Guidelines for Using Ketamine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Severe Organophosphate Poisoning with Delayed Cholinergic Crisis, Intermediate Syndrome and Organophosphate Induced Delayed Polyneuropathy on Succession
Organophosphate Poisoning… Aklilu A 203 CASE REPORT SEVERE ORGANOPHOSPHATE POISONING WITH DELAYED CHOLINERGIC CRISIS, INTERMEDIATE SYNDROME AND ORGANOPHOSPHATE INDUCED DELAYED POLYNEUROPATHY ON SUCCESSION Aklilu Azazh ABSTRACT Organophosphate compounds are the organic derivatives of Phosphorous containing acids and their effect on neuromuscular junction and Autonomic Synapses is clinically important. After exposure these agents cause acute and sub acute manifestations depending on the type and severity of the agents like Acute Cholinergic Manifestations, Intermediate Syndrome with Nicotinic features and Delayed Central Nervous System Complications. The patient reported here had severe Organophosphate Poisoning with various rare complications on a succession. This is the first report of Organophosphates Poisoning complicated by Intermediate Syndrome and Organophosphate Induced Delayed Polyneuropathy in Ethiopia and it is reported to increase awareness of health care workers on these rare complications of a common problem. INTRODUCTION phosphorylated by the Phosphate end of Organophosphates; then the net result is Organophosphate compounds are the organic accumulation of excessive Acetyl Chlorine with derivatives of Phosphorous containing acids and resultant effect on Muscarinic, Nicotinic and their effect on Neuromuscular Junction and central nervous system (Figure 2). Autonomic synapses is clinically important. In the Neuromuscular Junction Acetylcholine is released Following classical OP poisoning, three well when a nerve impulse reaches -

Biased Versus Partial Agonism in the Search for Safer Opioid Analgesics
molecules Review Biased versus Partial Agonism in the Search for Safer Opioid Analgesics Joaquim Azevedo Neto 1 , Anna Costanzini 2 , Roberto De Giorgio 2 , David G. Lambert 3 , Chiara Ruzza 1,4,* and Girolamo Calò 1 1 Department of Biomedical and Specialty Surgical Sciences, Section of Pharmacology, University of Ferrara, 44121 Ferrara, Italy; [email protected] (J.A.N.); [email protected] (G.C.) 2 Department of Morphology, Surgery, Experimental Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] (A.C.); [email protected] (R.D.G.) 3 Department of Cardiovascular Sciences, Anesthesia, Critical Care and Pain Management, University of Leicester, Leicester LE1 7RH, UK; [email protected] 4 Technopole of Ferrara, LTTA Laboratory for Advanced Therapies, 44122 Ferrara, Italy * Correspondence: [email protected] Academic Editor: Helmut Schmidhammer Received: 23 July 2020; Accepted: 23 August 2020; Published: 25 August 2020 Abstract: Opioids such as morphine—acting at the mu opioid receptor—are the mainstay for treatment of moderate to severe pain and have good efficacy in these indications. However, these drugs produce a plethora of unwanted adverse effects including respiratory depression, constipation, immune suppression and with prolonged treatment, tolerance, dependence and abuse liability. Studies in β-arrestin 2 gene knockout (βarr2( / )) animals indicate that morphine analgesia is potentiated − − while side effects are reduced, suggesting that drugs biased away from arrestin may manifest with a reduced-side-effect profile. However, there is controversy in this area with improvement of morphine-induced constipation and reduced respiratory effects in βarr2( / ) mice. Moreover, − − studies performed with mice genetically engineered with G-protein-biased mu receptors suggested increased sensitivity of these animals to both analgesic actions and side effects of opioid drugs. -

Methadone Hydrochloride Tablets, USP) 5 Mg, 10 Mg Rx Only
ROXANE LABORATORIES, INC. Columbus, OH 43216 DOLOPHINE® HYDROCHLORIDE CII (Methadone Hydrochloride Tablets, USP) 5 mg, 10 mg Rx Only Deaths, cardiac and respiratory, have been reported during initiation and conversion of pain patients to methadone treatment from treatment with other opioid agonists. It is critical to understand the pharmacokinetics of methadone when converting patients from other opioids (see DOSAGE AND ADMINISTRATION). Particular vigilance is necessary during treatment initiation, during conversion from one opioid to another, and during dose titration. Respiratory depression is the chief hazard associated with methadone hydrochloride administration. Methadone's peak respiratory depressant effects typically occur later, and persist longer than its peak analgesic effects, particularly in the early dosing period. These characteristics can contribute to cases of iatrogenic overdose, particularly during treatment initiation and dose titration. In addition, cases of QT interval prolongation and serious arrhythmia (torsades de pointes) have been observed during treatment with methadone. Most cases involve patients being treated for pain with large, multiple daily doses of methadone, although cases have been reported in patients receiving doses commonly used for maintenance treatment of opioid addiction. Methadone treatment for analgesic therapy in patients with acute or chronic pain should only be initiated if the potential analgesic or palliative care benefit of treatment with methadone is considered and outweighs the risks. Conditions For Distribution And Use Of Methadone Products For The Treatment Of Opioid Addiction Code of Federal Regulations, Title 42, Sec 8 Methadone products when used for the treatment of opioid addiction in detoxification or maintenance programs, shall be dispensed only by opioid treatment programs (and agencies, practitioners or institutions by formal agreement with the program sponsor) certified by the Substance Abuse and Mental Health Services Administration and approved by the designated state authority. -

Opioid Analgesics These Are General Guidelines
Adult Opioid Reference Guide June 2012 Opioid Analgesics These are general guidelines. Patient care requires individualization based on patient needs and responses. Lower doses should be used initially, then titrated up to achieve pain relief, especially if the patient has not been taking opioids for the past week (opioid naïve). Patients who have been taking scheduled opioids for at least the previous 5 days may be considered “opioid tolerant”. These patients may require higher doses for analgesia. Drug # Route Starting Dose Onset Peak Duration Metabolism Half Life Comments (Adults > 50 Kg) Buprenorphine Trans- 5 mcg/hr q 7 DAYS 17 hr 60 hr 7 DAYS Liver 26 hr Maximum dose = 20 mcg/hr patch dermal Extensively metabolized by CYP3A4 enzymes – watch for Example: Butrans® drug interactions Transdermal patches are not available at UIHC Codeine PO 30 - 60 mg q 4 hr 30 min 1½ hr 6 hr Liver 2 - 4 hr Oral not recommended first-line therapy. Some patients cannot metabolize codeine to active morphine. Fentanyl IM 5 mcg/Kg q 1 - 2 hr 7 - 8 min 20 - 50 min 1 - 2 hr Liver 1 - 6 hr* Give IV slowly over several minutes to prevent chest wall IV 0.25 - 1 mcg/Kg as Immediate 1 - 5 min 30 - 60 min rigidity SQ needed Refer to the formulary for administration and monitoring. May be used in patients with renal impairment as it has no active metabolites. Accumulates in adipose tissue with continuous infusion. Trans- 25 mcg/hr 12 - 24 hr 24 hr 48 - 72 hr Transdermal should NOT be used to treat acute pain. -

Protocol for a Randomised Controlled Trial: Efficacy of Donepezil Against
BMJ Open: first published as 10.1136/bmjopen-2013-003533 on 25 September 2013. Downloaded from Open Access Protocol Protocol for a randomised controlled trial: efficacy of donepezil against psychosis in Parkinson’s disease (EDAP) Hideyuki Sawada, Tomoko Oeda To cite: Sawada H, Oeda T. ABSTRACT ARTICLE SUMMARY Protocol for a randomised Introduction: Psychosis, including hallucinations and controlled trial: efficacy of delusions, is one of the important non-motor problems donepezil against psychosis Strengths and limitations of this study in patients with Parkinson’s disease (PD) and is in Parkinson’s disease ▪ In previous randomised controlled trials for (EDAP). BMJ Open 2013;3: possibly associated with cholinergic neuronal psychosis the efficacy was investigated in patients e003533. doi:10.1136/ degeneration. The EDAP (Efficacy of Donepezil against who presented with psychosis and the primary bmjopen-2013-003533 Psychosis in PD) study will evaluate the efficacy of endpoint was improvement of psychotic symp- donepezil, a brain acetylcholine esterase inhibitor, for toms. By comparison, this study is designed to prevention of psychosis in PD. ▸ Prepublication history for evaluate the prophylactic effect in patients this paper is available online. Methods and analysis: Psychosis is assessed every without current psychosis. Because psychosis To view these files please 4 weeks using the Parkinson Psychosis Questionnaire may be overlooked and underestimated it is visit the journal online (PPQ) and patients with PD whose PPQ-B score assessed using a questionnaire, Parkinson (http://dx.doi.org/10.1136/ (hallucinations) and PPQ-C score (delusions) have Psychosis Questionnaire (PPQ) every 4 weeks. bmjopen-2013-003533). been zero for 8 weeks before enrolment are ▪ The strength of this study is its prospective randomised to two arms: patients receiving donepezil design using the preset definition of psychosis Received 3 July 2013 hydrochloride or patients receiving placebo. -
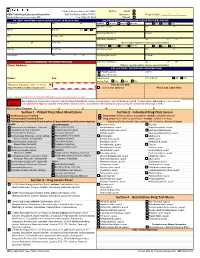
Quantitative Drug Test Menu Section 2
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Nitrous Oxide in Emergency Medicine Í O’ Sullivan, J Benger
214 ANALGESIA Emerg Med J: first published as 10.1136/emj.20.3.214 on 1 May 2003. Downloaded from Nitrous oxide in emergency medicine Í O’ Sullivan, J Benger ............................................................................................................................. Emerg Med J 2003;20:214–217 Safe and predictable analgesia is required for the identify these zones as there is considerable vari- potentially painful or uncomfortable procedures often ation between people. He also emphasised the importance of the patient’s pre-existing beliefs. If undertaken in an emergency department. The volunteers expect to fall asleep while inhaling characteristics of an ideal analgesic agent are safety, 30% N2O then a high proportion do so. An appro- predictability, non-invasive delivery, freedom from side priate physical and psychological environment increases the actions of N2O and may allow lower effects, simplicity of use, and a rapid onset and offset. doses to be more effective. Unlike many other Newer approaches have threatened the widespread use anaesthetic agents, N2O exhibits an acute toler- of nitrous oxide, but despite its long history this simple ance effect, whereby its potency is greater at induction than after a period of “accommoda- gas still has much to offer. tion”. .......................................................................... MECHANISM OF ACTION “I am sure the air in heaven must be this Some writers have suggested that N2O, like wonder-working gas of delight”. volatile anaesthetics, causes non-specific central nervous system depression. Others, such as 4 Robert Southey, Poet (1774 to 1843) Gillman, propose that N2O acts specifically by interacting with the endogenous opioid system. HISTORY N2O is known to act preferentially on areas of the Nitrous oxide (N2O) is the oldest known anaes- brain and spinal cord that are rich in morphine thetic agent. -

Analgesic Indications: Developing Drug and Biological Products
Guidance for Industry Analgesic Indications: Developing Drug and Biological Products DRAFT GUIDANCE This guidance document is being distributed for comment purposes only. Comments and suggestions regarding this draft document should be submitted within 60 days of publication in the Federal Register of the notice announcing the availability of the draft guidance. Submit electronic comments to http://www.regulations.gov. Submit written comments to the Division of Dockets Management (HFA-305), Food and Drug Administration, 5630 Fishers Lane, rm. 1061, Rockville, MD 20852. All comments should be identified with the docket number listed in the notice of availability that publishes in the Federal Register. For questions regarding this draft document contact Sharon Hertz at 301-796-2280. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) February 2014 Clinical/Medical 5150dft.doc 01/15/14 Guidance for Industry Analgesic Indications: Developing Drug and Biological Products Additional copies available from: Office of Communications, Division of Drug Information Center for Drug Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave., Bldg. 51, rm. 2201 Silver Spring, MD 20993-0002 Tel: 301-796-3400; Fax: 301-847-8714; E-mail: [email protected] http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) February -

Adverse Reactions to Hallucinogenic Drugs. 1Rnstttutton National Test
DOCUMENT RESUME ED 034 696 SE 007 743 AUTROP Meyer, Roger E. , Fd. TITLE Adverse Reactions to Hallucinogenic Drugs. 1rNSTTTUTTON National Test. of Mental Health (DHEW), Bethesda, Md. PUB DATP Sep 67 NOTE 118p.; Conference held at the National Institute of Mental Health, Chevy Chase, Maryland, September 29, 1967 AVATLABLE FROM Superintendent of Documents, Government Printing Office, Washington, D. C. 20402 ($1.25). FDPS PRICE FDPS Price MFc0.50 HC Not Available from EDRS. DESCPTPTOPS Conference Reports, *Drug Abuse, Health Education, *Lysergic Acid Diethylamide, *Medical Research, *Mental Health IDENTIFIEPS Hallucinogenic Drugs ABSTPACT This reports a conference of psychologists, psychiatrists, geneticists and others concerned with the biological and psychological effects of lysergic acid diethylamide and other hallucinogenic drugs. Clinical data are presented on adverse drug reactions. The difficulty of determining the causes of adverse reactions is discussed, as are different methods of therapy. Data are also presented on the psychological and physiolcgical effects of L.S.D. given as a treatment under controlled medical conditions. Possible genetic effects of L.S.D. and other drugs are discussed on the basis of data from laboratory animals and humans. Also discussed are needs for futher research. The necessity to aviod scare techniques in disseminating information about drugs is emphasized. An aprentlix includes seven background papers reprinted from professional journals, and a bibliography of current articles on the possible genetic effects of drugs. (EB) National Clearinghouse for Mental Health Information VA-w. Alb alb !bAm I.S. MOMS Of NAM MON tMAN IONE Of NMI 105 NUNN NU IN WINES UAWAS RCM NIN 01 NUN N ONMININI 01011110 0. -

The Role of Serotonin in Memory: Interactions with Neurotransmitters and Downstream Signaling
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Bushehr University of Medical Sciences Repository Exp Brain Res (2014) 232:723–738 DOI 10.1007/s00221-013-3818-4 REVIEW The role of serotonin in memory: interactions with neurotransmitters and downstream signaling Mohammad Seyedabadi · Gohar Fakhfouri · Vahid Ramezani · Shahram Ejtemaei Mehr · Reza Rahimian Received: 28 April 2013 / Accepted: 20 December 2013 / Published online: 16 January 2014 © Springer-Verlag Berlin Heidelberg 2014 Abstract Serotonin, or 5-hydroxytryptamine (5-HT), is there has been an alteration in the density of serotonergic found to be involved in many physiological or pathophysi- receptors in aging and Alzheimer’s disease, and serotonin ological processes including cognitive function. Seven dis- modulators are found to alter the process of amyloidogen- tinct receptors (5-HT1–7), each with several subpopulations, esis and exert cognitive-enhancing properties. Here, we dis- have been identified for serotonin, which are different in cuss the serotonin-induced modulation of various systems terms of localization and downstream signaling. Because involved in mnesic function including cholinergic, dopa- of the development of selective agonists and antagonists minergic, GABAergic, glutamatergic transmissions as well for these receptors as well as transgenic animal models as amyloidogenesis and intracellular pathways. of cognitive disorders, our understanding of the role of serotonergic transmission in learning and memory has Keywords Serotonin · Memory · Signaling pathways improved in recent years. A large body of evidence indi- cates the interplay between serotonergic transmission and Abbreviations other neurotransmitters including acetylcholine, dopamine, 2PSDT Two-platform spatial discrimination task γ-aminobutyric acid (GABA) and glutamate, in the neu- 3xTg-AD Triple-transgenic mouse model of Alzheimer’s robiological control of learning and memory. -

Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the Use of Antiemetics Author(S): Dr Annette Edwards (Chai
Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the use of Antiemetics Author(s): Dr Annette Edwards (Chair) and Deborah Royle on behalf of the Yorkshire Palliative Medicine Clinical Guidelines Group Overall objective : To provide guidance on the evidence for the use of antiemetics in specialist palliative care. Search Strategy: Search strategy: Medline, Embase and Cinahl databases were searched using the words nausea, vomit$, emesis, antiemetic and drug name. Review Date: March 2008 Competing interests: None declared Disclaimer: These guidelines are the property of the Yorkshire Palliative Medicine Clinical Guidelines Group. They are intended to be used by qualified, specialist palliative care professionals as an information resource. They should be used in the clinical context of each individual patient’s needs. The clinical guidelines group takes no responsibility for any consequences of any actions taken as a result of using these guidelines. Contact Details: Dr Annette Edwards, Macmillan Consultant in Palliative Medicine, Department of Palliative Medicine, Pinderfields General Hospital, Aberford Road, Wakefield, WF1 4DG Tel: 01924 212290 E-mail: [email protected] 1 Introduction: Nausea and vomiting are common symptoms in patients with advanced cancer. A careful history, examination and appropriate investigations may help to infer the pathophysiological mechanism involved. Where possible and clinically appropriate aetiological factors should be corrected. Antiemetics are chosen based on the likely mechanism and the neurotransmitters involved in the emetic pathway. However, a recent systematic review has highlighted that evidence for the management of nausea and vomiting in advanced cancer is sparse. (Glare 2004) The following drug and non-drug treatments were reviewed to assess the strength of evidence for their use as antiemetics with particular emphasis on their use in the palliative care population. -

The Use of Cyclizine in Patients Receiving Parenteral Nutrition
DRAFT - The use of cyclizine in patients receiving parenteral nutrition Jeremy Nightingale, Uchu Meade, Gavin Leahy and the BIFA committee Cyclizine is a piperazine derivative that was discovered in 1947 while researching new antihistamine drugs (H1 blockers) and was first sold 1965. It is marketed for the treatment or prevention of nausea, vomiting, and labyrinthine disorders including vertigo and motion sickness. This includes nausea after a general anaesthetic and that caused by opioid use. In the United Kingdom the oral formulation is classified as a Pharmacy (P) medicine and can be sold from a registered pharmacy premises by or under the supervision of a pharmacist. The intravenous formulation is classified as a Prescription Only Medicine (POM). There is increasing recognition that the intravenous formulation of cyclizine may cause euphoria and dependence (addiction); these side effects may not be reported by patients and be under recognised by healthcare professionals. It has many associated problems when used by patients receiving long-term parenteral nutrition. This position paper highlights the risks associated with its long-term intravenous use. Actions/pharmacology (1) Cyclizine has both anti-histamine (H1) and anti-cholinergic (anti-muscarinic M1) effects. It is a class 1 drug in the biopharmaceutical classification (high permeability and solubility) with a peak plasma concentration of about 70 ng/ ml reached approximately 2 hours after oral ingestion, as measured in healthy adult patients. Its quoted elimination (biological) half-life is 20 hours when given orally (1) and 13 hours when given intravenously (2). Cyclizine is metabolised to its N-demethylated derivative, norcyclizine, which has little anti-histaminic (H1) activity compared to cyclizine.