Women's Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GIPE-010316-Contents.Pdf
THE INTERNATIONAL LIDRARY OF SEXOLOGY AND PSYCHOLOGY Edited by' NoRMAN HAIRE, Ch.M., M.B. THE CASE F.OR STERII.JSATION TID! INTERNA110NAL LIBRA.llY OF SEXOLOGY AND PSYOIOLOGY Edited by NoiUWI Hm..s,. Cll.M., M.B. v.,.r-u p.biisw,. ;, pr,p;.liotl MAN AND WoMAN JN M.uuw.Ga. By C. B. S. Evans. M.D. THB Coii:PANIONATB M.uuw.Ga. By Judge Ben Lindsey. THB R.iwoLT oP MoDI!B.N YoUTH. By Judge Ben Lindsey. Su LrFB AND SBX ETHICS. By Reo4! Guyon. • SBXUAL .ABER.8.ATIONS (a vols.). By Wilhelm Srekcl. · THB CHOICB OP A MATL By Anthony M. Ludovid. THB PoWBa m Lova. By Edwin W. H.incb. M.D. Su JN HUMAN Rlu..ATIONSHIPS. By Dr. Magnus Hirschfeld THE CASE FOR STERILISATION by LEON F. WlllTNEY Dhectot oE the American Eugenics Society Wfth a.n Introduction a.nd Notes by NORMAN HAIRE, Ch.M., M.B. and two diagrams LONDON JOHN LANE THE BODLEY HEAD 111.1.11& .tJ1D I'IWiftD D GIIL\'1 IIIUTADI BY 'I'OIIIIIIIDGII nlllftU II.D. I'ILLCB BALL WOIIJal 'I'OIIBIUDGII DJIT EDITOR'S INTRODUCTION The menace of the u.a.fit is not a new problem, nor confined to any one country. It is age-old and world wide. At some periods, and in some places, it is solved by the crude method of infanticide-the destrug:ion of the child after birth. This solution being out of con sonance with our ethical views, we have to consider whether we are to accept as inevitable the burden which has to be shouldered by the rest of Society if unpro ductive, and often actively anti-social, individuals are permitted to be born without Society making any _attempt at all to check their numbers, or whether, on the other hand, we are to make some attempt to check them. -

Finding Aid Template
RARE BOOKS & SPECIAL COLLECTIONS University Library GUIDE TO THE NORMAN HAIRE COLLECTION DESCRIPTIVE SUMMARY Reference id: Manuscript collection. Norman Haire collection. Title: Norman Haire collection Date: Bulk 1926-1950 Creator: Haire, Norman, 1892-1952 Language Represented: English Repository: Rare Books and Special Collections, University of Sydney Library Extent: 8 boxes Genres and Forms: Material including manuscripts; typescript; press clippings; photographs; correspondence; documents; films; glass negatives; x-rays; related publications. Abstract: The Norman Haire collection chiefly consists of the writings of Norman Haire. Much of this material is in typescript. Correspondence between Haire and other sexologists such as Magnus Hirschfeld and Havlock Ellis are also held. Other material includes press clippings of items of interest to Haire. ADMINISTRATIVE INFORMATION Provenance Norman Haire bequeathed his papers and collection to the University of Sydney, Rare Books and Special Collections library. Access The Rare Books and Special Collections Library is a closed access collection. Readers may not browse the shelves. To use material from the collection go to the Rare Books Office and fill out a request slip for each item you require. Staff will collect the material for you which you must read under supervision in the Rare Books Reading Room. You must provide identification (for example, University of Sydney library card, drivers licence) while you are using the material. Biographical note Norman Haire was a medical practitioner and sexologist. He studied medicine at the University of Sydney (M.B., Ch.M. 1915). He was a prolific author and active educator. Haire was a prominent reformer and researcher in Britain during the 1930s. -

228 Paddington: a History
228 Paddington: A history Paddington_Chapter9_Final.indd 228 23/9/18 2:37 pm Chapter 9 Creative Paddington Peter McNeil 22 9 229 Paddington_Chapter9_Final.indd 229 23/9/18 2:37 pm Margaret Olley, one of Australia’s favourite artists, The creatives of Paddington today are more likely died in July 2011. She had become synonymous to run an art space, architecture or design firm, with the suburb of Paddington. As if to celebrate engage in public relations and media, trade her art and personal energy, her estate left the commodities, or be retired doctors or lawyers. downstairs lights of her home blazing, revealing the In the Paddington–Moore Park area today, nearly bright walls as well as her own artworks, including 20 per cent of employees work in legal and rooms she made famous by including them as financial services.3 subjects. Olley loved the suburb of Paddington. But why have so many culturally influential She could paint, garden and, entertain there from people lived in Paddington? Located conveniently her large corner terrace in Duxford Street. She close to the central business district which could liked the art crowd as well as the young people be reached by bus, tram and later the train link working in shops and the working-class people at Edgecliff station, its mixture of terraced who still lived there. She recalled that, as art houses, small factories, workshops and students at the old Darlinghurst Gaol in the early warehouses, provided cultural producers – 1940s, ‘Paddington beckoned … we knew there was whether they be artists or advertising executives something across beyond the Cutler Footway, but – a range of multi-functional spaces and initially we dared not go there’.1 Within a generation interpersonal networks. -

Sexuality: an Australian Historian's Perspective
Sexuality: An Australian Historian’s Perspective Frank Bongiorno Suppression N 2004 A CONTROVERSY ERUPTED WHEN IT CAME TO LIGHT THAT THE AUSTRALIAN education minister, Brendan Nelson, had vetoed several projects Irecommended for funding by the Australian Research Council (ARC). The provocation for Nelson’s action on behalf of the conservative government to which he belonged was an article published in a tabloid newspaper by right-wing columnist Andrew Bolt, criticising the ARC for supporting ‘peek-in-your-pants researchers fixated on gender or race’ (Bolt, ‘Grants to Grumble’). Bolt’s campaign against the ARC continued for several years, as did Nelson’s vetting of research proposals. Among the columnist’s targets were a project on ‘the cultural history of the body in modern Japan’, and another on ‘attitudes towards sexuality in Judaism and Christianity in the Hellenistic Greco-Roman era’ (Bolt, ‘Paid to be Pointless’; Macintyre). The identity of the researchers and projects that Nelson had actually rejected remained a secret but university researchers, guided by Bolt’s fixation with projects about sex, took for granted that these were prominent among those culled. One researcher later commented that applicants were omitting the words ‘sexuality’, ‘class’ and ‘race’ from proposals in an effort to avoid the minister’s wrath (Alexander). The episode raised many questions—including about academic freedom—but was of particular interest to researchers of sexuality. Why did such projects lend Bongiorno, Frank. ‘Sexuality: An Australian Historian’s -
Introduction: Issues of Definition and Evidence
Notes Introduction: Issues of Definition and Evidence 1. Buckridge, “Kind of Exile,” 111. 2. Blackmur, Lion and the Honeycomb, 61. 3. Wolfreys, Writing London, 10. Other books on this subject are John Clement Ball’s Imagining London (2004); Alan Robinson’s Imagining London, 1770–1900 (2004); and John McLeod’s Postcolonial London: Rewriting the Metropolis (2004). Collections of edited essays include David Feldman and Gareth Stedman Jones’s Metropolis London (1989); Susana Onega and John Stotesbury’s London in Literature (2002); Pamela Gilbert’s Imagined Londons (2002); and Lawrence Phillips’s The Swarming Streets (2004). In 1999, the journal of postcoloniality, Kunapipi, devoted an entire issue to readings of the city. Despite the quantity, however, virtually none of this most recent work is by Australians, or touches on representations of London by Australians. 4. Porter, “Anglo-Australian Watershed,” 187. Italics added. Porter himself twice attempted suicide early in his expatriation. 5. Arnold, “Australian Books,” 10.9, 10.14. See his table 10.1 and Appendix. 6. Miller, Australian Literature: A Bibliography . Extended to 1950 . by Frederick T. Macartney. It claims to include all authors who were “connected with Australia . irrespective of whether or not they . continue to reside here” (vi). Arnold was unable to use the major reference work of which he is joint editor (Arnold & Hay, eds., Bibliography of Australian Literature) because at the time of writing it was incomplete. 7. Hornung has an entry in ADB but Roberts and Farjeon do not. Hornung, Farjeon, and Roberts all have entries in ODNB, where, not surprisingly, they are treated as exclusively English authors. -

How to Find Treasure Troves ALMS Conference, Amsterdam, August 1-3, 2012
Thirty Years of Collecting Our History – Or: How to Find Treasure Troves ALMS Conference, Amsterdam, August 1-3, 2012 Ralf Dose, Magnus Hirschfeld Society, Berlin When founded in 1982/83, the Magnus Hirschfeld Society’s aim was to preserve the heritage of the sexual scientist Magnus Hirschfeld (1868-1935) for posterity, and to do research on his work. At that time, this was connected with the aim of the GL(BT) movement, which was to claim a history of its own. When looking more closely into the matter of the work and achievements of Dr. Hirschfeld, we soon noticed that the focus on GL(BT) history was far too narrow to capture the importance of Hirschfeld both for sexual science and for cultural history. 1 My paper explores some of the steps we took in finding the material remnants of Hirschfeld’s cultural heritage over some thirty years of research and collecting. It should be read together with the corresponding paper by Don McLeod on “Serendipity and the Papers of Magnus Hirschfeld: The Case of Ernst Maass,” where he gives a lot of detail about one of our joint searches. And, please, keep in mind that my English is not as good as my German. Thus, the German version of this paper sometimes is more specific than this one. 2 Preface When we started to look for Hirschfeld’s heritage, it was a common belief that hardly anything of Hirschfeld’s personal belongings or items from his Institute for Sexual Science would have survived. Manfred Herzer compiled a preliminary short list of single Hirschfeld letters which survived in various archives, libraries, and private collections. -
The Arc Erotica Collection Cambridge University Library
The ARC erotica collection of Cambridge University Library This short-title catalogue comprises a full inventory of the erotica held by Cambridge University Library in their ‘Arc’ - short for ‘Arcana’, meaning mysteries or secrets - collection as of February 2015. I first became aware of the extent of this collection and some of its treasures in the early 1980s when, together with my friend Peter Mendes, we both visited the library for the purpose of conducting some research for books we were writing. Peter’s interests were limited, by the nature of his project, to English erotica of the 19th century, but I had broader scope and rummaged around in the printed catalogue for entries by the ‘usual suspects’. I quickly found an edition of Restif de la Bretonne’s outstandingly obscene l’Anti-Justine dated 1798. To my certain knowledge, only four copies of this rara avis were in existence, all in the Bibliothèque Nationale, Paris, although rumours of a fifth copy surfaced from time-to-time. I suspected strongly that the Cambridge edition was a later reprint, falsely pre-dated as is often the custom with pornographers, and yet I was sufficiently curious to put in a request for it. To my very great surprise, and that of my companion, the book, when it arrived, turned out to be the legendary fifth copy, in a fantastic mid-19th century binding and decorative box that suggested that one of its previous owners may probably have been Frederick Hankey, the English sadist-bibliophile resident in Paris who so disturbed the Goncourt brothers when they dropped in on him. -

~FSHS Distinguished Fortians 18.02.2020 NEW.Rev.Ed MASTER
DISTINGUISHED FORTIANS 20 Name, Achievements Occupation Notes, Sources (see also notes at end) Abbott, Edwin CBE Public servant 1878-1947 • Comptroller General of Customs 1933-1944; CBE 1933 Fortian 1893 Entered NSW Customs Dept. 1893 aged 15 • Chief Inspector in the Federal Public Service Trove.nla.nla.news-article, E Abbott …30 Oct 2016 • Chief Surveyor Central Office Melbourne 1924; then Canberra 1927 Jnr.1893, NSW Jnr Snr Public Exams 1867-1916 online Honours/awards/Edwin Abbott …1 Feb 2019 Fort Street Centenary Book, 1949, p.78 Ada, Gordon Leslie AO, DSc University academic 1922-2012 • Emeritus Professor of Microbiology, John Curtin school of Medical Microbiologist Fortian 1939 Research ANU BSc 1944, MSc 1946, DSc 1961 (all USyd); FAA USyd alumni sidneienses/search • An important contributor to the World Health Organisation 1971-91 Anu.edu.au/news, Prof. Gordon Ada…23 Nov 2016 • Elected a Fellow of the Australian Academy of Science 1964; served as Honours/awards/Gordon L Ada …1 Feb 2019 its Foreign Secretary 1977-81 LC 1939 results • AO for service to medicine in the field of immunology and international health 1993 Adams, Beverlee Jill Louisa (Saul) AM Teacher Fortian 1948 Environment Parks (pdf.p.49)...14 Jul 2017 • Farmer NSW winner of ABC Rural Woman of the Year Award 1995 Honours/awards/Beverlee Adams …1 Feb 2019 • Local Council Member LC 1948 results SMH online; Fortian, 1997, p.6 • Member of Rural Women’s Network, State Advisory Committee • AM for services to local government, the community, conservation 2001 Adams, William Duncan “Bill” BA, BD, D.Min Minister of religion Fortian 1947 • Minister of the Wesley Central Mission, Brisbane BA USyd 1954; BD Melb; D.Min San Francisco; Theol. -
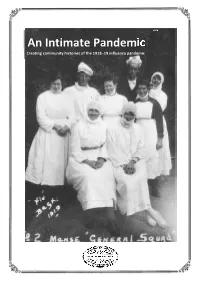
An Intimate Pandemic Creating Community Histories of the 1918–19 Influenza Pandemic
An Intimate Pandemic Creating community histories of the 1918–19 influenza pandemic Page 1 An Intimate Pandemic Creating community histories of the 1918–19 influenza pandemic The year 2019 marks the centenary of the arrival of the pneumonic influenza pandemic – often known as the ‘Spanish flu’ – on Australian shores. This guide has been prepared by the Royal Australian Historical Society to assist and encourage local history and family history groups, plus local studies librarians and public historians, to investigate this significant historical moment. Coming at the end of World War I, the pandemic infected approximately a third of Australia’s population through 1919, causing up to 15,000 deaths. The disease touched almost every community, causing illness, disruption and bereavement, but also led to profound moments of charity, courage and community spirit. This guide does not provide a history of the pandemic in Australia. Rather, it has been created to assist you in delving into local, state and national collections to prepare your own projects to commemorate the centenary. It suggests archival documents that can be drawn upon and sites to consider visiting in building a fuller picture of the local impact of the 1919 crisis. An extensive annotated bibliography of period, historical and medical accounts of the pandemic is also provided at the end of the document. The following guides to researching and writing history are recommended as starting points: Ann Curthoys and Ann McGrath. How to Write History That People Want to Read (Sydney: UNSW Press, 2009). Rosalie Triolo, Helen Doyle, and Katya Johanson. Writing and Publishing Local History: a Guide for First‐Time Authors and Historical Societies (Melbourne: Royal Historical Society of Victoria, 2017). -

Sex, Politics and Society THEMES in BRITISH SOCIAL HISTORY Edited by John Stevenson
Sex, Politics and Society THEMES IN BRITISH SOCIAL HISTORY Edited by John Stevenson Newspapers and English Society 1695–1855 Hannah Barker The English Family 1450–1700 R. Houlbrooke The Professions in Early Modern England, 1450–1800: Servants of the Commonwealth Rosemary O’Day Women’s Agency in Early Modern Britain and the American Colonies Rosemary O’Day Popular Cultures in England 1550–1750 Barry Reay Crime in Early Modern England 1550–1750 (Second Edition) J. A. Sharpe Gender in English Society 1650–1850: The Emergence of Separate Spheres? Robert B. Shoemaker Literature and Society in Eighteenth-Century England: Ideology, Politics and Culture, 1680–1820 W. A. Speck Crime and Society in England 1750–1900 (Fourth Edition) Clive Emsley Popular Disturbances in England 1700–1832 (Second Edition) John Stevenson The English Town, 1680–1840: Government, Society and Culture Rosemary Sweet Sex, Politics and Society The regulation of sexuality since 1800 THIRD EDITION Jeffrey Weeks First published 1981 by Pearson Education Limited Second edition 1989 Third edition 2012 Published 2014 by Routledge 2 Park Square, Milton Park, Abingdon, Oxon OX14 4RN 711 Third Avenue, New York, NY 10017, USA Routledge is an imprint of the Taylor & Francis Group, an informa business Copyright © 1981, 1989, 2012, Taylor & Francis. The right of Jeffrey Weeks to be identified as author of this work has been asserted by him in accordance with the Copyright, Designs and Patents Act 1988. All rights reserved. No part of this book may be reprinted or reproduced or utilised in any form or by any electronic, mechanical, or other means, now known or hereafter invented, including photocopying and recording, or in any information storage or retrieval system, without permission in writing from the publishers. -

Striving for National Fitness
STRIVING FOR NATIONAL FITNESS EUGENICS IN AUSTRALIA 1910s TO 1930s Diana H Wyndham A thesis submitted in fulfilment of the requirement for the degree of Doctor of Philosophy Department of History University of Sydney July 1996 Abstract Striving For National Fitness: Eugenics in Australia, 1910s to 1930s Eugenics movements developed early this century in more than 20 countries, including Australia. However, for many years the vast literature on eugenics focused almost exclusively on the history of eugenics in Britain and America. While some aspects of eugenics in Australia are now being documented, the history of this movement largely remained to be written. Australians experienced both fears and hopes at the time of Federation in 1901. Some feared that the white population was declining and degenerating but they also hoped to create a new utopian society which would outstrip the achievements, and avoid the poverty and industrial unrest, of Britain and America. Some responded to these mixed emotions by combining notions of efficiency and progress with eugenic ideas about maximising the growth of a white population and filling the 'empty spaces'. It was hoped that by taking these actions Australia would avoid 'racial suicide' or Asian invasion and would improve national fitness, thus avoiding 'racial decay' and starting to create a 'paradise of physical perfection'. This thesis considers the impact of eugenics in Australia by examining three related propositions: • that from the 1910s to the 1930s, eugenic ideas in Australia were readily accepted because of concerns about the declining birth rate • that, while mainly derivative, Australian eugenics had several distinctly Australian qualities • that eugenics has a legacy in many disciplines, particularly family planning and public health This examination of Australian eugenics is primarily from the perspective of the people, publications and organisations which contributed to this movement in the first half of this century. -

The Temporality of Modernist Life Writing in the Era of Transsexualism
Loyola University Chicago Loyola eCommons English: Faculty Publications and Other Works Faculty Publications Fall 2013 The Temporality of Modernist Life Writing in the Era of Transsexualism Pamela L. Caughie Loyola University Chicago, [email protected] Follow this and additional works at: https://ecommons.luc.edu/english_facpubs Part of the English Language and Literature Commons Recommended Citation Caughie, P. "The Temporality of Modernist Life Writing in the Era of Transsexualism." Modern Fiction Studies 59(3), 2013. This Article is brought to you for free and open access by the Faculty Publications at Loyola eCommons. It has been accepted for inclusion in English: Faculty Publications and Other Works by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. © Purdue Research Foundation by the Johns Hopkins University Press, 2013. Caughie 501 THE TEMPORALITY OF MODERNIST LIFE WRITING IN f THE ERA OF TRANSSEXUALISM: VIRGINIA WOOLF'S ORLANDO AND EINAR WEGENER'S MAN INTO WOMAN Pamela L. Caughie Consider what immense forces society brings to play upon each of us, how that society changes from decade to decade . ; well, if we cannot analyse these invisible presences, we know very little of the subject of the memoir; and again how futile life writing becomes. —Virginia Woolf, "A Sketch of the Past" In a conversation with Bruno Latour, historian and philosopher of science Michel Serres provides a metaphor that captures modernist life writing's temporality. Our experience of time, says Serres, re- sembles a crumpled handkerchief rather than a flat plane, where the past folds in on the present, pressing on it at difference places, and the present folds in on the past, pressing on it from behind in that the present redacts our understanding of what the past has become (60).1 Virginia Woolf shares this understanding of the proximity of MFS Modern Fiction Studies, Volume 59, number 3, Fall 2013.