2008 Health Eletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brief Industrial Profile of PURNEA District
P a g e | 1 G o v e r n m e n t o f I n d i a M in is t r y of M S M E Brief Industrial Profile of PURNEA District Carried out by MS ME - D e v e l opme nt I ns ti tute , M uz a ff a r pur (Ministry of MSME, Govt. of India,) Phone :-0621-2284425 Fax: 0621-2282486 e-mail:[email protected] Web- www.msmedimzfpur.bih.nic.in Page | 2 Contents S. No. Topic Page No. 1. General Characteristics of the District 3 1.1 Location & Geographical Area 4 1.2 Topography 5-6 1.3 Availability of Minerals. 7 1.4 Forest 8 1.5 Administrative set up 8-9 2. District at a glance 9-14 2.1 Existing Status of Industrial Area in the District Purnia 14 3. Industrial Scenario Of Purnia 15 3.1 Industry at a Glance - 3.2 Year Wise Trend Of Units Registered 16 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The 17 District 3.4 Large Scale Industries / Public Sector undertakings 18 3.5 Major Exportable Item 18 3.6 Growth Trend 18 3.7 Vendorisation / Ancillarisation of the Industry 18 3.8 Medium Scale Enterprises 18 3.8.1 List of the units in –PURNEA ---- & near by Area 18 3.8.2 Major Exportable Item 18 3.9.1 Coaching Industry 19 3.9.2 Potentials areas for service industry 19 3.10 Potential for new MSMEs 19 4. -

Socio- Economic Status of the Farmers in Islampur Block,Uttar Dinajpur District,West Bengal
International Journal of Research in Social Sciences Vol. 8 Issue 5, May 2018, ISSN: 2249-2496 Impact Factor: 7.081 Journal Homepage: http://www.ijmra.us, Email: [email protected] Double-Blind Peer Reviewed Refereed Open Access International Journal - Included in the International Serial Directories Indexed & Listed at: Ulrich's Periodicals Directory ©, U.S.A., Open J-Gage as well as in Cabell’s Directories of Publishing Opportunities, U.S.A SOCIO- ECONOMIC STATUS OF THE FARMERS IN ISLAMPUR BLOCK,UTTAR DINAJPUR DISTRICT,WEST BENGAL Subrata Ghosh* Abstract The way of life as well as socio-economic condition of the marginal farmers are different in many ways from civilized and technologically advanced society. Marginal farmers of the study area usually depend on subsistence agriculture. In this Keywords: regard an attempt has been made in this paper to understand socio-economic condition, the socio-economic condition of marginal farmers. The marginal farmer, subsistence present paper is purely based on primary data collected from agriculture, dependent the study area. The study area has 101 villages out of which 5 villages are selected for survey of 30 families for stratified random sampling. It has been observed that most of the peoples of the study area are highly dependent on agricultural activities. It is also noticed that these peoples are socio- economically backward. There need a number of measures to the overall socio economic development of the farmers. * Research Scholar, Department of Geography and Applied Geography, University of North Bengal, Raja Rammohunpur, Darjeeling, West Bengal 570 International Journal of Research in Social Sciences http://www.ijmra.us, Email: [email protected] ISSN: 2249-2496 Impact Factor: 7.081 Introduction : Socioeconomic status (SES) is an economic and sociological combined total measure of a person's work experience and of an individual's or family's economic and social position in relation to others, based on income, education and occupation. -

Town Survey Report Forbesganj, Series-4, Bihar
CENSUS OF INDIA 1981 SERIES-4 BIHAR Part-X B TOWN SURVEY REPORT FORBESGANJ Draft by: Edited by: Supervised by ~. P. N. SINHA S. C. SAXENA V.K.BHARGAVA Assistant Director Deputy Director Deputy Director of Census Operations, Bihar of Census Operations, Bihar of Census Operations, Bihar CONTENTS Page Foreword ... (v) Preface (vii) Chapter I Introduction 1-5 Chapter II History of growth of the town 7-8 Chapter III Amenities and services-History of growth and present position 9-17 Chapter IV Economic life of the town 19-42 Chapter V Ethnic and selected socio-demographic characteristics of the population 43-63 Chapter VI Migration and settlement of families 64-75 Chapter VII Neighbourhood pattern 76-86 Chapter VIII Family life in the town 87-93 Chapter IX Housing and materia I culture 95-102 Chapter X Organisation of power and prestige 103-106 Chapter XI Leisure and recreation, social participation, social awareness, religion and crime. 107-112 Chapter XII Linkage and Continua 113-126 Chapter XIII Conclusion 127-128 Map & Charts Showing Urban Land use Showing Pre-urban area Showing Public utility services FORBESGANJ TOWN URBAN LAND USE (NOT TO SCALE) N i BOUNDARY> TOWN WNlD ROAD Rs ,., RAILWAY .. BUSINESS A~EA re-.-el I!.!..!.!I ADMINISTAATIVE AREA ~ RESIDENTIAL AREA • EDUCATIONAL AREA ~ INDUSTRIAL AREA D AGRICULTURAL AREA D UNCLASSIFIED AREA I REGISTRY OFFICE VETERINARY 2 POST OfFICE POLICE STATION 1 HOSPITAL 6 INSPECTION BUNGALOW ~ GRAVE YARD FORBESGANJ TOWN PERI· URBAN AREA Furlongs 8 4 (0 1 Miles t:::t;:!:~~~=::::::l Km, I o 1 Kms. / \ \ ,.1 __ ._ ........ -
Purnea Introduction
DISTRICT PROFILE PURNEA INTRODUCTION Purnea district is one of the thirty-eight administrative districts of Bihar state. Purnea district is a part of Purnea division. Purnea is bounded by the districts of Araria, Katihar, Bhagalpur, Kishanganj, Madhepura and Saharsa and district of West Dinajpur of West Bengal. The major rivers flowing through Purnea are Kosi, Mahananda, Suwara Kali, Koli and Panar. Purnea district extends northwards from river Ganges. Purnia has seen three districts partitioned off from its territory: Katihar in 1976, and Araria and Kishanganj in 1990. Purnea with its highest rainfall in Bihar and its moderate climate has earned the soubriquet of 'Poor's man's Darjeeling’. HISTORICAL BACKGROUND Purnea has a rich history and a glorious past. It is believed that the name Purnea originates either from the Goddess Puran Devi (Kali) or from Purain meaning Lotus. The earliest inhabitants of Purnea were Anas and Pundras. In the epics, the Anas are grouped with the Bengal tribes and were the eastern most tribes known to the Aryans during the period of Atharva Samhita while the Pundras, although they had Aryan blood were regarded as degraded class of people in the Aitarya Brahmana, Mahabharata and Manu Samhita, because they neglected the performance of sacred rites. According to the legend of Mahabharata, Biratnagar which gave shelter to the five Pandava brothers during their one year incognito exile, is said to be located in Purnea. During the Mughal rule, Purnea was a military frontier province under the command of a Faujdar. The revenue from this outlying province was spent on the maintenance of troops for protecting the borders against tribes from the north and east. -

District Election Plan
Election Related Details Purnia 1 Geographical Indicators.. Area :- 3229 Sq Km. Longitude :- 86*-59’-06’’ ~ 87*-52’-35’’ E Latitude :- 25*-13’-80’’ ~ 27*-07’-59’’ N Soil :- Loamy soil of alluvial formation. Rivers :- Koshi, Mahananda, Suwarna kali & koli. Agriculture Products :- Jute and Banana. Population :- 3264619 (Census 2011) Projected Population :- 3909988 (2019) SC Population :- 312088 ST Population :- 111,947 Sex Ratio :- 921 (As per Census 2011) Literacy Male :- 45.63% Female :- 23.42% Total :- 35.10% Rural Area :- 2800.10 sq.kms Urban Area :- 400.21 sq.kms Railway Station :- Purnia Junction. Nearest Airport :- Bagdogra (West Bengal), Chunapur Air Force Station, Purnia. District Border :- North – Araria & Kishanganj, South – Katihar & Bhagalpur, East :- Uttar Dinajpur (W.B), West :- Madhepura Gram Panchayat :- 246 Revenue Village :- 1296 Police Station :- 27 CD Block :- 14 Sub division :- 04 2 AAddmmiinniissttrraattiivvee UUnniittss Sub division Block Purnia East, Krityanand Nagar, Kasba, Jalalgarh, Sadar Purnia Srinagar, Baisi Baisi, Dagarua, Amour, Baisa Banmankhi Banmankhi Dhamdaha Dhamdaha, Barhara Kothi, Bhawanipur, Rupauli Parliamentry Constituency Segments 58- AC Kasba 59- AC Banmankhi (SC) 60- AC Rupauli 61- AC Dhamdaha 62- AC Purnia 69- Korha (Katihar) Assembly Constituency Segments 56- AC Amour 57- AC Baisi 58- AC Kasba 59- AC Banmankhi (SC) 60- AC Rupauli 61- AC Dhamdaha 62- AC Purnia 3 Assembly Constituency Information AC no. and Total no. of Polling Sl. No Sub division Block name Station 1 2 3 4 5 Amour 1 56-Amour -

Transformation of the Rural Society of North Bengal Especially in Malda and West Dinajpur
INTRODUCTION Topographically, India may be divided into four well-marked parts1- i) The Himalayan ii) The Indo-Gangetic plain iii) The Deccan Table land iv) The Coastal plains. North Bengal is related with the Himalayan and Indo-Gangetic plain and Darjeeling district is under the Himalayan region. Northern part of Jalpaiguri and Coocbehar district were under the Himalayan region, while Malda, West Dinajpur and southern part of Jalpaiguri i.e. Duars belongs to Indo-Gangetic plain. North Bengal bears distinct features in the socio-economic structure of the geo-political atlas of India. The oldest reference of the name „Malda‟ is found in an inscription at the tomb of Pir Sahagada dated August 4, 1455 during the reign of Nasir-ud-din Muhammad Shah.2 Malda is the southernmost of the northern Bengal districts. It came under the British administration with the acquisition of Diwani by the East India Company in 1765. The district of Malda did not exist as a separate entity at that time, because Malda got the official recognition as a district in the year 1813. It should be noted that in 1816, four police stations of Purnia, two police stations of Dinajpur and three police stations of Rajshahi were added to form the Malda district which was under the supervision of a Joint Magistrate 3 (order of Governor, 25 April, 1815). At the time of its formation, the district was placed under the charge of a Joint Magistrate and Deputy Collector (Mr. Braddon).4 In 1832, for the first time, a treasury was established in Englishbazar and from that very year the separate entity of the district of Malda was recognized. -

Bihar: What Went Wrong? and What Changed? Arnab Mukherji
Bihar: What Went Wrong? And What Changed? Arnab Mukherji and Anjan Mukherji Working Paper No. 2012-107 September 2012 National Institute of Public Finance and Policy New Delhi http://www.nipfp.org.in 1 DRAFT Bihar: What went wrong? And what changed? Arnab Mukherji1 and Anjan Mukherji2,3 Economy in Historical Perspective Bihar as a political entity, either as a kingdom, or as a state within the republic of India, has its own identity from the time written records were available (Thapar 1966; Rangarajan 1992). Noted historian, Romila Thapar, describes the history of ancient India as the history of ancient Bihar. Many achievements that India became renowned for, in education, governance, society, or religion, have their roots in Bihar. Significant achievements of Bihar in trade and economic engagement within the state and outside of the Indian sub-continent emerge from a past that appears to have left no living legacy in today’s Bihar--a past so alien as to be either simply forgotten or treated as being completely incredible.4 A more recognizable, if rather dramatic picture of Bihar is that seen in a 2010 article on change in the state: 1Assistant Professor, Center for Public Policy, Indian Institute of Management Bangalore. 2Jawaharlal Nehru National Fellow, National Institute of Public Finance and Policy, New Delhi, and Country Director, IGC India-Bihar Program. 3Acknowledgements: Presented at the National Institute of Public Finance and Policy-Columbia University conference on “Growth, Poverty and Human Development in Indian States: Selected Issues” on August 7-8 at the India International Centre, New Delhi. We are indebted to our discussants Satya Das and Arunish Chawla for very helpful comments. -

Presentations on District and Agencies' Profile
Presentation on Review & Consultation Workshop from (6 Jan to 7 Jan, 2016) for Multi-Hazard District Disaster Management Plan By: Poorvanchal Gramin Vikas Sansthan (PGVS) B1/19 Vineet Khand, Gomti Nagar, Lucknow Uttar Pradesh-226010 Target districts of Purnia division Rivers Flowing from Nepal to Bihar PGVS team for coordination and Facilitation at top to down level Kumari Usha Ram Kishor Seven River Zones Zone iv iv) Kosi-Mahananda Zone consisting of Madhepura, Araria, Purnia, Kishanganj and Katihar districts. 1- Salient Points Covered in Inception Report and issues presented during Inception Workshop Sr. Points covered Purnea Araria Kishanganj Katihar No. 1. Hazards Mapping 1.1 Flood with rivers details 2. Social Vulnerabilities 2.1 Human losses 2.2 Total affected population in Lakh 11.28 3. Economical Vulnerabilities 3.1 Details of flood affected agriculture land 3.2 Livestock losses 4. Physical Vulnerabilities 4.1 House damage details 4.2 Details of sensitive places of the embankment 4.3 Total Flood affected G P 110 54 132 4.4 Total Flood affected Revenue 402 108 164 497 villages Continue--- Sr. Points covered Purnea Araria Kishanganj Katihar No. 5. Capacities 5.1 List of trained person on 40 80 10 (Police LS&R Person – LS&R) 5.2 Trained Motorboat drivers 36 20 10 10 5.3 Trained Swimmers 35 10 36 5.4 Tent 734 200 5.5 List of trained home guard 40 10 who are involved in security work 5.6 List of identified helipad 10 44 5.7 Communication plan 5.8 Details of Relief distribution places 5.9 List of Functional rain fall monitoring stations 5.10 List of Identified safe and 165 51 raised places 5.11 Details of flood post 32 Continue--- Sr. -
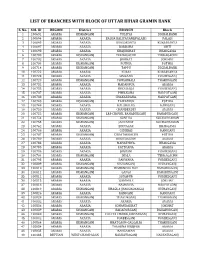
List of Branches with Block of Uttar Bihar Gramin Bank
LIST OF BRANCHES WITH BLOCK OF UTTAR BIHAR GRAMIN BANK S. No. SOL ID REGION District BRANCH Block 1 100691 ARARIA KISHANGANJ TULSIYA DIGHALBANK 2 100694 ARARIA ARARIA BALUA KALIYAGANJ(PALASI) PALASI 3 100695 ARARIA ARARIA KURSAKANTA KURSAKANTA 4 100697 ARARIA ARARIA BARDAHA SIKTI 5 100698 ARARIA ARARIA KHAJURIHAT BHARGAMA 6 100700 ARARIA KISHANGANJ TERHAGACHH TERRAGACHH 7 100702 ARARIA ARARIA JOKIHAT JOKIHAT 8 100704 ARARIA KISHANGANJ POTHIA POTHIA 9 100714 ARARIA KISHANGANJ TAPPU DIGHALBANK 10 100722 ARARIA ARARIA KUARI KURSAKANTA 11 100723 ARARIA ARARIA SIMRAHA FORBESGANJ 12 100729 ARARIA KISHANGANJ POWAKHALI THAKURGANJ 13 100732 ARARIA ARARIA MADANPUR ARARIA 14 100733 ARARIA ARARIA DHOLBAJJA FORBESGANJ 15 100737 ARARIA ARARIA PHULKAHA NARPATGANJ 16 100738 ARARIA ARARIA CHAKARDAHA. NARPATGANJ 17 100748 ARARIA KISHANGANJ TAIYABPUR POTHIA 18 100749 ARARIA ARARIA KALABALUA RANIGANJ 19 100750 ARARIA ARARIA CHANDERDEI ARARIA 20 100752 ARARIA KISHANGANJ LRP CHOWK, BAHADURGANJ BAHADURGANJ 21 100754 ARARIA KISHANGANJ SONTHA KOCHADHAMAN 22 100755 ARARIA KISHANGANJ JANTAHAT KOCHADHAMAN 23 100762 ARARIA ARARIA BIRNAGAR BHARGAMA 24 100766 ARARIA ARARIA GIDHBAS RANIGANJ 25 100767 ARARIA KISHANGANJ CHHATARGACHH POTHIA 26 100780 ARARIA ARARIA KUSIYARGAW ARARIA 27 100783 ARARIA ARARIA MAHATHWA. BHARGAMA 28 100785 ARARIA ARARIA PATEGANA. ARARIA 29 100786 ARARIA ARARIA JOGBANI FORBESGANJ 30 100794 ARARIA KISHANGANJ JHALA TERRAGACHH 31 100795 ARARIA ARARIA PARWAHA FORBESGANJ 32 100809 ARARIA KISHANGANJ KISHANGANJ KISHANGANJ 33 100810 ARARIA KISHANGANJ -
Araria Introduction
DISTRICT PROFILE ARARIA INTRODUCTION Araria, which was earlier a sub-division of Purina, became a full-fledged district on January 14, 1990, after the division of Purnia into three districts, namely Purnia, Araria and Kishanganj. This showery district of north-eastern Bihar is one of the most backward districts of Bihar, standing at the bottom of the 90 minority concentration districts. Borders of Araria are surrounded by Nepal in northern side, Kishanganj in eastern side and Supaul at western side. District border is adjacent to border of Nepal, so the district is important in terms of security. HISTORICAL BACKGROUND The territory of the present-day district became Araria sub-division of the erstwhile Purnia district in 1964. In ancient times Araria was ruled by three important clans of Indian history. The important tribe of Kiratas governed the northern side, while the eastern side was under the Pundras and area west of the river Kosi, at that time flowing somewhere near the present Araria, by Angas. During the Mauryan period this area formed the part of the Mauryan Empire and according to Asokavadana the Emperor Asoka put to death many naked heretics of this area who had done despite to the Budhist religion. In the 6th century A.D. the area south of the Himalayan pilgrim center of Varaha Kshetra, namely the Gupta kings Budhgupta and Devagupta gave Koti-varsha for the maintenance of the said pilgrim centre. In the first war of independence of 1857 Araria also witnessed a few skirmishes between the mutineers and the commissioner Yule’s forces, which took place near Nathpur. -

2010-2011 West-Champaran, Bihar
DISTRICT HEALTH ACTION PLAN 2010-2011 DISTRICT HEALTH SOCIETY West-Champaran, Bihar 1 PREFACE National Rural Health Mission (NRHM) is one of the major health schemes run by Ministry of health and family welfare, GoI. The basic concept of the mission is to enhance the access of Quality health services to the poorest of the poor of the society and improve the health status of the community. It envisages to improve the health status of the rural mass through various programmes. All the health services should be provided to the pregnant women such as ANC checkups, Post Natal Care, IFA tablets for restricting the enemia cases and other reproductive child health releted services. It also focuses on promotion of institutional delivery for restricting the infant and as well as maternal deaths. Immunization is also a very important component which plays a vital role in child and mother health. Family planning and control of other diseases are also other focus areas. The NRHM has a strong realization that it is important to involve community for the improvement of health status of the community through various stake holders such as ASHA, AWWs, PRI, NGOs etc. ASHA is a link worker between the client and the health service providers. The skill of the health functionaries such as ANMs LHVs should be upgraded through proper orientation to ensure quality of care in health services . Apart from that there is a need to strengthen the infrastructure and area of human resource for getting the quality of care in health services at the health centres . To achieve the better health status of the District, there is need to develop a District Health Action plan. -
Need for Vigorous Implementation of Npp-2000 in Bihar : an Empirical Study
HUNGRY PEOPLE AND EMPTY HANDS : NEED FOR VIGOROUS IMPLEMENTATION OF N.P.P.-2000 IN BIHAR : AN EMPIRICAL STUDY SPONSORED BY THE PLANNING COMMISSION GOVT. OF INDIA NEW DELHI CONDUCTED BY PROF. CHAKRADHAR SINHA UNIVERSITY PROFESSOR & HEAD (RETD.) UNIVERSITY DEPARTMENT OF ECONOMICS BRA BIHAR UNIVERSITY MUZAFFARPUR (BIHAR) Planning Commission Project “HUNGRY PEOPLE AND EMPTY HANDS : NEED FOR VIGOROUS IMPLEMENTATION OF N.P.P.-2000 IN BIHAR : AN EMPIRICAL STUDY” under Prof. Chakradhar Sinha as P.I. A Research Project entitled “HUNGRY PEOPLE AND EMPTY HANDS : NEED FOR VIGOROUS IMPLEMENTATION OF N.P.P.- 2000 IN BIHAR : AN EMPIRICAL STUDY” submitted by Dr. Chakradhar Sinha, Retd. Professor of Economics, BRA Bihar University, was approved by Planning Commission, Govt. of India vide letter No. O- 15012/82/2001-SER dated 28.02.2003. The Under Secretary to Govt. of India, conveyed the approval of the President of India for Grant-in- aid of Rs. 4.33 Lacs (Rupees four lacs thirty three thousand only) to the Registrar, BRA Bihar University, Muzaffarpur (Bihar) for conducting this Research Project. Out of the above amount of Rs. 4.33 Lacs, the Planning Commission provided to BRA Bihar University, Muzaffarpur, a sum of Rs. 1,73,200/- (Rupees One lac seventy three thousand two hundred only) on 22/4/2003. Subsequently, another instalment of Rs. 1,73,200/- was provided to the host university on 30/4/2004. Thus a sum of Rs.3,46,400/- (Rupees Three lacs forty six thousand four hundred only) has been paid to the host university, i.e. BRA Bihar University, Muzaffarpur.