Nsambya Community Home-Based Care Complements National HIV and TB Management Efforts and Contributes to Health Systems Strengthening in Uganda: an Observational Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Hiv and Aids Uganda Country Progress Report 2014
THE HIV AND AIDS UGANDA COUNTRY PROGRESS REPORT 2014 The First Lady of the Republic of Uganda and national EMTCT champion taking a public HIV test at Kololo grounds at the launch of the EMTCT campaign in KCCA Plot 1-3 Salim Bey Road, Ntinda Nakawa Division; P.O.Box 10779, Kampala- Uganda Tel: +256-414288065 Fax: +256-41-Email:[email protected] Website:http://www.aidsuganda.org 15th June, 2015 2014 Uganda HIV and AIDS Country Progress report Pagei NAFOPHANU National Forum of People with ABBREVIATIONS AND ACRONYMS HIV/AIDS Network in Uganda NASA National AIDS Spending Assessment ACP AIDS Control Program NDP National Development Plan AIDS Acquired Immune Deficiency NGO Non-Governmental Organization Syndrome NMS National Medical Stores AIS AIDS Indicator Survey NPAP National Priority Action Plan (for ANC Antenatal care HIV/AIDS) ART Antiretroviral Therapy or Treatment NSP National Strategic Plan (for HIV/AIDS) ARVs Antiretroviral Drugs NTLP National TB and Leprosy Control BCC Behaviour Change Communication Program CDC Centres for Disease Control NTRL National TB Reference Laboratory CPHL Central Public Health Laboratory OI Opportunistic Infection CSO Civil Society Organization OVC Orphans and Vulnerable Children DHS Demographic and Health Survey PACE Program for Accessible health, EID Early Infant Diagnosis Communication and Education eMTCT Elimination of Mother-to-Child PCR Polymerase Chain Reaction Transmission (of HIV) PEP Post-Exposure Prophylaxis FBO Faith Based Organization PEPFAR US Presidential Emergency Fund for GARPR Global AIDS Response -
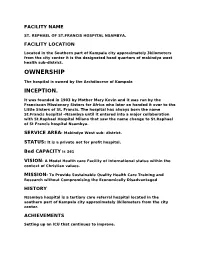
St. Rephael of St.Francis Hospital Nsambya
FACILITY NAME ST. REPHAEL OF ST.FRANCIS HOSPITAL NSAMBYA. FACILITY LOCATION Located in the Southern part of Kampala city approximately 3kilometers from the city center it is the designated head quarters of makindye west health sub-district. OWNERSHIP The hospital is owned by the Archdiocese of Kampala INCEPTION. It was founded in 1903 by Mother Mary Kevin and it was run by the Franciscan Missionary Sisters for Africa who later on handed it over to the Little Sisters of St. Francis. The hospital has always born the name St.Francis hospital –Nsambya until it entered into a major collaboration with St.Raphael Hospital Milano that saw the name change to St.Raphael of St Francis hospital Nsambya. SERVICE AREA: Makindye West sub- district. STATUS: It is a private not for profit hospital. Bed CAPACITY is 361 VISION: A Model Health care Facility of International status within the context of Christian values. MISSION: To Provide Sustainable Quality Health Care Training and Research without Compromising the Economically Disadvantaged HISTORY Nsambya hospital is a tertiary care referral hospital located in the southern part of Kampala city approximately 3kilometers from the city center. ACHIEVEMENTS Setting up an ICU that continues to improve. Setting up a quality assurance department that monitors quality continuously and we are now establishing standard operating procedures to assure quality. Very well equipped laboratory service and of recent a modern histopathology unit Set up a modern out patient department that awaits opening. Infection prevention and control is being practiced since its introduction with the continuous supervision of the infection prevention and control committee. -

Kampala Cholera Situation Report
Kampala Cholera Situation Report Date: Monday 4th February, 2019 1. Summary Statistics No Summary of cases Total Number Total Cholera suspects- Cummulative since start of 54 #1 outbreak on 2nd January 2019 1 New case(s) suspected 04 2 New cases(s) confirmed 54 Cummulative confirmed cases 22 New Deaths 01 #2 3 New deaths in Suspected 01 4 New deaths in Confirmed 00 5 Cumulative cases (Suspected & confirmed cases) 54 6 Cumulative deaths (Supected & confirmed cases) in Health Facilities 00 Community 03 7 Total number of cases on admission 00 8 Cummulative cases discharged 39 9 Cummulative Runaways from isolation (CTC) 07 #3 10 Number of contacts listed 93 11 Total contacts that completed 9 day follow-up 90 12 Contacts under follow-up 03 13 Total number of contacts followed up today 03 14 Current admissions of Health Care Workers 00 13 Cummulative cases of Health Care Workers 00 14 Cummulative deaths of Health Care Workers 00 15 Specimens collected and sent to CPHL today 04 16 Cumulative specimens collected 45 17 Cummulative cases with lab. confirmation (acute) 00 Cummulative cases with lab. confirmation (convalescent) 22 18 Date of admission of last confirmed case 01/02/2019 19 Date of discharge of last confirmed case 02/02/2019 20 Confirmed cases that have died 1 (Died from the community) #1 The identified areas are Kamwokya Central Division, Mutudwe Rubaga, Kitintale Zone 10 Nakawa, Naguru - Kasende Nakawa, Kasanga Makindye, Kalambi Bulaga Wakiso, Banda Zone B3, Luzira Kamwanyi, Ndeba-Kironde, Katagwe Kamila Subconty Luwero District, -

I UGANDA MARTYRS UNIVERSITY MOTHER KEVIN POSTGRADUATE
UGANDA MARTYRS UNIVERSITY MOTHER KEVIN POSTGRADUATE MEDICAL SCHOOL SHORT TERM POOR OUTCOME DETERMINANTS OF PATIENTS WITH TRAUMATIC PELVIC FRACTURES: A CROSSECTIONAL STUDY AT THREE PRIVATE NOT FOR PROFIT HOSPITALS OF NSAMBYA, LUBAGA AND MENGO. PRINCIPAL INVESTIGATOR: OSUTA HOPE METHUSELAH, MBChB (KIU) REG. NO: 2016/M181/10017 SUPERVISORS: 1- MR MUTYABA FREDERICK – MBChB(MUK), M.MED SURGERY, FCS ORTHOPAEDICS 2- SR.DR. NASSALI GORRETTI - MBChB(MUK), M.MED SURGERY, FCS A DISSERTATION TO BE SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE AWARD OF THE DEGREE OF MASTER OF MEDICINE IN SURGERY OF UGANDA MARTYRS UNIVERSITY © AUGUST 2018 i DEDICATION I dedicate this work to my dear wife, children and siblings for their faith in me, their unwavering love and support and to my teachers for their availability, patience, guidance, shared knowledge and moral support. ii AKNOWLEDGEMENT I would like to acknowledge all the patients whose information we used in this study and the institutions in which we conducted this study, for graciously granting us access to relevant data and all the support. I also would like to express my sincere gratitude to my dissertation supervisors, Mr. Mutyaba Frederick and Sr.Dr. Nassali Gorretti whose expertise, understanding, and patience have added substantially to my masters’ experience and this dissertation in particular. Special thanks go out to Professor. Kakande Ignatius, the Late Mr. Ekwaro Lawrence, Mr. Mugisa Didace, Mr. Muballe Boysier, Mr. Ssekabira John. Mr. Kiryabwire Joel, Dr.Basimbe Francis, Dr. Magezi Moses, Sr.Dr. Nabawanuka Assumpta, Dr. Nakitto Grace, Dr. Ssenyonjo Peter, my senior and junior colleagues in this journey, the Nursing Staff, the Radiology, Laboratory and Records staff whose expertise, assistance and guidance have been invaluable through my postgraduate journey. -

Doctoral Dissertation Announcement
Doctoral Dissertation Announcement Ronald Anguzu “Intimate Partner Violence during pregnancy in Uganda: Healthcare Provider screening practices, policymaker perspectives and spatial accessibility to antenatal care services” Candidate for Doctor of Philosophy in Public and Community Health Division of Epidemiology Institute for Health and Equity Graduate School of Biomedical Sciences Medical College of Wisconsin Committee in Charge: Laura D. Cassidy, PhD, MS (Chair) Rebekah J. Walker, PhD, MS Kirsten M.M. Beyer, PhD, MPH, MS Harriet Babikako, PhD, MPH, MBChB Julia Dickson-Gomez, PhD, MA Monday, May 24th, 2021 9:00 AM (CST) Live Public Viewing: https://mcw-edu.zoom.us/j/91474142263?pwd=MEdhQk14c2FZb0txa0Q1bUFEYWFUZz09 1 Graduate studies Biostatistics I Introduction to Epidemiology Community Health Improvement I Qualitative and Mixed Methods Doctoral Seminar Community Health Improvement III Community Health Improvement IV Introduction to Statistical Analysis using Stata Qualitative Data Analysis Ethics and Integrity in Science Readings and Research Foundations of Maternal and Child Health Regression Analysis – Stata Survey Research Methods Theories and Models of Health Behavior Research Ethics Discussion Series Community Health Improvement II Health and Medical Geography Doctoral Dissertation 2 DISSERTATION Intimate Partner Violence during pregnancy in Uganda: Healthcare Provider screening practices, policymaker perspectives and spatial accessibility to antenatal care services ABSTRACT Background: Globally, intimate partner violence (IPV) -

Missionary Medicine and Primary/Universal Health Care: the Case of Uganda
Missionary Medicine and Primary/Universal Health Care: The Case of Uganda Dr Shane Doyle University of Leeds Healthcare for all? • Can effective healthcare be provided at low cost to the bulk of the population even in poor countries? • Do mission institutions have a role to play in Recovering children with mothers in a pediatric malaria ward in Butare. Photograph: David Evans/National the provision of Geographic/Getty Images universal elementary healthcare and preventive services? 2 Was missionary medicine primarily ‘a tool for evangelization’ (J. McCracken) • Medical mission: • ‘used as heavy artillery . in the less responsive fields (H. Lankester) • ‘has to treat the physical problem of suffering and disease, and it has to deal with the spiritual and moral problem of sin’ (A. Cook) Or was medical mission penitential? • For Albert Schweitzer medical mission was a means of righting ‘the injustice and cruelties that in the course of centuries [Africans] have suffered at the hands of Europeans’ Is missionary medicine compatible with universal and primary healthcare? Mission healthcare may seem to policy-makers to provide a structural obstacle to the integration, coordination and consistency implied by universal health coverage. Whereas Universal and Primary Healthcare have a focus on the community, on prevention, mission medicine by reputation focuses on the curative, on the individual, and on its own adherents. Medical mission focused on groups which were defined as particularly vulnerable, or especially important to the religious aims of the mission. • Missions concentrated on relief for disadvantaged groups such as lepers, the blind and the crippled, ‘biblical manifestations of disease and misery’. Maternity provision in Uganda. -

Factors Affecting Adoption, Implementation and Sustainability of Telemedicine Information Systems in Uganda
Journal of Health Informatics in Developing Countries Submitted: November 5, 2011 Accepted: November 7, 2011 Factors Affecting Adoption, Implementation and Sustainability of Telemedicine Information Systems in Uganda Dr. STEPHEN R. ISABALIJAa,1, KITUYI G. MAYOKAb, Dr. AGNES S. RWASHANAc and Prof. VICTOR W. MBARIKAd aDepartment of Business Administration, Faculty of Entrepreneurship and Business Administration, Makerere University Business School [email protected] bDepartment of Business Computing, Faculty of Computing and Management Science, Makerere University Business School [email protected] cDepartment of Information Systems, College of Computing and Informatics Technology, Makerere University [email protected] dInternational Center for Info. Tech. and Development, Southern University (USA) [email protected] Abstract. Telemedicine has become a method of choice for improved access to quality healthcare services world over. The technology, which has been used for decades in the developed world, is now being diffused to developing countries. However, many initiatives have not lived to their expectations. In this paper, we present some of the main hindrances to telemedicine adoption, implementation and sustainability in Uganda. Case studies were carried out in two hospitals that have attempted to use the technology. Both qualitative and quantitative research methods were used to collect and analyze the data. Our findings indicate that the key factors affecting telemedicine in Uganda were lack of telemedicine policy, knowledge and skills and resistance to change by members of staff in the hospitals. A discussion of the findings inline with some selected technology adoption theories and models is done. We have also identified and discussed the key requirements for sustainable telemedicine in Uganda. 1 Stephen R. -

Approved Bodaboda Stages
Approved Bodaboda Stages SN Division Parish Stage ID X-Coordinate Y-Coordinate 1 CENTRAL DIVISION BUKESA 1001 32.563999 0.317146 2 CENTRAL DIVISION BUKESA 1002 32.564999 0.317240 3 CENTRAL DIVISION BUKESA 1003 32.566799 0.319574 4 CENTRAL DIVISION BUKESA 1004 32.563301 0.320431 5 CENTRAL DIVISION BUKESA 1005 32.562698 0.321824 6 CENTRAL DIVISION BUKESA 1006 32.561100 0.324322 7 CENTRAL DIVISION INDUSTRIAL AREA 1007 32.610802 0.312010 8 CENTRAL DIVISION INDUSTRIAL AREA 1008 32.599201 0.314553 9 CENTRAL DIVISION KAGUGUBE 1009 32.565701 0.325353 10 CENTRAL DIVISION KAGUGUBE 1010 32.569099 0.325794 11 CENTRAL DIVISION KAGUGUBE 1011 32.567001 0.327003 12 CENTRAL DIVISION KAGUGUBE 1012 32.571301 0.327249 13 CENTRAL DIVISION KAMWOKYA II 1013 32.583698 0.342530 14 CENTRAL DIVISION KOLOLO I 1014 32.605900 0.326255 15 CENTRAL DIVISION KOLOLO I 1015 32.605400 0.326868 16 CENTRAL DIVISION MENGO 1016 32.567101 0.305112 17 CENTRAL DIVISION MENGO 1017 32.563702 0.306650 18 CENTRAL DIVISION MENGO 1018 32.565899 0.307312 19 CENTRAL DIVISION MENGO 1019 32.567501 0.307867 20 CENTRAL DIVISION MENGO 1020 32.567600 0.307938 21 CENTRAL DIVISION MENGO 1021 32.569500 0.308241 22 CENTRAL DIVISION MENGO 1022 32.569199 0.309950 23 CENTRAL DIVISION MENGO 1023 32.564800 0.310082 24 CENTRAL DIVISION MENGO 1024 32.567600 0.311253 25 CENTRAL DIVISION MENGO 1025 32.566002 0.311941 26 CENTRAL DIVISION OLD KAMPALA 1026 32.567501 0.314132 27 CENTRAL DIVISION OLD KAMPALA 1027 32.565701 0.314559 28 CENTRAL DIVISION OLD KAMPALA 1028 32.566002 0.314855 29 CENTRAL DIVISION OLD -

Slum Settlement Profile Comes at an Opportune Time – a Time When the City of Kampala Is Experiencing Unprecedented Growth in the History of Uganda
FOREWORD This Slum Settlement Profile comes at an opportune time – a time when the city of Kampala is experiencing unprecedented growth in the history of Uganda. This growth and expansion is visible through the mushrooming of informal settlements across the different divisions of Kampala, especially in the low-lying areas of the city. This expansion has definitely exerted enormous pressure on land, with the poor occupying open spaces and the rich pushing the poor out of settlements for commercial and more formalised developments. The urban infrastructure (services and utilities) has not been spared as many residents demand for better quality water, sewer/ sanitation facilities, electricity, roads, security, and proper solid waste management systems. While the city still grapples with serving the existing communities, there are thousands that are flocking to the city in search of employment opportunities and better services. The invisible challenge for both the city and the communities has been lack of data/ information concerning the informal settlements, leading to a very wide gap between the plans and the priorities for the slum residents. The variables looked at in this Slum Profile include, among other factors, Security of Tenure, Housing, Water and Sanitation, Economic Activities, Accessibility, Drainage, and Solid Waste Management. Perhaps, the most outstanding and profound aspect is that this Slum Profile is not a collection of information from lawyers, teachers, doctors, or academicians, but rather ideas from the real slum dwellers who interface with the day-to- day challenges of slum life. KAMPALA PROFILES: MAKINDYE Page 1 TABLE OF CONTENTS FOREWORD ........................................................................................................................................................ 1 PROFILE METHODOLOGY ................................................................................................................................ 3 A. -

Abstracts and Conference Reports from International Workshops on Infectious Diseases & Antiviral Therapy
L A T R I H V E I T R N A A P Y N I REVIEWSI in Antiviral Therapy N S I E Reviews N S F A E 2013 C SE INFECTIOUS DISEASES &TIOUS DI & 7 JOURNAL OF ABSTRACTS AND CONFERENCE REPORTS FROM INTERNATIONAL WORKSHOPS ON INFECTIOUS DISEASES & ANTIVIRAL THERAPY Abstract Book Reviews in Antiviral Therapy & Infectious Diseases 5th International Workshop on HIV Pediatrics 28 - 29 June 2013, Kuala Lumpur, Malaysia 7/2013 a medical education company Abstracts 1 th 5 International Workshop on HIV Pediatrics 28 – 29 June 2013, Kuala Lumpur, Malaysia Abstracts Oral presentations Reviews in Antiviral Therapy & Infectious Diseases – Volume 7: 2013 Abstracts 2 Reviews in Antiviral Therapy & Infectious Diseases – Volume 7: 2013 Abstracts 3 Abstract: O_01 129/145 (89%) by pill count. Median daily LPV dose was 543 (447-619) mg/m2/day. Median Treatment of pediatric HIV infection trough plasma LPV concentration was 6.7 (4.1- 9.6) mg/L in 61 children with available samples. Median LPV hair concentrations were Lopinavir hair concentrations 5.43 (3.21 - 9.01) when VL was >1000 and predict virological failure 9.96 (6.51 - 12.31) ng/mg of hair when VL was among Asian children <1000 copies/mL. Plasma and hair LPV levels were not strongly correlated (Pearson’s correlation coefficient = 0.20; p=0.13). In 1 1 2 W. Prasitsuebsai , S.J. Kerr , T.H. Khanh , J. univariate models, age, sex, body surface 1 3 4 5 Ananworanich , D.C. Viet , L.N. Van , N. Kurniati , P. area, LPV plasma trough level and <95% 6 7 8 Kosalaraksa , V. -
Planned Shutdown Web October 2020.Indd
PLANNED SHUTDOWN FOR SEPTEMBER 2020 SYSTEM IMPROVEMENT AND ROUTINE MAINTENANCE REGION DAY DATE SUBSTATION FEEDER/PLANT PLANNED WORK DISTRICT AREAS & CUSTOMERS TO BE AFFECTED Kampala West Saturday 3rd October 2020 Mutundwe Kampala South 1 33kV Replacement of rotten vertical section at SAFARI gardens Najja Najja Non and completion of flying angle at MUKUTANO mutundwe. North Eastern Saturday 3rd October 2020 Tororo Main Mbale 1 33kV Create Two Tee-offs at Namicero Village MBALE Bubulo T/C, Bududa Tc Bulukyeke, Naisu, Bukigayi, Kufu, Bugobero, Bupoto Namisindwa, Magale, Namutembi Kampala West Sunday 4th October 2020 Kampala North 132/33kV 32/40MVA TX2 Routine Maintenance of 132/33kV 32/40MVA TX 2 Wandegeya Hilton Hotel, Nsooda Atc Mast, Kawempe Hariss International, Kawempe Town, Spencon,Kyadondo, Tula Rd, Ngondwe Feeds, Jinja Kawempe, Maganjo, Kagoma, Kidokolo, Kawempe Mbogo, Kalerwe, Elisa Zone, Kanyanya, Bahai, Kitala Taso, Kilokole, Namere, Lusanjja, Kitezi, Katalemwa Estates, Komamboga, Mambule Rd, Bwaise Tc, Kazo, Nabweru Rd, Lugoba Kazinga, Mawanda Rd, East Nsooba, Kyebando, Tilupati Industrial Park, Mulago Hill, Turfnel Drive, Tagole Cresent, Kamwokya, Kubiri Gayaza Rd, Katanga, Wandegeya Byashara Street, Wandegaya Tc, Bombo Rd, Makerere University, Veterans Mkt, Mulago Hospital, Makerere Kavule, Makerere Kikumikikumi, Makerere Kikoni, Mulago, Nalweuba Zone Kampala East Sunday 4th October 2020 Jinja Industrial Walukuba 11kV Feeder Jinja Industrial 11kV feeders upgrade JINJA Walukuba Village Area, Masese, National Water Kampala East -

Croc's July 1.Indd
CLASSIFIED ADVERTS NEW VISION, Monday, July 1, 2013 57 BUSINESS INFORMATION MAYUGE SUGAR INDUSTRIES LTD. SERVICE Material Testing EMERGENCY VACANCIES POLICE AND FIRE BRIGADE: Ring: 999 or 342222/3. One of the fastest developing and THE ONLY 6. BOILER ATTENDANT - 3 Posts Africa Air Rescue (AAR) 258527, MANUFACTURER OF SULPHURLESS SUGAR IN Boiler Attendant Certificate Holders with 3-5 258564, 258409. EAST AFRICA based in Uganda. The organization yrs working experience preferred (Thermo ELECTRICAL FAILURE: Ring is engaged in the manufacturing of “Nile Sugar” fluid handling) UMEME on185. and soon starting the manufacturing of Extra 7. SR. ELECTRICAL & INSTRUMENTATION ENGR. MATERIAL TESTING AND SURVEY EQUIPMENT Water: Ring National Water and Neutral Alcohol Invites applications for below - 1Post Sewerage Corporation on 256761/3, 242171, 232658. Telephone inquiry: posts; B.E.(electrical & instrumentation) or equallent Material Testing UTL-900, Celtel 112, MTN-999, 112 1. SHIFT CHEMIST FOR DISTILLATION - 3 Posts with experience of 15 years FUNERAL SERVICES Must have 3-5 years of experience in PLC/ 8. ELECTRICAL ENGR - 1 Post Aggregates impact Value Kampala Funeral Directors, SKADA system independent operation . Diploma in Electrical Engr.or equallent with Apparatus Bukoto-Ntinda Road. P.O. Box 9670, Qualification :-B.SC.Alco,Tech or Diploma in exp of 5 yrs Flakiness Gauge&Flakiness Chem Eng. 9. INSTRUMENTATION ENGR. - 1 Post Kampala. Tel: 0717 533533, 0312 Sleves 533533. 2. LABORATORY CHEMIST SHIFT - 3 Posts Diploma in Instrumentation or equallent with Los Angeles Abrasion Machine Uganda Funeral Services For Mol Analysis /Spirit Analysis /Q.C exp of 5 yrs H/Q 80A Old Kira Road, Bukoto Checking/Spent wash loss checking etc 10.