Medications to Avoid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms and Clinical Significance of Pharmacokinetic-Based Drug-Drug Interactions With
DMD Fast Forward. Published on November 15, 2018 as DOI: 10.1124/dmd.118.084905 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 84905 Title Mechanisms and Clinical Significance of Pharmacokinetic-based Drug-drug Interactions with Drugs Approved by the U.S. Food and Drug Administration in 2017 Jingjing Yu, Ichiko D. Petrie, René H. Levy, and Isabelle Ragueneau-Majlessi Department of Pharmaceutics, School of Pharmacy, University of Washington, Seattle, WA, USA (J.Y., I.P., R.H.L. I.R-M.) Downloaded from dmd.aspetjournals.org at ASPET Journals on October 3, 2021 1 DMD Fast Forward. Published on November 15, 2018 as DOI: 10.1124/dmd.118.084905 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 84905 Running Title Page a) Running title: A review of clinical DDIs in 2017 NDAs b) Corresponding author: Jingjing Yu, Drug Interaction Database (DIDB) Program, Department of Pharmaceutics, School of Pharmacy, University of Washington, Box 357610, Seattle, WA 98195, Phone: 206.221.2856, Fax: 206.543.3204, E-mail: [email protected] c) Number of text pages: 18 Number of tables: 2 Downloaded from Number of figures: 2 Number of references: 38 Number of words in the Abstract: 242 dmd.aspetjournals.org Number of words in the Introduction: 227 Number of words in the Discussion: 619 d) Abbreviations: at ASPET Journals on October 3, 2021 AUC, area under the time-plasma concentration curve; BCRP, breast cancer resistance protein; Cmax, maximum plasma -

Treatment of Psychosis: 30 Years of Progress
Journal of Clinical Pharmacy and Therapeutics (2006) 31, 523–534 REVIEW ARTICLE Treatment of psychosis: 30 years of progress I. R. De Oliveira* MD PhD andM.F.Juruena MD *Department of Neuropsychiatry, School of Medicine, Federal University of Bahia, Salvador, BA, Brazil and Department of Psychological Medicine, Institute of Psychiatry, King’s College, University of London, London, UK phrenia. Thirty years ago, psychiatrists had few SUMMARY neuroleptics available to them. These were all Background: Thirty years ago, psychiatrists had compounds, today known as conventional anti- only a few choices of old neuroleptics available to psychotics, and all were liable to cause severe extra them, currently defined as conventional or typical pyramidal side-effects (EPS). Nowadays, new antipsychotics, as a result schizophrenics had to treatments are more ambitious, aiming not only to suffer the severe extra pyramidal side effects. improve psychotic symptoms, but also quality of Nowadays, new treatments are more ambitious, life and social reinsertion. We briefly but critically aiming not only to improve psychotic symptoms, outline the advances in diagnosis and treatment but also quality of life and social reinsertion. Our of schizophrenia, from the mid 1970s up to the objective is to briefly but critically review the present. advances in the treatment of schizophrenia with antipsychotics in the past 30 years. We conclude DIAGNOSIS OF SCHIZOPHRENIA that conventional antipsychotics still have a place when just the cost of treatment, a key factor in Up until the early 1970s, schizophrenia diagnoses poor regions, is considered. The atypical anti- remained debatable. The lack of uniform diagnostic psychotic drugs are a class of agents that have criteria led to relative rates of schizophrenia being become the most widely used to treat a variety of very different, for example, in New York and psychoses because of their superiority with London, as demonstrated in an important study regard to extra pyramidal symptoms. -

Inbrija, INN-Levodopa
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Inbrija 33 mg inhalation powder, hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each hard capsule contains 42 mg levodopa. Each delivered dose contains 33 mg levodopa. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Inhalation powder, hard capsule. White opaque capsules containing white powder, with “A42” printed in black on the cap of the capsule and two black bands printed on the body of the capsule. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Inbrija is indicated for the intermittent treatment of episodic motor fluctuations (OFF episodes) in adult patients with Parkinson’s disease (PD) treated with a levodopa/dopa-decarboxylase inhibitor. 4.2 Posology and method of administration Posology Patients should be on a stable levodopa/dopa-decarboxylase inhibitor (e.g. carbidopa or benserazide) regimen before starting Inbrija. Patients selected for treatment with Inbrija should be able to recognize the onset of their 'OFF' symptoms and be capable of preparing the inhaler or else have a responsible care giver able to prepare the inhaler for them when required. Inbrija should be inhaled when symptoms, motor or non-motor, of an OFF period start to return. The recommended dose of Inbrija is 2 hard capsules up to 5 times per day each delivering 33 mg levodopa. The maximum daily dose of Inbrija should not exceed 10 capsules (330 mg). It is not recommended to take more than 2 capsules per OFF period. Exceeding the recommended dose may lead to increased levodopa associated adverse reactions. -

Serotonin 2A Activation and a Novel Therapeutic Drug
Psychopharmacology (2018) 235:3083–3091 https://doi.org/10.1007/s00213-018-5042-1 THEORETICAL AND METHODOLOGICAL PERSPECTIVE The neuropharmacology of sleep paralysis hallucinations: serotonin 2A activation and a novel therapeutic drug Baland Jalal1 Received: 23 April 2018 /Accepted: 17 September 2018 /Published online: 5 October 2018 # The Author(s) 2018 Abstract Sleep paralysis is a state of involuntary immobility occurring at sleep onset or offset, often accompanied by uncanny Bghost-like^ hallucinations and extreme fear reactions. I provide here a neuropharmacological account for these hallucinatory experiences by evoking the role of the serotonin 2A receptor (5-HT2AR). Research has shown that 5-HT2AR activation can induce visual hallucinations, Bmystical^ subjective states, and out-of-body experiences (OBEs), and modulate fear circuits. Hallucinatory experiences triggered by serotonin—serotonergic (Bpseudo^) hallucinations, induced by hallucinogenic drugs—tend to be Bdream-like^ with the experiencer having insight (Bmeta-awareness^) that he is hallucinating, unlike dopaminergic (Bpsychotic^ and Blife-like^) hallucinations where such insight is lost. Indeed, hallucinatory experiences during sleep paralysis have the classic features of serotonergic hallucinations, and are strikingly similar to perceptual and subjective states induced by hallucinogenic drugs (e.g., lysergic acid diethylamide [LSD] and psilocybin), i.e., they entail visual hallucinations, mystical experiences, OBEs, and extreme fear reactions. I propose a possible mechanism whereby serotonin could be functionally implicated in generating sleep paralysis hallucinations and fear reactions through 5-HT2AR activity. Moreover, I speculate on the role of 5-HT2C receptors vis-à-vis anxiety and panic during sleep paralysis, and the orbitofrontal cortex—rich with 5-HT2A receptors—in influencing visual pathways during sleep paralysis, and, in effect, hallucinations. -

Atypical Antipsychotics TCO 02.2018
Therapeutic Class Overview Atypical Antipsychotics INTRODUCTION • Antipsychotic medications have been used for over 50 years to treat schizophrenia and a variety of other psychiatric disorders (Miyamato et al 2005). • Antipsychotic medications generally exert their effect in part by blocking dopamine (D)-2 receptors (Jibson et al 2017). • Antipsychotics are divided into 2 distinct classes based on their affinity for D2 and other neuroreceptors: typical antipsychotics, also called first-generation antipsychotics (FGAs), and atypical antipsychotics, also called second- generation antipsychotics (SGAs) (Miyamato et al 2005). • Atypical antipsychotics do not have a uniform pharmacology or mechanism of action; these differences likely account for the different safety and tolerability profiles of these agents (Clinical Pharmacology 2020, Jibson et al 2017). The atypical antipsychotics differ from the early antipsychotics in that they have affinity for the serotonin 5-HT2 receptor in addition to D2. Clozapine is an antagonist at all dopamine receptors (D1-5), with lower affinity for D1 and D2 receptors and high affinity for D4 receptors. Aripiprazole and brexpiprazole act as partial agonists at the D2 receptor, functioning as an ○ agonist when synaptic dopamine levels are low and as an antagonist when they are high. Cariprazine is a partial agonist at D2 and D3. Pimavanserin does not have dopamine blocking activity and is primarily an inverse agonist at 5-HT2A receptors. The remaining atypical antipsychotics share the similarity of D2 and 5-HT2A -
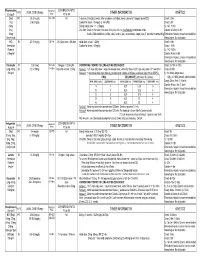
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
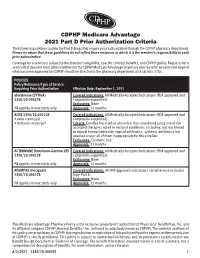
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria
CDPHP Medicare Advantage 2021 Part D Prior Authorization Criteria The following guidelines outline the Part D drugs that require prior authorization through the CDPHP pharmacy department. Please be aware that these guidelines do not reflect those instances in which it is the member’s responsibility to seek prior authorization. Coverage for a service is subject to the member’s eligibility, specific contract benefits, and CDPHP policy. Requests for a service that does not meet criteria outlined in the CDPHP Medicare Advantage pharmacy policies or for an extension beyond what has been approved by CDPHP should be directed to the pharmacy department at (518) 641-3784. POLICIES Policy Reference/Type of Service Requiring Prior Authorization Effective Date: September 1, 2021 abiraterone (ZYTIGA) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ACNE 1350/20.000118 Covered indications: All Medically-Accepted Indications (FDA approved and • avita cream/gel compendia-supported). • tretinoin cream/gel Criteria: Enrollee has tried or prescriber has considered using one of the accepted therapies noted in national guidelines, including, but not limited to topical benzoyl peroxide, topical antibiotics, systemic antibiotics but deemed one or all of them inappropriate for the enrollee. Exclusions: Cosmetic Use. Approvals: 12 months. ACTIMMUNE (Interferon-Gamma 1B) Covered indications: All Medically-Accepted Indications (FDA approved and 1350/20.000278 compendia-supported). Exclusions: None PA applies to new starts only Approvals: 12 months. ADEMPAS (riociguat) Covered indications: All FDA-approved indications not otherwise excluded 1350/20.000278 from Part D. -
Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -

The Effects of Valbenazine in Participants with Tardive Dyskinesia
SAFETY PROFILE In the extension period, valbenazine was generally well tolerated in a population of LONG-TERM TREATMENT WITH patients with diagnosed schizophrenia, schizoaffective disorder, or mood disorder.8 ONCE-DAILY VALBENAZINE MAY BE AN EFFECTIVE TREATMENT Treatment-emergent adverse events ≥5% in either valbenazine treatment group8,j FOR TD IN ADULTS WITH A • Headache (7.1%) • Dizziness (5.6%) • Urinary tract infection (6.6%) • Suicidal ideation (5.1%) RANGE OF PRESENTATIONS AND • Diarrhea (5.6%) • Depression (4.0%) TREATMENT HISTORIES8 j Combined valbenazine 40 mg and 80 mg once daily.8 • Valbenazine was generally well tolerated through 48 weeks, with There were no clinically important changes in clinical laboratory assessments, sustained TD reductions vital signs, or ECG parameters during the extension or washout periods.8 • TD symptoms tended to return to Psychiatric status generally remained stable during the extension study.8 baseline during the washout period, supporting the maintenance efficacy of ongoing valbenazine treatment LONG-TERM RESULTS AIMS mean score showed sustained TD reduction AIMS score reduction by ≥50% was generally through Week 488,9 consistent through Week 488 Extension study of valbenazine 40 mg and Percentage of extension study participants valbenazine 80 mg (ITT population)10 with AIMS responsel 1.0 100 90 0.0 -0.1 80 -1.0 -1.3 -1.1 -1.4 70 -1.8 -2.0 -2.3 60 -2.2 -2.9 52.4% -2.5 48.0% -3.0 -2.5 50 46.0% -3.0 P<0.001m -3.5 -3.5 40.0% 41.2% 40 -4.0 -4.2 m 28.8% 28.3% -4.2 -4.8 30 P<0.05 -4.3 -4.4 23.8% 23.4% -

Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the Use of Antiemetics Author(S): Dr Annette Edwards (Chai
Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the use of Antiemetics Author(s): Dr Annette Edwards (Chair) and Deborah Royle on behalf of the Yorkshire Palliative Medicine Clinical Guidelines Group Overall objective : To provide guidance on the evidence for the use of antiemetics in specialist palliative care. Search Strategy: Search strategy: Medline, Embase and Cinahl databases were searched using the words nausea, vomit$, emesis, antiemetic and drug name. Review Date: March 2008 Competing interests: None declared Disclaimer: These guidelines are the property of the Yorkshire Palliative Medicine Clinical Guidelines Group. They are intended to be used by qualified, specialist palliative care professionals as an information resource. They should be used in the clinical context of each individual patient’s needs. The clinical guidelines group takes no responsibility for any consequences of any actions taken as a result of using these guidelines. Contact Details: Dr Annette Edwards, Macmillan Consultant in Palliative Medicine, Department of Palliative Medicine, Pinderfields General Hospital, Aberford Road, Wakefield, WF1 4DG Tel: 01924 212290 E-mail: [email protected] 1 Introduction: Nausea and vomiting are common symptoms in patients with advanced cancer. A careful history, examination and appropriate investigations may help to infer the pathophysiological mechanism involved. Where possible and clinically appropriate aetiological factors should be corrected. Antiemetics are chosen based on the likely mechanism and the neurotransmitters involved in the emetic pathway. However, a recent systematic review has highlighted that evidence for the management of nausea and vomiting in advanced cancer is sparse. (Glare 2004) The following drug and non-drug treatments were reviewed to assess the strength of evidence for their use as antiemetics with particular emphasis on their use in the palliative care population. -

The Effects of Antipsychotic Treatment on Metabolic Function: a Systematic Review and Network Meta-Analysis
The effects of antipsychotic treatment on metabolic function: a systematic review and network meta-analysis Toby Pillinger, Robert McCutcheon, Luke Vano, Katherine Beck, Guy Hindley, Atheeshaan Arumuham, Yuya Mizuno, Sridhar Natesan, Orestis Efthimiou, Andrea Cipriani, Oliver Howes ****PROTOCOL**** Review questions 1. What is the magnitude of metabolic dysregulation (defined as alterations in fasting glucose, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels) and alterations in body weight and body mass index associated with short-term (‘acute’) antipsychotic treatment in individuals with schizophrenia? 2. Does baseline physiology (e.g. body weight) and demographics (e.g. age) of patients predict magnitude of antipsychotic-associated metabolic dysregulation? 3. Are alterations in metabolic parameters over time associated with alterations in degree of psychopathology? 1 Searches We plan to search EMBASE, PsycINFO, and MEDLINE from inception using the following terms: 1 (Acepromazine or Acetophenazine or Amisulpride or Aripiprazole or Asenapine or Benperidol or Blonanserin or Bromperidol or Butaperazine or Carpipramine or Chlorproethazine or Chlorpromazine or Chlorprothixene or Clocapramine or Clopenthixol or Clopentixol or Clothiapine or Clotiapine or Clozapine or Cyamemazine or Cyamepromazine or Dixyrazine or Droperidol or Fluanisone or Flupehenazine or Flupenthixol or Flupentixol or Fluphenazine or Fluspirilen or Fluspirilene or Haloperidol or Iloperidone