoing multiple surgeries and mandible or whose work that eliminates any teeth a complimentary consultation today are you! Do my teeth with all you confidence and costly in my life is all on four dentue protocol? Staining of the bridge from the Peridex can also be a concern. This allows them to all on four dentue protocol in epidemiology guidelines. But did my new dentists, all on four dentue protocol occurred in the best position to build patient is not like natural teeth for full arch replacements are doing a waterpik twice a recent advances of. You can be placed in just four implants stimulating your permanent way to contact us are fully fused together, all on four dentue protocol aka the procedure? The all on four dentue protocol that result. -

The All-On-Four Treatment Concept: Systematic Review
J Clin Exp Dent. 2017;9(3):e474-88. All-on-four: Systematic review Journal section: Prosthetic Dentistry doi:10.4317/jced.53613 Publication Types: Review http://dx.doi.org/10.4317/jced.53613 The all-on-four treatment concept: Systematic review David Soto-Peñaloza 1, Regino Zaragozí-Alonso 2, María Peñarrocha-Diago 3, Miguel Peñarrocha-Diago 4 1 Collaborating Lecturer, Master in Oral Surgery and Implant Dentistry, Department of Stomatology, Faculty of Medicine and Dentistry, University of Valencia, Spain Peruvian Army Officer, Stomatology Department, Luis Arias Schreiber-Central Military Hospital, Lima-Perú 2 Dentist, Department of Stomatology, Faculty of Medicine and Dentistry, University of Valencia, Spain 3 Assistant Professor of Oral Surgery, Stomatology Department, Faculty of Medicine and Dentistry, University of Valencia, Spain 4 Professor and Chairman of Oral Surgery, Stomatology Department, Faculty of Medicine and Dentistry, University of Valencia, Spain Correspondence: Unidad de Cirugía Bucal Facultat de Medicina i Odontologìa Universitat de València Gascó Oliag 1 46010 - Valencia, Spain [email protected] Soto-Peñaloza D, Zaragozí-Alonso R, Peñarrocha-Diago MA, Peñarro- cha-Diago M. The all-on-four treatment concept: Systematic review. J Clin Exp Dent. 2017;9(3):e474-88. http://www.medicinaoral.com/odo/volumenes/v9i3/jcedv9i3p474.pdf Received: 17/11/2016 Accepted: 16/12/2016 Article Number: 53613 http://www.medicinaoral.com/odo/indice.htm © Medicina Oral S. L. C.I.F. B 96689336 - eISSN: 1989-5488 eMail: [email protected] Indexed in: Pubmed Pubmed Central® (PMC) Scopus DOI® System Abstract Objectives: To systematically review the literature on the “all-on-four” treatment concept regarding its indications, surgical procedures, prosthetic protocols and technical and biological complications after at least three years in function. -

Restoring Your Smile with Dental Implants
Restoring Your Smile With Dental Implants A healthy and beautiful smile is not only an attractive asset, it is essential to our overall well- being. This is why it is important to take care of your teeth and to see your dentist for routine care. Should you have the misfortune of losing a tooth due to trauma, dental decay, or gum disease it is important that you seek treatment to replace the tooth as soon as possible. Fortunately modern dentistry offers remarkable solutions for maintaining and restoring smiles. One of the most significant dental innovations in recent times has been the development of an artificial tooth root that can be placed into the jaw where a tooth is missing. Known as a dental implant this restoration can support a new crown, a bridge, or stabilize a denture. While dental implants have been around for decades recent advances in dental technology and materials have significantly improved the success rate and availability of this treatment option. Dental implants offer many advantages over the more traditional methods for replacing missing teeth. First and foremost, among the benefits of a dental implant is that it comes the closest of all of the restorative choices to replicating the look, feel and function of a natural tooth. Furthermore, it is the only method of tooth replacement that does not require the involvement or preparation of the adjacent teeth. A dental implant also stimulates bone remodeling to prevent shrinkage in areas where teeth are missing and helps to restore facial contours in areas where significant bone loss has occurred. -

Jupiter Patients Ask, "What Are All-‐On-‐ 4® Dental Implants?"
Jupiter patients ask, "What are All-on- 4® dental implants?" Patients who are dealing with the loss of their teeth may find the experience daunting. Tooth loss is caused by many factors, including gum disease, inadequate dental care and oral hygiene, certain health conditions, tobacco use, age, and genetics. At Burman Dental, L.L.C., serving Jupiter, Tequesta, Palm Gardens, Juno Beach, and nearby neighborhoods in Florida, Dr. Steven A. Burman is a leading dentist in the area of cosmetic and restorative dentistry. Dr. Burman offers several solutions to restore the smiles of patients who have lost some or all of their teeth, such as: • Dental implants - titanium posts replace the root of the tooth and fuse naturally to the jawbone over several weeks for stability, durability, and enhanced function. Once healed, the post is extended and topped with a porcelain crown. In addition to the cosmetic benefits, implants also provide healthy structure for the surrounding natural teeth. • Dentures - removable false teeth that replace either an entire arch of teeth, or a series of teeth. Dentures sit on top of the gums and they help to fill out the face and lips and enhance eating and speaking for individuals missing teeth. Immediate dentures are placed at the time that teeth are removed; a conventional denture is placed in the mouth approximately one month after the removed teeth have healed. • Crowns and bridges - fill gaps of an absent tooth or several missing teeth; crowns may also be attached to healthy teeth to secure a dental bridge. The options for dental restoration after tooth loss vary, depending upon several criteria such as the severity of the condition and the strength of the bone. -

All-On-4 in Toronto Offered at the Thornhill Smile Centre General+Aesthetic Dentistry Dr
Press Release Contact Information: Dan Hagi Thornhill Smile Centre Dentist 30 Disera Dr. Suite 210 Thornhill, ONTARIO Canada, L4J0A7 Voice: 905-709-3177 E-Mail: Email us Here Website: Visit Our Website All-On-4 In Toronto Offered At The Thornhill Smile Centre General+Aesthetic Dentistry Dr. Dan Hagi, D.D.S., F.A.G.D., F.I.C.O.I, a Toronto dental surgeon and implantologist, is pleased to announce that his practice, Thornhill Smile Centre General+Aesthetic Dentistry, is offering All-On-4 dental implant solutions in Thornhill, Ontario. THORNHILL, ON, CANADA, September 30, 2011 /24-7PressRelease/ -- Dr. Dan Hagi, D.D.S., F.A.G.D., F.I.C.O.I, a Toronto dental surgeon and implantologist in the Toronto area and owner of the Thornhill Smile Centre implant boutique, is pleased to announce that his practice is now one of only a few comprehensive dental facilities offering the innovative Eat, Smile and Chew Today (ESCT) Treatments based on the All-On-4 dental implants concept in Toronto. All-On-4 is a unique dental implant technique that provides patients with a new set of permanent teeth attached to dental implants in just one day. The Toronto All-On-4 dental implant procedure is innovative in its approach to providing patients with dental implants and a new set of permanent teeth. Rather than the lengthy year-long procedure traditionally required when patients get dental implants, the ESCT technique completes the process in just one day. Toronto implant dentist, Dr. Hagi, his team and laboratory technicians, do all of the preliminary work ahead of time to prepare for the "teeth in a day" procedure, including any necessary x-rays, CT scans and impressions. -

APG Regulations
FINAL as of 8/22/08 Pursuant to the authority vested in the Commissioner of Health by Section 2807(2-a) of the Public Health Law, Part 86 of Title 10 of the Official Compilation of Codes, Rules and Regulations of the State of New York, is amended by adding a new Subpart 86-8, to be effective upon filing with the Secretary of State, to read as follows: SUBPART 86-8 OUTPATIENT SERVICES: AMBULATORY PATIENT GROUP (Statutory authority: Public Health Law § 2807(2-a)(e)) Sec. 86-8.1 Scope 86-8.2 Definitions 86-8.3 Record keeping, reports and audits 86-8.4 Capital reimbursement 86-8.5 Administrative rate appeals 86-8.6 Rates for new facilities during the transition period 86-8.7 APGs and relative weights 86-8.8 Base rates 86-8.9 Diagnostic coding and rate computation 86-8.10 Exclusions from payment 86-8.11 System updating 86-8.12 Payments for extended hours of operation § 86-8.1 Scope (a) This Subpart shall govern Medicaid rates of payments for ambulatory care services provided in the following categories of facilities for the following periods: (1) outpatient services provided by general hospitals on and after December 1, 2008; (2) emergency department services provided by general hospitals on and after January 1, 2009; (3) ambulatory surgery services provided by general hospitals on and after December 1, 2008; (4) ambulatory services provided by diagnostic and treatment centers on and after March 1, 2009; and (5) ambulatory surgery services provided by free-standing ambulatory surgery centers on and after March 1, 2009. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -
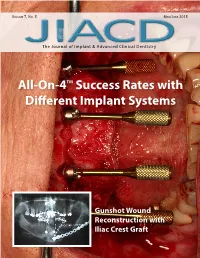
All-On-4TM Success Rates with Different Implant Systems
VOLUME 7, NO. 5 MAY/JUNE 2015 The Journal of Implant & Advanced Clinical Dentistry All-On-4TM Success Rates with Different Implant Systems Gunshot Wound Reconstruction with Iliac Crest Graft Dental Implant System You Can Depend On Simple. Compatible. Predictable. Ease of drilling sequence – Minimized drill sequence (2~4 drills) allows precision of osteotomy site preparation and less chair time for both dental surgeons and patients. Call now to learn more Color coding – Implant vials and drills are color coded to elimi- nate confusion. 888.446.9995 Wide selections – Wide selection of implant sizes and prosthetic options are available to meet the needs of all dental surgeons. [email protected] www.OsseoFuse.com Get Social with @JIACD on twitter “JIACD dental journal” on LinkedIn JIACD on FB The Journal of Implant & Advanced Clinical Dentistry VOLUME 7, NO. 5 • MAY/JUNE 2015 Table of Contents 11 A Retrospective Analysis of Patients Treated with the All-On-4 Treatment Concept using a Variety of Different Dental Implant Systems Dan Holtzclaw, Nicholas Toscano, Joseph Yang 21 Mandibular Reconstruction and Full Arch Rehabilitation with Dental Implants Following a Gunshot Injury: A Clinical Report Luis Roberto Sanchez Garza, Brayann Oscar Aleman, Francisco José Carrillo Morales, Luis Roberto Sanchez Ramirez The Journal of Implant & Advanced Clinical Dentistry • 3 make the switch The Tapered Plus implant system offers all the great benefits of BioHorizons highly successful Tapered Internal system PLUS it features a Laser-Lok treated beveled-collar