4. Oral Pathology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Picture of the Month
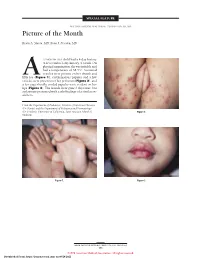
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

Management of Anterior Spacing with Peg Lateral by Interdisciplinary Approach : a Case Report
Case Report Management of Anterior Spacing with Peg Lateral by Interdisciplinary Approach : A Case Report Dr Sanjay Prasad Gupta Assistant Professor & Consultant Orthodontist, Department of Orthodontics, Tribhuvan University Teaching Hospital, Institute of Medicine, Kathmandu Correspondence: Dr Sanjay Prasad Gupta; Email: [email protected] ABSTRACT Anterior spacing is a common esthetic problem of patient during dental consultation. The most common etiology include tooth size and arch length discrepancy. Maxillary lateral incisors vary in form more than any other tooth in the mouth except the third molars. Microdontia is a condition where the teeth are smaller than the normal size. Microdontia of maxillary lateral incisor is called as “peg lateral”, that exhibit converging mesial and distal surfaces of crown forming a cone like shape. A carefully documented diagnosis and treatment plan are essential if the clinician is to apply the most effective approach to address the patient’s needs. A patient sometimes requires a multidisciplinary approach to correct the esthetics and to improve the occlusion. This case report describes the management of an adult female patient with a proclined upper anterior teeth, upper anterior spacing, deep bite and peg shaped upper right lateral incisor tooth through orthodontic and restorative treatment approach. Key words: Anterior spacing, Peg lateral, Esthetic, Interdisciplinary approach INTRODUCTION Peg shaped lateral incisors occur in approximately 2% to 5% of the general population, and women show a Maxillary lateral incisors vary in form more than any slightly higher frequency than men. Usually they are found other tooth in the mouth except the third molars. If the equally on the right and left, uni or bilaterally, however variation is too great, it is considered a developmental some studies have shown their bilateral occurrence anomaly.1 Developmental alterations which are most slightly higher than the unilateral occurrence. -

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -
Small Dog, Big Smile
Small Dog, Big Smile How to make sure your little dog has a happy, healthy mouth Christine Hawke Sydney Pet Dentistry INTRODUCTION Hello and thanks for downloading my book, ‘Small Dog, Big Smile – How to make sure your little dog has a happy, healthy mouth’. Small dogs are gorgeous, and deservedly very popular throughout the world. Centuries of careful and selective breeding has provided us with a huge range of small breeds to choose from, each with their own specific characteristics and charm. While good things certainly come in small packages, one of the drawbacks of their small size is that many of these dogs suffer silently from serious dental issues. While all dog breeds are susceptible to ‘teething problems’, periodontal infection and orthodontic disorders, dogs with small mouths have the added issue of overcrowded teeth to contend with. Similar to their larger ancestors, they have to find space for 42 teeth, which is sometimes no easy feat. As a result, things don’t always go according to plan…. My name is Christine Hawke, and I am a veterinarian with almost 20 years experience in small animal practice. After many years in general practice, I developed a passion for all things dental, and have been running a small animal dentistry-only practice in Sydney since 2007. I am a Member of the Australian and New Zealand College of Veterinary Scientists in the field of Veterinary Dentistry (this can only be attained through examination), and the American Veterinary Dental Society. I am currently the President of the Australian Veterinary Dental Society, and teach veterinary dentistry to vet students (at The University of Sydney), vets and nurses across Australia. -

Keratocystic Odontogenic Tumour Mimicking As a Dentigerous Cyst – a Rare Case Report Dr
DOI: 10.21276/sjds.2017.4.3.16 Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2017; 4(3):154-157 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Keratocystic Odontogenic Tumour Mimicking as a Dentigerous Cyst – A Rare Case Report Dr. K. Saraswathi Gopal1, Dr. B. Prakash vijayan2 1Professor and Head, Department of Oral Medicine and Radiology, Meenakshi Ammal Dental College and Hospital, Chennai 2PG Student, Department of Oral Medicine and Radiology, Meenakshi Ammal Dental College and Hospital, Chennai *Corresponding author Dr. B. Prakash vijayan Email: [email protected] Abstract: Keratocystic odontogenic tumor (KCOT) formerly known as odontogenic keratocyst (OKC), is considered a benign unicystic or multicystic intraosseous neoplasm and one of the most aggressive odontogenic lesions presenting relatively high recurrence rate and a tendency to invade adjacent tissue. On the other hand Dentigerous cyst (DC) is one of the most common odontogenic cysts of the jaws and rarely recurs. They were very similar in clinical and radiographic characteristics. In our case a pathological report following incisional biopsy turned out to be dentigerous cyst and later as Keratocystic odontogenic tumour following total excision. The treatment was chosen in order to prevent any pathological fracture. A recurrence was noticed after 2 months following which the lesion was surgically enucleated. At 2-years of follow-up, patient showed no recurrence. Keywords: Dentigerous cyst, Keratocystic odontogenic tumour (KCOT), Recurrence, Enucleation INTRODUCTION Keratocystic odontogenic tumour (KCOT) is a CASE REPORT rare developmental, epithelial and benign cyst of the A 17-year-old patient reported to the OP with a jaws of odontogenic origin with high recurrence rates. -

Permanent Mandibular Incisor with Multiple Anomalies - Report of a Rare Clinical Case
Braz346 Dent J (2011) 22(4): 346-350 N. B. Nagaveni et al. ISSN 0103-6440 Permanent Mandibular Incisor with Multiple Anomalies - Report of a Rare Clinical Case Nayaka Basavanthappa NAGAVENI1 Kagathur Veerbadrapa UMASHANKARA2 B.G. VIDYULLATHA3 SREEDEVI3 Nayaka Basavanthappa RADHIKA4 1Department of Pedodontics and Preventive Dentistry, Hitkarini Dental College and Hospital, Jabalpur, Madhya Pradesh, India 2Department of Oral and Maxillofacial Surgery, Hitkarini Dental College and Hospital, Jabalpur, Madhya Pradesh, India 3Department of Oral Medicine and Radiology, Hitkarini Dental College and Hospital, Jabalpur, Madhya Pradesh, India 4Department of Orthodontics and Dentofacial Orthopedics, School of Dentistry, Krishna Institute of Medical Sciences, Satara district, Karad, Maharashtra, India Permanent mandibular central incisor is rarely affected by tooth shape anomalies of crown and root. Co-occurrence of multiple anomalies in a permanent mandibular central incisor is extremely rare. This paper reports an unusual concurrent combination of multiple dental anomalies affecting both the crown and root of a permanent mandibular left central incisor - talon cusp, dens invaginatus, short root anomaly and macrodontia -, which has not previously been reported together. Case management is described and implications are discussed. The dentist should be aware of these rare entities in order to provide an accurate diagnosis and management for which detailed examination of the tooth both clinically and radiographically is very important. Key Words: anomalies, dens invaginatus, mandibular incisor, short root anomaly, talon cusp. INTRODUCTION differentiation stage of tooth development (2). Dens invaginatus is also a rare developmental Morphological variations of dental structure anomaly defined as a deep surface invagination of the involving either crown or root are common in the crown or root, which is lined by enamel and resulting literature. -

Oral Health in Prevalent Types of Ehlers–Danlos Syndromes
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Ghent University Academic Bibliography J Oral Pathol Med (2005) 34: 298–307 ª Blackwell Munksgaard 2005 Æ All rights reserved www.blackwellmunksgaard.com/jopm Oral health in prevalent types of Ehlers–Danlos syndromes Peter J. De Coster1, Luc C. Martens1, Anne De Paepe2 1Department of Paediatric Dentistry, Centre for Special Care, Paecamed Research, Ghent University, Ghent; 2Centre for Medical Genetics, Ghent University Hospital, Ghent, Belgium BACKGROUND: The Ehlers–Danlos syndromes (EDS) Introduction comprise a heterogenous group of heritable disorders of connective tissue, characterized by joint hypermobility, The Ehlers–Danlos syndromes (EDS) comprise a het- skin hyperextensibility and tissue fragility. Most EDS erogenous group of heritable disorders of connective types are caused by mutations in genes encoding different tissue, largely characterized by joint hypermobility, skin types of collagen or enzymes, essential for normal pro- hyperextensibility and tissue fragility (1) (Fig. 1). The cessing of collagen. clinical features, modes of inheritance and molecular METHODS: Oral health was assessed in 31 subjects with bases differ according to the type. EDS are caused by a EDS (16 with hypermobility EDS, nine with classical EDS genetic defect causing an error in the synthesis or and six with vascular EDS), including signs and symptoms processing of collagen types I, III or V. The distribution of temporomandibular disorders (TMD), alterations of and function of these collagen types are displayed in dental hard tissues, oral mucosa and periodontium, and Table 1. At present, two classifications of EDS are was compared with matched controls. -

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated Through 445 Nm Diode Laser
healthcare Case Report A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated through 445 nm Diode Laser Maria Vittoria Viani 1,*, Luigi Corcione 1, Chiara Di Blasio 2, Ronell Bologna-Molina 3 , Paolo Vescovi 1 and Marco Meleti 1 1 Department of Medicine and Surgery, University of Parma, 43126 Parma, Italy; [email protected] (L.C.); [email protected] (P.V.); [email protected] (M.M.) 2 Private practice, Centro Medico Di Blasio, 43121 Parma; Italy; [email protected] 3 Faculty of Dentistry, University of the Republic, 14600 Montevideo, Uruguay; [email protected] * Correspondence: [email protected] Received: 10 June 2020; Accepted: 11 August 2020; Published: 13 August 2020 Abstract: Oral granular cell tumor (GCT) is a relatively rare, benign lesion that can easily be misdiagnosed. Particularly, the presence of pseudoepitheliomatous hyperplasia might, in some cases, lead to the hypothesis of squamous cell carcinoma. Surgical excision is the treatment of choice. Recurrence has been reported in up to 15% of cases treated with conventional surgery. Here, we reported a case of GCT of the tongue in a young female patient, which was successfully treated through 445 nm diode laser excision. Laser surgery might reduce bleeding and postoperative pain and may be associated with more rapid healing. Particularly, the vaporization effect on remnant tissues could eliminate GCT cells on the surgical bed, thus hypothetically leading to a lower rate of recurrence. In the present case, complete healing occurred in 1 week, and no recurrence was observed after 6 months. Laser surgery also allows the possibility to obtain second intention healing. -

June 18, 2013 8:30 Am – 11:30 Am
Tuesday – June 18, 2013 8:30 am – 11:30 am Poster Abstracts – Tuesday, June 18, 2013 #1 ORAL LESIONS AS THE PRESENTING MANIFESTATION OF CROHN'S DISEASE V Woo, E Herschaft, J Wang U of Nevada, Las Vegas Crohn’s disease (CD) is an immune-mediated disorder of the gastrointestinal tract which together with ulcerative colitis, comprise the two major types of inflammatory bowel disease (IBD). The underlying etiology has been attributed to defects in mucosal immunity and the intestinal epithelial barrier in a genetically susceptible host, resulting in an inappropriate inflammatory response to intestinal microbes. The lesions of CD can affect any region of the alimentary tract as well as extraintestinal sites such as the skin, joints and eyes. The most common presenting symptoms are periumbilical pain and diarrhea associated with fevers, malaise and anemia. Oral involvement has been termed oral CD and may manifest as lip swelling, cobblestoned mucosa, mucogingivitis and linear ulcerations and fissures. Oral lesions may precede gastrointestinal involvement and can serve as early markers of CD. We describe a 6-year-old male who presented for evaluation of multifocal gingival erythema and swellings. His medical history was unremarkable for gastrointestinal disorders or distress. Histopathologic examination showed multiple well-formed granulomas that were negative for special stains and foreign body material. A diagnosis of granulomatous gingivitis was rendered. The patient was advised to seek consultation with a pediatric gastroenterologist and following colonoscopy, was diagnosed with early stage CD. Timely recognition of the oral manifestations of CD is critical because only a minority of patients will continue to exhibit CD-specific oral lesions at follow-up. -

Spectrum of PEX1 and PEX6 Variants in Heimler Syndrome
European Journal of Human Genetics (2016) 24, 1565–1571 Official Journal of The European Society of Human Genetics www.nature.com/ejhg ARTICLE Spectrum of PEX1 and PEX6 variants in Heimler syndrome Claire EL Smith1, James A Poulter1, Alex V Levin2,3,4, Jenina E Capasso4, Susan Price5, Tamar Ben-Yosef6, Reuven Sharony7, William G Newman8,9, Roger C Shore10, Steven J Brookes10, Alan J Mighell1,11,12 and Chris F Inglehearn*,1,12 Heimler syndrome (HS) consists of recessively inherited sensorineural hearing loss, amelogenesis imperfecta (AI) and nail abnormalities, with or without visual defects. Recently HS was shown to result from hypomorphic mutations in PEX1 or PEX6,both previously implicated in Zellweger Syndrome Spectrum Disorders (ZSSD). ZSSD are a group of conditions consisting of craniofacial and neurological abnormalities, sensory defects and multi-organ dysfunction. The finding of HS-causing mutations in PEX1 and PEX6 shows that HS represents the mild end of the ZSSD spectrum, though these conditions were previously thought to be distinct nosological entities. Here, we present six further HS families, five with PEX6 variants and one with PEX1 variants, and show the patterns of Pex1, Pex14 and Pex6 immunoreactivity in the mouse retina. While Ratbi et al. found more HS-causing mutations in PEX1 than in PEX6, as is the case for ZSSD, in this cohort PEX6 variants predominate, suggesting both genes play a significant role in HS. The PEX6 variant c.1802G4A, p.(R601Q), reported previously in compound heterozygous state in one HS and three ZSSD cases, was found in compound heterozygous state in three HS families.