Oxytocin Administration and Amniotomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Preventing the First Cesarean Delivery
Current Commentary Preventing the First Cesarean Delivery Summary of a Joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal- Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop Catherine Y. Spong, MD, Vincenzo Berghella, MD, Katharine D. Wenstrom, MD, Brian M. Mercer, MD, and George R. Saade, MD points were identified to assist with reduction in cesar- With more than one third of pregnancies in the United ean delivery rates including that labor induction should States being delivered by cesarean and the growing be performed primarily for medical indication; if done knowledge of morbidities associated with repeat cesar- for nonmedical indications, the gestational age should be ean deliveries, the Eunice Kennedy Shriver National Insti- at least 39 weeks or more and the cervix should be favor- tute of Child Health and Human Development, the able, especially in the nulliparous patient. Review of the Society for Maternal-Fetal Medicine, and the American current literature demonstrates the importance of adher- College of Obstetricians and Gynecologists convened ing to appropriate definitions for failed induction and a workshop to address the concept of preventing the first arrest of labor progress. The diagnosis of “failed induc- cesarean delivery. The available information on maternal tion” should only be made after an adequate attempt. and fetal factors, labor management and induction, and Adequate time for normal latent and active phases of nonmedical factors leading to the first cesarean delivery the first stage, and for the second stage, should be was reviewed as well as the implications of the first allowed as long as the maternal and fetal conditions per- cesarean delivery on future reproductive health. -

Labor and Vaginal Delivery
VI LABOR, DELIVERY, AND POSTPARTUM LABOR AND VAGINAL DELIVERY Kelly A. Best, MD CHAPTER 61 1. What is the definition of labor? Labor begins when uterine contractions of sufficient frequency, intensity, and duration are attained to bring about effacement and progressive dilation of the cervix. 2. What two steps are theorized to be crucial to the initiation of labor in human pregnancy? 1. Retreat from pregnancy maintenance 2. Uterotonic induction Despite extensive investigation into the associated physiologic and biochemical changes, the physiologic processes in human pregnancy that result in the onset of labor are still not defined. 3. In which patients is induction of labor considered? Awaiting the onset of normal labor may not be an option in certain circumstances. At preterm gestations, indications for labor induction include severe preeclampsia, fetal growth restriction with abnormal antepartum surveillance or other evidence of fetal compromise, and deterioration of maternal disease to the point that continuation of pregnancy is believed to be detrimental. In cases of rupture of membranes without labor (i.e., premature rupture of membranes) at term (37 to 42 weeks) or postterm (≥42 weeks), induction of labor is often performed. 4. What is a Bishop score, and how is it used? A Bishop score is a quantifiable method to assess the likelihood of a successful induction. Elements include dilation, effacement, station, consistency, and position of the cervix (Table 61-1). A score of 6 or less trans- lates into a need to ripen the cervix and is associated with less successful inductions. A score 8 or greater generally means the cervix does not need ripening and induction is more likely to be successful. -

Intra-Vaginal Prostaglandin E2 Versus Double-Balloon Catheter for Labor Induction in Term Oligohydramnios
Journal of Perinatology (2015) 35, 95–98 © 2015 Nature America, Inc. All rights reserved 0743-8346/15 www.nature.com/jp ORIGINAL ARTICLE Intra-vaginal prostaglandin E2 versus double-balloon catheter for labor induction in term oligohydramnios G Shechter-Maor1, G Haran1, D Sadeh-Mestechkin1, Y Ganor-Paz1, MD Fejgin1,2 and T Biron-Shental1,2 OBJECTIVE: Compare mechanical and pharmacological ripening for patients with oligohydramnios at term. STUDY DESIGN: Fifty-two patients with oligohydramnios ⩽ 5 cm and Bishop score ⩽ 6 were randomized for labor induction with a vaginal insert containing 10 mg timed-release dinoprostone (PGE2) or double-balloon catheter. The primary outcome was time from induction to active labor. Time to labor, neonatal outcomes and maternal satisfaction were also compared. RESULT: Baseline characteristics were similar. Time from induction to active labor (13 with PGE2 vs 19.5 h with double-balloon catheter; P = 0.243) was comparable, with no differences in cesarean rates (15.4 vs 7.7%; P = 0.668) or neonatal outcomes. The PGE2 group had higher incidence of early device removal (76.9 vs 26.9%; P = 0.0001), mostly because of active labor or non-reassuring fetal heart rate. Fewer PGE2 patients required oxytocin augmentation for labor induction (53.8 vs 84.6% P = 0.034). Time to delivery was significantly shorter with PGE2 (16 vs 20.5 h; P = 0. 045) CONCLUSION: Intravaginal PGE2 and double-balloon catheter are comparable methods for cervical ripening in term pregnancies with oligohydramnios. Journal of Perinatology (2015) 35, 95–98; doi:10.1038/jp.2014.173; published online 2 October 2014 INTRODUCTION better mimic the natural course of labor and might have an Ultrasound estimation of amniotic fluid volume is an important advantage in cervical ripening. -

Confidential: for Review Only Continued Versus Discontinued Oxytocin Stimulation in the Active Phase of Labour (CONDISOX)- a Double-Blind Randomised Controlled Trial
BMJ Confidential: For Review Only Continued versus discontinued oxytocin stimulation in the active phase of labour (CONDISOX)- A double-blind randomised controlled trial Journal: BMJ Manuscript ID BMJ-2020-063027 Article Type: Research BMJ Journal: BMJ Date Submitted by the 09-Nov-2020 Author: Complete List of Authors: Boie, Sidsel; Randers Regional Hospital, Obstetrics and Gynaecology Glavind, Julie; Aarhus University Hospital, Obstetrics and Gynaecology Uldbjerg, Niels; Aarhus University Hospital, Obstetrics and Gynecology Steer, Philip; Imperial College London, Academic Department of Obstetrics and Gynaecology Bothazi, Attila; Aalborg University Hospital, Obstetrics and Gynaecology Sundtoft, Iben ; Hospitalsenheden Vest, Obstetrics and Gynaecology Bakker, Jannet; Amsterdam UMC Location AMC, Obstetrics and Gynaecology Van der Post, Joris; Amsterdam UMC Location AMC, Obstetrics and Gynaecology Renault, Kristina; Rigshospitalet, Obstetrics and Gynaecology Huusom, Lene; Hvidovre Hospital, Obstetrics and Gynaecology Hvidman, Lone; Aarhus University Hospital, Obstetrics and Gynaecology Rask, Maja; Odense University Hospital, Obstetrics and Gynaecology Khalil, Mohammed; Sygehus Lillebalt Kolding Sygehus, Obstetrics and Gynaecology Møller, Nini; Nordsjaellands Hospital, Obstetrics and Gynaecology Greve, Tine; Hvidovre Hospital, Obstetrics and Gynaecology Bor, Pinar; Randers Regional Hospital, Obstetrics and Gynaecology induction of labour, oxytocin, discontinuation, Caesarean section, active Keywords: phase of labour, uterine tachysystole -

2020 CDA Paper Abstraction Forms
2020 OBI DATA ABSTRACTION FORMS DEMOGRAPHICS Hospital Name: Patient Last Name: Patient First Name: Medical Record Number (MRN): Maternal Birthdate (MM/DD/YY): Postal Zip Hispanic Ethnicity: Code: Hispanic or Latino Not Hispanic or Latino Race (select all that apply): Unknown American Indian or Alaskan Native Asian Patient's Insurance Type: Black or African American Medicaid Self Pay/None Native Hawaiian or Other Pacific Islander Private Other: __________ White Unknown LABOR MANAGEMENT: Admission L&D Admission Date: L&D Admission Time: Provider admitting patient to Labor & Delivery (Last Name, First Name): Service/Practice patient admitted to: Admitting Nurse (Last name, First name): Certified Nurse Midwife Family Practice / Family Medicine Gravidity on admission: Parity on admission: Maternal Fetal Medicine Obstetrics Physician Maternal Height at admission: Maternal Weight at admission: Pre-pregnancy Weight: IN LBS LBS CM K G KG Did the patient receive prenatal care? If yes, date prenatal care Transfer of care from an intended home birth? started: Yes No Unable to determine Yes No LABOR MANAGEMENT: Maternal Comorbidities Present On Admission Pre-pregnancy diabetes (Type I or Type II Yes Was the patient using opioids during this Yes diabetes diagnosed prior to this pregnancy) No pregnancy? No Gestational diabetes (diagnosis in this pregnancy Yes What was the status of the patient's opioid use during this with or without medication tx) No pregnancy? (select all that apply): In treatment for opioid use disorder during pregnancy Pre-pregnancy -

Terms/Definitions
9th Annual AABC Birth Institute 10/1/2015 HEAD COMPRESSION: PLAINTIFF’S NEW THEORY TO EXPLAIN CEREBRAL PALSY 9th ANNUAL AABC BIRTH INSTITUTE OCTOBER 1-4, 2015, SCOTTSDALE, AZ OCTOBER 2, 2015 Julia K. McNelis, R.N., J.D. Kitch Drutchas Wagner Valitutti & Sherbrook Mt. Clemens, Michigan (Detroit, Marquette, Lansing, Chicago, Toledo) Terms/Definitions • Freemans, 3rd Ed. 2003 • NICHD 2008 • ACOG 2009 • Williams, 23nd Ed. 2010 • Freeman’s, 4th Ed. 2012 1 9th Annual AABC Birth Institute 10/1/2015 Freeman’s 3rd Ed (2003) • Primary function of ctx is expulsion of uterine contents • Manual palpation has been traditional method of monitoring ctx • During labor strength varies 30mm Hg average early labor to 50 mm Hg later first stage • 50mm Hg to 80 mm Hg second stage • Once labor starts ctx become more frequent and stronger Freeman’s 3rd (2003) Fig 5.8 2 9th Annual AABC Birth Institute 10/1/2015 NICHD (2008) • Normal-5 or less ctx in 10 minutes, averaged over 30 minutes • Tachysystole-> 5 ctx in 10 minutes, averaged over 30 minutes • “Hyperstimulation” and “hypercontractility” are not defined and should be abandoned ACOG # 107 (2009) • Adopts NICHD definitions • Tachysystole should always be qualified as to the presence or absence of associated FHR decelerations • The term tachysystole applies to both spontaneous and stimulated labor 3 9th Annual AABC Birth Institute 10/1/2015 Williams 23 Ed. 2010 • Ctx in normal labor-forces are greatest and last longest at the fundus and diminish towards the cervix • The Montevideo group ascertained that the lowest limit of ctx pressure required to dilate the cervix is 15 mm Hg Williams 23 Ed. -

Misoprostol Tablets
Cytotec® misoprostol tablets WARNINGS CYTOTEC (MISOPROSTOL) ADMINISTRATION TO WOMEN WHO ARE PREGNANT CAN CAUSE BIRTH DEFECTS, ABORTION, PREMATURE BIRTH OR UTERINE RUPTURE. UTERINE RUPTURE HAS BEEN REPORTED WHEN CYTOTEC WAS ADMINISTERED IN PREGNANT WOMEN TO INDUCE LABOR OR TO INDUCE ABORTION. THE RISK OF UTERINE RUPTURE INCREASES WITH ADVANCING GESTATIONAL AGES AND WITH PRIOR UTERINE SURGERY, INCLUDING CESAREAN DELIVERY (see also PRECAUTIONS and LABOR AND DELIVERY). CYTOTEC SHOULD NOT BE TAKEN BY PREGNANT WOMEN TO REDUCE THE RISK OF ULCERS INDUCED BY NONSTEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDs) (see CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS). PATIENTS MUST BE ADVISED OF THE ABORTIFACIENT PROPERTY AND WARNED NOT TO GIVE THE DRUG TO OTHERS. Cytotec should not be used for reducing the risk of NSAID-induced ulcers in women of childbearing potential unless the patient is at high risk of complications from gastric ulcers associated with use of the NSAID, or is at high risk of developing gastric ulceration. In such patients, Cytotec may be prescribed if the patient has had a negative serum pregnancy test within 2 weeks prior to beginning therapy. is capable of complying with effective contraceptive measures. has received both oral and written warnings of the hazards of misoprostol, the risk of possible contraception failure, and the danger to other women of childbearing potential should the drug be taken by mistake. will begin Cytotec only on the second or third day of the next normal menstrual period. DESCRIPTION Cytotec oral tablets contain either 100 mcg or 200 mcg of misoprostol, a synthetic prostaglandin E1 analog. 1 Reference ID: 4228046 Misoprostol contains approximately equal amounts of the two diastereomers presented below with their enantiomers indicated by (±): Misoprostol is a water-soluble, viscous liquid. -

20180523 Vlemminx
Real-time electrohysterography Citation for published version (APA): Vlemminx, M. W. C. (2018). Real-time electrohysterography: a novel technology used on the labour ward. Technische Universiteit Eindhoven. Document status and date: Published: 23/05/2018 Document Version: Publisher’s PDF, also known as Version of Record (includes final page, issue and volume numbers) Please check the document version of this publication: • A submitted manuscript is the version of the article upon submission and before peer-review. There can be important differences between the submitted version and the official published version of record. People interested in the research are advised to contact the author for the final version of the publication, or visit the DOI to the publisher's website. • The final author version and the galley proof are versions of the publication after peer review. • The final published version features the final layout of the paper including the volume, issue and page numbers. Link to publication General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal. If the publication is distributed under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license above, please follow below link for the End User Agreement: www.tue.nl/taverne Take down policy If you believe that this document breaches copyright please contact us at: [email protected] providing details and we will investigate your claim. -

OBGYN-Study-Guide-1.Pdf
OBSTETRICS PREGNANCY Physiology of Pregnancy: • CO input increases 30-50% (max 20-24 weeks) (mostly due to increase in stroke volume) • SVR anD arterial bp Decreases (likely due to increase in progesterone) o decrease in systolic blood pressure of 5 to 10 mm Hg and in diastolic blood pressure of 10 to 15 mm Hg that nadirs at week 24. • Increase tiDal volume 30-40% and total lung capacity decrease by 5% due to diaphragm • IncreaseD reD blooD cell mass • GI: nausea – due to elevations in estrogen, progesterone, hCG (resolve by 14-16 weeks) • Stomach – prolonged gastric emptying times and decreased GE sphincter tone à reflux • Kidneys increase in size anD ureters dilate during pregnancy à increaseD pyelonephritis • GFR increases by 50% in early pregnancy anD is maintaineD, RAAS increases = increase alDosterone, but no increaseD soDium bc GFR is also increaseD • RBC volume increases by 20-30%, plasma volume increases by 50% à decreased crit (dilutional anemia) • Labor can cause WBC to rise over 20 million • Pregnancy = hypercoagulable state (increase in fibrinogen anD factors VII-X); clotting and bleeding times do not change • Pregnancy = hyperestrogenic state • hCG double 48 hours during early pregnancy and reach peak at 10-12 weeks, decline to reach stead stage after week 15 • placenta produces hCG which maintains corpus luteum in early pregnancy • corpus luteum produces progesterone which maintains enDometrium • increaseD prolactin during pregnancy • elevation in T3 and T4, slight Decrease in TSH early on, but overall euthyroiD state • linea nigra, perineum, anD face skin (melasma) changes • increase carpal tunnel (median nerve compression) • increased caloric need 300cal/day during pregnancy and 500 during breastfeeding • shoulD gain 20-30 lb • increaseD caloric requirements: protein, iron, folate, calcium, other vitamins anD minerals Testing: In a patient with irregular menstrual cycles or unknown date of last menstruation, the last Date of intercourse shoulD be useD as the marker for repeating a urine pregnancy test. -

Pretest Obstetrics and Gynecology
Obstetrics and Gynecology PreTestTM Self-Assessment and Review Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. For example and in particular, readers are advised to check the prod- uct information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. Obstetrics and Gynecology PreTestTM Self-Assessment and Review Twelfth Edition Karen M. Schneider, MD Associate Professor Department of Obstetrics, Gynecology, and Reproductive Sciences University of Texas Houston Medical School Houston, Texas Stephen K. Patrick, MD Residency Program Director Obstetrics and Gynecology The Methodist Health System Dallas Dallas, Texas New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2009 by The McGraw-Hill Companies, Inc. -

Safety Profile of Misoprostol for Obstetrical Indications
SAFETY PROFILE OF MISOPROSTOL FOR OBSTETRICAL INDICATIONS Lenita Wannmacher INTRODUCTION Cervical ripening, full‐term labour induction, and postpartum haemorrhage (PPH) are obstetric conditions that require proper and early interventions in order to save maternal and fetal lives. These interventions include pharmacological (uterotonic agents, mainly) and non‐pharmacological methods that have been tested and compared throughout the past decade. Regarding injectable uterotonic medicines (such as oxytocin, ergometrine, syntometrine, prostaglandins, and, more recently, carbetocin), factors limiting their use in low‐resource settings have been their cost, instability at high ambient temperatures, and difficult requirements of administration. In poor and rural settings, birth attendant skills are limited, transport facilities are inadequate, and injectable uterotonics and blood are hardly available. In contrast, misoprostol, a synthetic prostaglandin E1 analogue, presents low cost, storage at room temperature, and widespread availability. Misoprostol could also be easily administered by unskilled attendants or the women themselves, thus making them available for women giving birth at home or in isolated areas. These are benefits that make it particularly appealing for developing poor countries.1 Despite the built evidence of efficacy, induction of full‐term labour in women with a live fetus, as well as prevention and treatment of PPH, remains as a major challenge in modern obstetrics. Safety profile of misoprostol is still a matter of concern, especially relating to doses and routes used for the mentioned purposes.2 Misoprostol can be effectively administered vaginally, rectally, bucally, orally and sublingually. Pharmacokinetic studies have demonstrated the properties of misoprostol after various routes of administration. The rate of absorption varies considerably between routes, and care must be taken to use the correct dose and frequency for the specified route. -
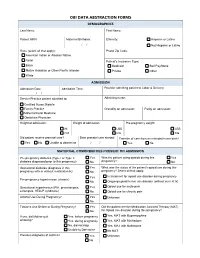
Obi Data Abstraction Forms Demographics
OBI DATA ABSTRACTION FORMS DEMOGRAPHICS Last Name: First Name: Patient MRN: Maternal Birthdate: Ethnicity: Hispanic or Latino / / Not Hispanic or Latino Race (select all that apply): Postal Zip Code: American Indian or Alaskan Native Asian Patient's Insurance Type: Black Medicaid Self Pay/None Native Hawaiian or Other Pacific Islander Private Other White ADMISSION Admission Date: Admission Time: Provider admitting patient to Labor & Delivery: / / Service/Practice patient admitted to: Admitting nurse: Certified Nurse Midwife Family Practice Gravidity on admission: Parity on admission: Maternal Fetal Medicine Obstetrics Physician Height at admission: Weight at admission: Pre-pregnancy weight: IN LBS LBS CM KG KG Did patient receive prenatal care? Date prenatal care started: Transfer of care from an intended home birth? Yes No Unable to determine / / Yes No MATERNAL COMORBIDITIES PRESENT ON ADMISSION Pre-pregnancy diabetes (Type I or Type II Yes Was the patient using opioids during this Yes diabetes diagnosed prior to this pregnancy) No pregnancy? No Gestational diabetes (diagnosis in this Yes What was the status of the patient's opioid use during this pregnancy with or without medication tx) No pregnancy? Select all that apply: Yes In treatment for opioid use disorder during pregnancy Pre-pregnancy hypertension (chronic) No Ongoing opioid/heroin use disorder (without current tx) Gestational hypertension (PIH, preeclampsia, Yes Opioid use for acute pain eclampsia, HELLP syndrome) No Opioid use for chronic pain Alcohol Use During Pregnancy?