Thoracic Abnormal Air Collections in Patients in the Intensive Care Unit
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Trauma-Associated Pulmonary Laceration in Dogs—A Cross Sectional Study of 364 Dogs
veterinary sciences Article Trauma-Associated Pulmonary Laceration in Dogs—A Cross Sectional Study of 364 Dogs Giovanna Bertolini 1,* , Chiara Briola 1, Luca Angeloni 1, Arianna Costa 1, Paola Rocchi 2 and Marco Caldin 3 1 Diagnostic and Interventional Radiology Division, San Marco Veterinary Clinic and Laboratory, via dell’Industria 3, 35030 Veggiano, Padova, Italy; [email protected] (C.B.); [email protected] (L.A.); [email protected] (A.C.) 2 Intensive Care Unit, San Marco Veterinary Clinic and Laboratory, via dell’Industria 3, 35030 Veggiano, Padova, Italy; [email protected] 3 Clinical Pathology Division, San Marco Veterinary Clinic and Laboratory, via dell’Industria 3, 35030 Veggiano, Padova, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-0498561098 Received: 5 March 2020; Accepted: 8 April 2020; Published: 12 April 2020 Abstract: In this study, we describe the computed tomography (CT) features of pulmonary laceration in a study population, which included 364 client-owned dogs that underwent CT examination for thoracic trauma, and compared the characteristics and outcomes of dogs with and without CT evidence of pulmonary laceration. Lung laceration occurred in 46/364 dogs with thoracic trauma (prevalence 12.6%). Dogs with lung laceration were significantly younger than dogs in the control group (median 42 months (interquartile range (IQR) 52.3) and 62 months (IQR 86.1), respectively; p = 0.02). Dogs with lung laceration were significantly heavier than dogs without laceration (median 20.8 kg (IQR 23.3) and median 8.7 kg (IQR 12.4 kg), respectively p < 0.0001). When comparing groups of dogs with thoracic trauma with and without lung laceration, the frequency of high-energy motor vehicle accident trauma was more elevated in dogs with lung laceration than in the control group. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

The Supine Pneumothorax
Annals of the Royal College of Surgeons of England (1987) vol. 69 The supine pneumothorax DAVID A P COOKE FRCS Surgical Registrar, Department ofSurgery, St Thomas' Hospital JULIE C COOKE FRCR* Radiological Senior Registrar, Department ofDiagnostic Radiology, Brompton Hospital, London Key words: PNEUMOTHORAX; COMPUTI ED TOMOGRAPHY; TRAUMA Summary TABLE I Causes of a pneumothorax The consequences of an undiagnosed pneumothorax can be life- threatening, particularly in patients with trauma to the head or Broncho-pulmonay pathology Traumatic injuy and in those mechanical ventilation. Yet multiple requiring Asthma it is these patients, whose films will be assessed initially by the Bronchial adenoma surgeon, who are more likely to have a chest X-ray taken in the Bronchial carcinoma Penetrating trauma supine position. The features of supine pneumothoraces are de- Emphysema Blunt trauma scribed and discussed together with radiological techniques used to Fibrosing alveolitis Inhaled foreign body confirm the diagnosis, including computed tomography (CT) Idiopathic which may be ofparticular importance in patients with associated Marfan's syndrome fatrogenic cranial trauma. Pulmonary abscess Pulmonary dysplasia CVP line insertion Introduction Pulmonary infarct Jet ventilation Pulmonary metastases Liver biopsy In a seriously ill patient or the victim of multiple trauma Pulmonoalveolar proteinosis Lung biopsy the clinical symptoms and signs of a pneumothorax may Radiation pneumonitis Oesophageal instrumentation be overshadowed by other problems. Usually in these Sarcoid PEEP ventilation circumstances a chest X-ray will be taken at the bedside Staphylococcal septicaemia Pleural aspiration with the patient supine and the appearances of a Tuberculosis Pleural biopsy pneumothorax will be different from those seen when the Tuberose sclerosis patient is upright. -

CHEST RADIOLOGY: Goals and Objectives
Harlem Hospital Center Department of Radiology Residency Training Program CHEST RADIOLOGY: Goals and Objectives ROTATION 1 (Radiology Years 1): Resident responsibilities: • ED chest CTs • Inpatient and outpatient plain films including the portable intensive care unit radiographs • Consultations with referring clinicians MEDICAL KNOWLEDGE: • Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognitive sciences and the application of this knowledge to patient care. At the end of the rotation, the resident should be able to: • Identify normal radiographic and CT anatomy of the chest • Identify and describe common variants of normal, including aging changes. • Demonstrate a basic knowledge of radiographic interpretation of atelectasis, pulmonary infection, congestive heart failure, pleural effusion and common neoplastic diseases of the chest • Identify the common radiologic manifestation of thoracic trauma, including widened mediastinum, signs of aortic laceration, pulmonary contusion/laceration, esophageal and diaphragmatic rupture. • Know the expected postoperative appearance in patients s/p thoracic surgery and the expected location of the life support and monitoring devices on chest radiographs of critically ill patients (intensive care radiology); be able to recognize malpositioned devices. • Identify cardiac enlargement and know the radiographic appearance of the dilated right vs. left atria and right vs. left ventricles, and pulmonary vascular congestion • Recognize common life-threatening -

Deep Sulcus Sign Developed in Patient with Multiple Fibrous Bands Between the Parietal and Visceral Pleura
eISSN: 2508-8033 Brief Image in Trauma pISSN: 2508-5298 Deep Sulcus Sign Developed in Patient with Multiple Fibrous Bands between the Parietal and Visceral Pleura Chan Yong Park1, Kwang Hee Yeo1, Sung Jin Park1, Ho Hyun Kim1, Chan Kyu Lee1, Seon Hee Kim1, Hyun Min Cho1, Seok Ran Yeom2 1Department of Trauma Surgery, Pusan National University Hospital, Busan, Korea 2Department of Emergency Medicine, Pusan National University Hospital, Busan, Korea A deepening of the costophrenic angle occurs in cases with a deep sulcus sign. We report a case of deep sulcus sign in a 47-year-old man who fell from the fifth floor. Supine chest radiography showed a right-sided pneumothorax with deep sulcus sign. Chest computed tomography (CT) demonstrated a large pneumothorax with multiple fibrous bands between the parietal and visceral pleura of the upper lobe of the right lung. (Trauma Image Proced 2017(1):7-9) Key Words: Pneumothorax; X-Rays; Diagnosis; Tomography, X-Ray computed CASE A 47-year-old man presented to the emergency department after falling from a fifth floor height. His vital signs were systolic blood pressure 60 mmHg, pulse rate 111 beats/min, respiration rate 31 breaths/min, body temperature, 36.4℃, and oxygen saturation 96%. The injury severity score was 29, revised trauma score 5.15, trauma and injury severity score 74.8%. His arterial blood gas analysis was pH 7.35, pCO2 29 mmHg, pO2 75 mmHg, hemoglobin 16.7, SaO2 94%, lactic acid 11.8 mmol/L, and base excess -8.0. Supine chest radiography showed a right-sided pneumothorax with a deep sulcus Fig. -

Large Traumatic Pneumatocele in a 2-Year-Old Child
Hindawi Publishing Corporation Case Reports in Pediatrics Volume 2013, Article ID 940189, 3 pages http://dx.doi.org/10.1155/2013/940189 Case Report Large Traumatic Pneumatocele in a 2-Year-Old Child N. K. Cheung,1 A. James,2 and R. Kumar3 1 Department of Surgery, John Hunter Hospital, New Lambton Heights, Newcastle, NSW 2305, Australia 2 Department of Cardiothoracic Surgery, John Hunter Hospital, New Lambton Heights, Newcastle, NSW 2305, Australia 3 Department of Paediatric Surgery, John Hunter Children’s Hospital, New Lambton Heights, Newcastle, NSW 2305, Australia Correspondence should be addressed to R. Kumar; [email protected] Received 3 August 2013; Accepted 22 August 2013 Academic Editors: Y. Z. Bai, S. Burjonrappa, S. G. Golombek, and Z. Jiang Copyright © 2013 N. K. Cheung et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Traumatic pneumatoceles are a rare complication of blunt chest trauma in children. Although they characteristically present as small, regular shaped lesions which can be safely treated nonoperatively, larger traumatic pneumatoceles pose diagnostic and management difficulties for clinicians. This case study reports one of the largest traumatic pneumatoceles reported to datein the paediatric population, which resulted in aggressive surgical intervention for both diagnostic and treatment reasons. This case adds further evidence to the current literature that significantly large traumatic pneumatoceles with failure of initial conservative management warrant surgical exploration and management to optimise recovery and prevent complications. 1. Introduction 2. Case Presentation Traumatic pneumatocele (TP) is a rare condition occurring A 2-year-old boy presented to the emergency department after blunt chest trauma in children and young adults, after being knocked over and his left shoulder and chest accounting for 3.9% of paediatric blunt chest traumas. -

A Case of Congenital Bronchial Defect Resulting in Massive Posterior Pneumomediastinum : First Case Report
대 한 주 산 회 지 제26권 제3호, 2015 � Case Report � Korean J Perinatol Vol.26, No.3, Sep., 2015 http://dx.doi.org/10.14734/kjp.2015.26.3.255 A Case of Congenital Bronchial Defect Resulting in Massive Posterior Pneumomediastinum : First Case Report Ji Eun Jeong, M.D.1, Chi Hoon Bae, M.D.2, and Woo Taek Kim, M.D.1 Department of pediatrics1, Department of Thoracic and Cardiovascular Surgery2, Catholic university of Daegu School of Medicine, Daegu, Korea Bronchial defects in neonates are known to occur very rarely as a complication of mechanical ventilation or intubation. This causes persistent air leakage that may form massive pneumomediastinum or pneumothorax, leading to cardiac tamponade or cardiorespiratory deterioration. Early diagnosis and treatment of bronchial defects are essential, as they can be accompanied by underlying severe lung parenchymal diseases, especially in preterm infants. We encountered an extremely low birth weight infant with an air cyst cavity in the posterior mediastinum that displaced the heart anteriorly, thereby causing cardiopulmonary deterioration. During exploratory-thoracotomy, after division of the air cyst wall (mediastinal pleura), we found a small bronchial defect in the posterior side of the right main bronchus. The patient had shown respiratory distress syndrome at birth, and she was managed by constant low positive pressure ventilation using a T-piece resuscitator after gentle intubation. As the peak inspiratory pressure was maintained low throughout and because intubation was successful at the first attempt without any difficulty, we think that the cause of the defect was not barotrauma or airway injury during intubation. -

Diagnosis of Pneumothorax in Critically Ill Adults Postgrad Med J: First Published As 10.1136/Pmj.76.897.399 on 1 July 2000
Postgrad Med J 2000;76:399–404 399 Diagnosis of pneumothorax in critically ill adults Postgrad Med J: first published as 10.1136/pmj.76.897.399 on 1 July 2000. Downloaded from James J Rankine, Antony N Thomas, Dorothee Fluechter Abstract The diagnosis of pneumothorax is estab- Box 1: Mechanisms of air entry lished from the patients’ history, physical causing pneumothorax examination and, where possible, by ra- x Chest wall damage: diological investigations. Adult respira- Trauma and surgery tory distress syndrome, pneumonia, and trauma are important predictors of pneu- x Lung surface damage: mothorax, as are various practical proce- Trauma—for example, rib fractures dures including mechanical ventilation, Iatrogenic—for example, attempted central line insertion, and surgical proce- central line insertion dures in the thorax, head, and neck and Rupture of lung cysts abdomen. Examination should include an inspection of the ventilator observations x Alveolar air leak: and chest drainage systems as well as the Barotrauma patient’s cardiovascular and respiratory Blast injury systems. x Via diaphragmatic foramina from Radiological diagnosis is normally con- peritoneal and retroperitoneal structures fined to plain frontal radiographs in the critically ill patient, although lateral im- x Via the head and neck ages and computed tomography are also important. Situations are described where an abnormal lucency or an apparent lung will then recoil away from the chest wall and a edge may be confused with a pneumotho- pneumothorax will be produced.1 rax. These may arise from outside the Air can enter the pleural space in a variety of thoracic cavity or from lung abnormali- diVerent ways that are summarised in box 1. -

Signs in Chest Imaging
Diagn Interv Radiol 2011; 17:18–29 CHEST IMAGING © Turkish Society of Radiology 2011 PICTORIAL ESSAY Signs in chest imaging Oktay Algın, Gökhan Gökalp, Uğur Topal ABSTRACT adiological practice includes classification of illnesses with similar A radiological sign can sometimes resemble a particular object characteristics through recognizable signs. Knowledge of and abil- or pattern and is often highly suggestive of a group of similar pathologies. Awareness of such similarities can shorten the dif- R ity to recognize these signs can aid the physician in shortening ferential diagnosis list. Many such signs have been described the differential diagnosis list and deciding on the ultimate diagnosis for for X-ray and computed tomography (CT) images. In this ar- ticle, we present the most frequently encountered plain film a patient. In this report, 23 important and frequently seen radiological and CT signs in chest imaging. These signs include for plain signs are presented and described using chest X-rays, computed tomog- films the air bronchogram sign, silhouette sign, deep sulcus raphy (CT) images, illustrations and photographs. sign, Continuous diaphragm sign, air crescent (“meniscus”) sign, Golden S sign, cervicothoracic sign, Luftsichel sign, scim- itar sign, doughnut sign, Hampton hump sign, Westermark Plain films sign, and juxtaphrenic peak sign, and for CT the gloved finger Air bronchogram sign sign, CT halo sign, signet ring sign, comet tail sign, CT an- giogram sign, crazy paving pattern, tree-in-bud sign, feeding Bronchi, which are not normally seen, become visible as a result of vessel sign, split pleura sign, and reversed halo sign. opacification of the lung parenchyma. -

Imaging of Thoracic Injuries 2.6
Chapter Imaging of Thoracic Injuries 2.6 G. Gavelli, G. Napoli, P.Bertaccini, G. Battista, R. Fattori Contents Since the chest X ray is essential in providing informa- tion regarding life-threatening conditions, such as tension 2.6.1 Introduction . 155 pneumothorax, hemothorax, flail chest, and mediastinal 2.6.2 Clinical and Imaging Findings . 156 abnormalities, the radiologist must have deep knowledge 2.6.2.1 Chest Wall Injuries . 156 of the possibilities and limits of this modality, which may 2.6.2.2 Parenchymal Lung Injuries . 159 not point out, or may underestimate, all these conditions. 2.6.2.3 Extra-alveolar Air . 162 2.6.2.4 Pleural Effusion and Hemothorax . 163 Poor-quality radiographs are, therefore, not acceptable 2.6.2.5 Tracheobronchial Injury . 164 especially when it becomes difficult or impossible to ex- 2.6.2.6 Thoracic Esophageal Disruption . 165 clude life-threatening conditions and an alternative imag- 2.6.2.7 Diaphragmatic Injury . 166 ing study should be performed. 2.6.2.8 Blunt Cardiac and Pericardial Injury . 169 2.6.2.9 Traumatic Aortic Injury . 169 In selected cases, it could be very useful to perform an additional lateral radiograph with horizontal incidence of 2.6.3 Conclusion . 175 the ray because the evaluation of pleural effusion, pneu- mothorax, and the identification of sternal fractures may References . 176 be easier. As mentioned previously, a CT study must be per- formed in all chest trauma patients in whom there is even the smallest diagnostic doubt on plain film. 2.6.1 Introduction Computed tomography has come to assume an increas- ingly important role in the evaluation of patients with Traumatic injuries are the fourth cause of death in the known or suspected chest injuries. -
High Yield Points
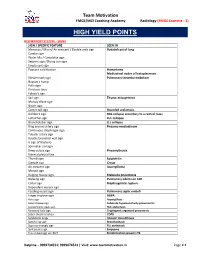
Team Motivation FMGE/MCI Coaching Academy Radiology (FMGE Essentia - 3) HIGH YIELD POINTS RESPIRATORY SYSTEM – SIGNS SIGN / SPECIFIC FEATURE SEEN IN Meniscus / Moon/ Air crescent / Double arch sign Hydatid cyst of lung Cumbo sign Water lilly / Camalotte sign Serpent sign / Rising sun sign Empty cyst sign Popcorn calcification Hamartoma Mediastinal nodes of histoplasmosis Westermark sign Pulmonary thrombo-embolism Hapton’s hump Palla sign Fleishner lines Felson’s sign Sail sign Thymic enlargement Mulvay Wave sign Notch sign Comet tail sign Rounded atelectasis Golden S sign RUL collapse secondary to a central mass Luftsichel sign LUL collapse Broncholobar sign LLL collapse Ring around artery sign Pneumo-mediastinum Continuous diaphragm sign Tubular artery sign Double bronchial wall sign V sign of Naclerio Spinnaker sail sign Deep sulcus sign Pneumothorax Visceral pleural line Thumb sign Epiglottitis Steeple sign Croup Air crescent sign Aspergilloma Monod sign Bulging fissure sign Klebsiella pneumonia Batwing sign Pulmonary edema on CXR Collar sign Diaphragmatic rupture Dependant viscera sign Feeding vessel sign Pulmonary septic emboli Finger in glove sign ABPA Halo sign Aspergillosis Head cheese sign Subacute hypersensitivity pneumonitis Juxtaphrenic peak sign RUL atelectasis Reversed halo sign Cryptogenic organized pneumonia Saber sheath trachea COPD Sandstorm lungs Alveolar microlithiasis Signet ring sign Bronchiectasis Superior triangle sign RLL atelectasis Split pleura sign Empyema Tree in bud sign on HRCT Endobronchial spread in TB -

Download Poster Abstracts
Poster # 1 Failure to Rescue and the Weekend Effect: A Study of a Statewide Trauma System Catherine E. Sharoky MD, Morgan M. Sellers MD, Elinore J. Kaufman MD, MSHP, Yanlan Huang MS, Wei Yang Ph.D., Rachel R. Kelz MD, MSCE, Patrick M. Reilly* MD, Daniel N. Holena* MD, MSCE University of Pennsylvania Introduction: Differential patient outcomes based on weekday or weekend patient presentation (i.e. the “weekend effect”) have been reported for several disease states. Failure to rescue (FTR, the probability of death after a complication) has been used to evaluate trauma care. We sought to determine whether the weekend effect impacts FTR across a mature statewide trauma system. Methods: We examined all 30 Level I and II trauma centers using the Pennsylvania Trauma Outcomes Study (PTOS) from 2007-2015. Patients age >16y with a minimum Abbreviated Injury Score 2 were included; burn patients and transfers were excluded. Our primary exposure was first major complication timing (weekday vs weekend), FTR was the primary outcome. We used multivariable logistic regression to examine the association between weekend complication occurrence and mortality. Results: Of 178,602 patients, 15,304 had a major complication [median age 58 (IQR 37-77) years, 68% male, 89% blunt injury mechanism, median injury severity score (ISS) 19 (IQR 10-29)]. Patient characteristics by complication timing were clinically similar (Table). Major complications were more likely on weekdays than weekends (9.3% vs 7.1%, p<0.001). Pulmonary and cardiac complications were most common in both groups (Table). Death occurred in 2,495 of 15,304 patients with complications, for an overall FTR rate of 16.3%.