Maternity Services Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dumfries & Galloway
Survey Report Dumfries & Galloway 2013 Revised Native Woodland Survey of Scotland Introduction Native woodlands are a vital part of Scotland’s natural and cultural heritage, providing us with a wide range of social, environmental and economic benefits. What is left today is only a small proportion of the native woodland that once covered much of Scotland, though much has been done since the 1980s to protect and restore the areas that remain. The Scottish Forestry Strategy (2006) promotes continuing action to expand our native woods, to improve their condition and to restore native woodland habitats on ancient woodland sites. To support this work Forestry Commission Scotland (FCS) has developed the Native Woodland Survey of Scotland (NWSS), which is the most extensive habitat survey of its kind ever undertaken in Scotland. The survey will provide a nationwide map and a comprehensive picture of our native woodland resource for the first time. Results will be reported separately for each local authority area and in a national summary. This report presents summary information from the Native Woodland Survey of Scotland for the Dumfries and Galloway authority area. Survey Aims The Native Woodland Survey of Scotland will create a woodland map linked to a spatial dataset which describes the type, extent, composition and condition of all native woods in Scotland over 0.5ha in area. Planted woods on ancient woodland sites (PAWS) will also be surveyed, even where they are not mainly native in species composition, in order to provide information to help maintain or restore their remaining biodiversity value. Method The fieldwork for Dumfries and Galloway was carried out between January 2008 and June 2012. -
Report on the Current Position of Poverty and Deprivation in Dumfries and Galloway 2020
Dumfries and Galloway Council Report on the current position of Poverty and Deprivation in Dumfries and Galloway 2020 3 December 2020 1 Contents 1. Introduction 1 2. National Context 2 3. Analysis by the Geographies 5 3.1 Dumfries and Galloway – Geography and Population 5 3.2 Geographies Used for Analysis of Poverty and Deprivation Data 6 4. Overview of Poverty in Dumfries and Galloway 10 4.1 Comparisons with the Crichton Institute Report and Trends over Time 13 5. Poverty at the Local Level 16 5.1 Digital Connectivity 17 5.2 Education and Skills 23 5.3 Employment 29 5.4 Fuel Poverty 44 5.5 Food Poverty 50 5.6 Health and Wellbeing 54 5.7 Housing 57 5.8 Income 67 5.9 Travel and Access to Services 75 5.10 Financial Inclusion 82 5.11 Child Poverty 85 6. Poverty and Protected Characteristics 88 6.1 Age 88 6.2 Disability 91 6.3 Gender Reassignment 93 6.4 Marriage and Civil Partnership 93 6.5 Pregnancy and Maternity 93 6.6 Race 93 6.7 Religion or Belief 101 6.8 Sex 101 6.9 Sexual Orientation 104 6.10 Veterans 105 7. Impact of COVID-19 Pandemic on Poverty in Scotland 107 8. Summary and Conclusions 110 8.1 Overview of Poverty in Dumfries and Galloway 110 8.2 Digital Connectivity 110 8.3 Education and Skills 111 8.4 Employment 111 8.5 Fuel Poverty 112 8.6 Food Poverty 112 8.7 Health and Wellbeing 113 8.8 Housing 113 8.9 Income 113 8.10 Travel and Access to Services 114 8.11 Financial Inclusion 114 8.12 Child Poverty 114 8.13 Change Since 2016 115 8.14 Poverty and Protected Characteristics 116 Appendix 1 – Datazones 117 2 1. -

Sweetheart Abbey and Precinct Walls Statement of Significance
Property in Care (PIC) ID: PIC216 Designations: Scheduled Monument (SM90293) Taken into State care: 1927 (Guardianship) Last reviewed: 2013 STATEMENT OF SIGNIFICANCE SWEETHEART ABBEY AND PRECINCT WALLS We continually revise our Statements of Significance, so they may vary in length, format and level of detail. While every effort is made to keep them up to date, they should not be considered a definitive or final assessment of our properties. Historic Environment Scotland – Scottish Charity No. SC045925 Principal Office: Longmore House, Salisbury Place, Edinburgh EH9 1SH © Historic Environment Scotland 2018 You may re-use this information (excluding logos and images) free of charge in any format or medium, under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit http://nationalarchives.gov.uk/doc/open- government-licence/version/3/ or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned. Any enquiries regarding this document should be sent to us at: Historic Environment Scotland Longmore House Salisbury Place Edinburgh EH9 1SH +44 (0) 131 668 8600 www.historicenvironment.scot You can download this publication from our website at www.historicenvironment.scot Historic Environment Scotland – Scottish Charity No. SC045925 Principal Office: Longmore House, Salisbury Place, Edinburgh EH9 1SH SWEETHEART ABBEY SYNOPSIS Sweetheart Abbey is situated in the village of New Abbey, on the A710 6 miles south of Dumfries. The Cistercian abbey was the last to be set up in Scotland. -

The Beeches Corse Hill, Haugh of Urr, Castle Douglas OFFICES ACROSS SCOTLAND the Beeches Corse Hill, Haugh of Urr Castle Douglas
THE BEECHES CORSE HILL, HAUGH OF URR, CASTLE DOUGLAS OFFICES ACROSS SCOTLAND THE BEECHES CORSE HILL, HAUGH OF URR CASTLE DOUGLAS Castle Douglas 3 miles Dalbeattie 3 miles Dumfries 13 miles. A beautiful architect designed bungalow in an elevated position on the edge of a sought after village. Accommodation on a single level comprises: • Entrance Vestibule. Hallway. Open plan Sitting & Dining Room. Kitchen. Utility Room. • Bedroom /Study. Guest Bedroom. Master Bedroom Suite. Integral Garage. Family Bathroom. • Disabled Access • Security System • Garden CKD Galbraith Castle Douglas Property Department 120 King Street Castle Douglas DG7 1LU Tel: 01556 505346 Fax: 01556 503729 Email: [email protected] Website: www.ckdgalbraith.co.uk GENERAL In addition, Kirkcudbright is the local Artists town The Beeches sits on the edge of the quiet Galloway with a number of galleries offering a range of art village of Haugh of Urr, which is tucked away in exhibitions throughout the year, and individual rolling countryside, yet centrally situated between shops. Communications to the area are very good. two small towns, and within easy reach of the A75 There is a main line railway station in Dumfries and trunk road. From the house itself, circuit walks also Lockerbie providing excellent links to both around the village of either 2 miles or 4 miles can the north and south. The M74 motorway network be enjoyed, and the village has a popular pub is approximately 30 miles distant, and there are which also serves meals. A village primary school is regular flights to other parts of the UK, Ireland and available just up the hill in Hardgate, a neighbouring Continental Europe from Prestwick Airport about hamlet. -
The Lowland Clearances and Improvement in Scotland
University of Massachusetts Amherst ScholarWorks@UMass Amherst Doctoral Dissertations Dissertations and Theses August 2015 Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland Christine B. Anderson University of Massachusetts Amherst Follow this and additional works at: https://scholarworks.umass.edu/dissertations_2 Part of the Archaeological Anthropology Commons Recommended Citation Anderson, Christine B., "Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland" (2015). Doctoral Dissertations. 342. https://doi.org/10.7275/6944753.0 https://scholarworks.umass.edu/dissertations_2/342 This Open Access Dissertation is brought to you for free and open access by the Dissertations and Theses at ScholarWorks@UMass Amherst. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of ScholarWorks@UMass Amherst. For more information, please contact [email protected]. Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland A dissertation presented by CHRISTINE BROUGHTON ANDERSON Submitted to the Graduate School of the University of Massachusetts Amherst in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY May 2015 Anthropology ©Copyright by Christine Broughton Anderson 2015 All Rights Reserved Uncovering and Recovering Cleared Galloway: The Lowland Clearances and Improvement in Scotland A Dissertation Presented By Christine Broughton Anderson Approved as to style and content by: H Martin Wobst, Chair Elizabeth Krause. Member Amy Gazin‐Schwartz, Member Robert Paynter, Member David Glassberg, Member Thomas Leatherman, Department Head, Anthropology DEDICATION To my parents. ACKNOWLEDGEMENTS It is with a sense of melancholy that I write my acknowledgements. Neither my mother nor my father will get to celebrate this accomplishment. -
Dumfries & Galloway
IN BLOOM 2020 DUMFRIES & GALLOWAY GARDENS & NURSERIES visitscotland.com DUMFRIES & GALLOWAY GARDENS & NURSERIES 1 Naturally Inspiring Contents 2 Map & Index 4 Scotland’s Gardens Scheme 7 What’s On From palm fringed coasts in the west and south to rugged 10 Gardens & nurseries moorlands in the north and east, you’ll find a huge variety of 10 Public transport landscapes in this magnificent part of Scotland, as well as a wide Secret Garden at Lime Orchard spectrum of flora and fauna. A wonderful range of gardens and 11 specialist nurseries thrive here too, all run by gardening 12 Logan Botanic Garden enthusiasts who are happy to share their passion and offer advice. 14 Castle Kennedy Gardens Blessed by a mild oceanic climate, as well as free-draining and lime-free 15 Glenwhan Garden, Tearoom & Arboretum soil, Dumfries & Galloway provides the ideal growing conditions for many plant species. Being less exposed to harsh winds and 16 Galloway House Gardens Trust hard frosts means that a diverse range of delicate blooms from the 17 Bayview Nursery southern hemisphere grow happily alongside hardier plants, such as rhododendrons and azaleas. The climate and soils unite with the skills 18 Elmlea Plants and passion of our gardeners to make Galloway a haven for garden 19 Cally Gardens & Nursery enthusiasts, with an unparalleled number of gardens and nurseries waiting for you to explore. Dumfries & Galloway’s spectacular gardens 20 Elizabeth MacGregor’s Nursery at Ellenbank all have their own unique stories to tell. If you’re looking for advice on 21 Drumlanrig Castle and Country Estate which plants to grow in your own garden, the region is home to a wide range of specialist nurseries where you can browse rare and unusual 22 Garden Wise plants, be inspired with ideas and get expert advice from knowledgeable 23 Heathhall Garden Centre staff, discover new plants and arrange for them to be delivered. -

Property and Architectural Services for SALE
Property and Architectural Services Cargen Tower • Garroch Business Park • Garroch Loaning • Dumfries • DG2 8PN • T: 030 33 33 3000 • W: www.dumgal.gov.uk/property FOR SALE DEVELOPMENT OPPORTUNITY FORMER LANGHOLM PRIMARY SCHOOL Thomas Telford Road, Langholm DG13 0BL Offers over £130,000 Close to Langholm Town Centre • Site area 4,034 square metres (0.99 acre) or thereby • Offers over £130,000 Viewing and contact information Andrew Maxwell 01387 273832 Property and Architectural Services [email protected] Dumfries and Galloway Council Cargen Tower Nik Lane 01387 273833 Garroch Business Park [email protected] Garroch Loaning Alastair Johnson 01387 273828 Dumfries [email protected] DG2 8PN www.dumgal.gov.uk/property Accomodation The accommodation is on two levels with a Gross Internal Area of approx. 1,264 square metres 13,606 square feet. Planning The site is identified in the Local Development Plan Location 2- Proposed Plan-Page 168- LMH.H201 Former Primary School, Langholm (10 units allocated to 2029). The Property is situated close to the centre of Langholm within easy reach of Carlisle, located some 20 miles https://www.dumgal.gov.uk/media/19739/LDP2- south along the A7. Hawick is located 23 miles north Proposed-Plan/pdf/PROPOSED_PLAN_JAN_2018. on the A7 and Dumfries 38 miles travelling south along pdf?m=636564441676770000 the A7 and A75. From Langholm Town Centre, turn on Interested parties are advised to contact: to Townhead Bridge and proceed 300 metres along the Thomas Telford Road and the property is located to Development Management -Dumfries Kirkbank your left opposite to the new joint Langholm Primary House, English Street, Dumfries, DG1 2HS and Secondary schools. -

A Landscape Fashioned by Geology
64751 SNH SW Cvr_5mm:cover 14/1/09 10:00 Page 1 Southwest Scotland: A landscape fashioned by geology From south Ayrshire and the Firth of Clyde across Dumfries and Galloway to the Solway Firth and northeastwards into Lanarkshire, a variety of attractive landscapes reflects the contrasts in the underlying rocks. The area’s peaceful, rural tranquillity belies its geological roots, which reveal a 500-million-year history of volcanic eruptions, continents in collision, and immense changes in climate. Vestiges of a long-vanished ocean SOUTHWEST are preserved at Ballantrae and the rolling hills of the Southern Uplands are constructed from the piled-up sediment scraped from an ancient sea floor. Younger rocks show that the Solway shoreline was once tropical, whilst huge sand dunes of an arid desert now underlie Dumfries. Today’s landscape has been created by aeons of uplift, weathering and erosion. Most recently, over the last 2 million years, the scenery of Southwest Scotland was moulded by massive ice sheets which finally melted away about 11,500 years ago. SCOTLAND SOUTHWEST A LANDSCAPE FASHIONED BY GEOLOGY I have a close personal interest in the geology of Southwest Scotland as it gave me my name. It comes of course from the town of Moffat, which is only a contraction of Moor Foot, which nestles near the head of a green valley, surrounded by hills and high moorland. But thank God something so prosaic finds itself in the midst of so SCOTLAND: much geological drama. What this excellent book highlights is that Southwest Scotland is the consequence of an epic collision. -
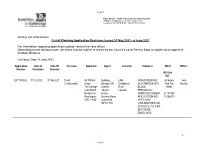
Weekly List of Decisions List of Planning Application Decisions Issued 31 May 2021 - 4 June 2021
PUBLIC Steve Rogers – Head of Economy and Development Kirkbank, English Street, Dumfries, DG1 2HS Telephone (01387) 260199 - Fax (01387) 260188 Weekly List of Decisions List of Planning Application Decisions issued 31 May 2021 - 4 June 2021 For information regarding applications please contact the case officer. Depending on the decision route, decisions may be subject to review by the Council’s Local Review Body or subject to an appeal to Scottish Ministers. List Issue Date: 9 June 2021 Application Date of Date Of Decision Applicant Agent Location Proposal Ward Officer Number Validation Decision OS Grid Ref. 20/1795/FUL 17.12.2020 01.06.2021 Grant Mr Clifford Building Little CONVERSION OF Stranraer Iona Conditionally Howe Design (UK) Cairnbrock ACCOMMODATION And The Brooke The Cottage Limited Ervie BLOCK Rhins Low Street Tayson Leswalt PREVIOUSLY Brotherton House APPROVED UNDER E:197848 Knottingley Methley Road APPLICATION NO. N:566670 WF11 9HQ Castleford 13/P/1/0430 WF10 1PA (IMPLEMENTED ON 21/05/2014) TO 3 NO. DETACHED DWELLINGS 1 PUBLIC PUBLIC Application Date of Date Of Decision Applicant Agent Location Proposal Ward Officer Number Validation Decision OS Grid Ref. 21/0067/FUL 11.03.2021 04.06.2021 Grant Mr Philip WBC Plot 4 ERECTION OF Stranraer Mary Conditionally Harrington Drawings South Cliff DWELLINGHOUSE And The Mitchell Waterside Lockside Portpatrick AND GARAGE Rhins House 38 Leigh Stranraer BUILDING AND Pincock Street DG9 8LE FORMATION OF E:200021 Street Wigan ACCESS N:553886 Euxton WN1 3BE PR7 6LR 21/0844/FUL 26.04.2021 03.06.2021 -

The Killing Times Margaret Mclauchlan Aged 63
PLACES OF INTEREST SOME OTHER COVENANTERS’ SITES IN SOUTHERN SCOTLAND 16 Traquair House NT 330 355 Ayr The Southern and the Minchmuir Road A memorial to seven prisoners from Pentland hanged by The Marquis of Montrose banged on the door of Traquair another prisoner, after the official hangman refused to do so. House in 1645 but was refused admission. He had fled along Wigtown Bay Upland Way the high Minchmuir Road after his Royalist troops had been A stone memorial commemorates two routed by a Covenanting Army at Philiphaugh (NT455 282) women who were drowned for their near Selkirk. faith: Margaret Wilson aged 18, and the killing times Margaret McLauchlan aged 63. 17 Covenanters’ Well NT 535 418 An old well, said to have been frequented by the Covenanters. Kirkcudbright It has now vanished but the spring that once fed the well The churchyard has a memorial to two still issues forth at the site. hanged and beheaded Covenanters. Dumfries HISTORICAL BACKGROUND Troqueer Church: a tablet to Rev. Blackadder who died during imprisonment on the Bass Rock. The Covenanters were Whitesands: a plaque to James Kirko, shot in Dumfries. Scottish Presbyterians who Moniaive objected to English An obelisk to James Renwick, born here in 1662. Episcopalian interference in Tweedsmuir & Moffat their worship. They were Tweedsmuir graveyard contains several graves of martyred called Covenanters because Covenanters. One such victim was John Hunter, who according they supported the National to his tombstone, was ‘cruelly murdered at Core Head by Convenant of 1638, which Col. James Douglas and his party for his adherence to the pledged opposition to the English Bishops. -

Dumfries & Galloway
12 Wildlife Walks Dumfries & Galloway visitdumfriesandgalloway.co.uk Welcome Contents 02 A walk on the wild side 05 VisitScotland Information Centres Scottish Outdoor Access Code 06 The Wig 08 Mull of Galloway 10 The Burnside Trail 12 Cairnsmore of Fleet 12 14 Ken-Dee Marshes 16 Mersehead 11 18 Kirkconnel Flow 20 The Reedbed Ramble 22 Castle Loch 24 Langholm Moorland 26 Moffat 10 28 Baker’s Burn Path 9 5 7 1 4 8 3 Cover Images Front – red squirrel 6 Back – bluebells at Castramon wood Credits Photography: Lorne Gill/SNH, Laurie Campbell/SNH, Glyn Slattery/SNH, George Logan/SNH, John Wright, Cat Barlow, SNH, Mark Pollitt DGERC Design www.stand-united.co.uk www.weesleekit.co.uk 2 VisitScotland has published this guide in good faith to reflect information submitted to it by Scottish Natural Heritage. Although VisitScotland has taken reasonable steps to confirm the information contained in the guide at the time of going to press, it cannot guarantee that the information published is and remains accurate. VisitScotland 1 The Wig 5 Ken-Dee Marshes 9 Castle Loch accepts no responsibility for any error or misrepresentation contained in the guide and excludes all liability for loss or damage caused by any reliance placed on the 2 Mull of Galloway 6 Mersehead 10 Langholm Moorland information contained in the guide. 3 The Burnside Trail 7 Kirkconnel Flow 11 Moffat 4 Cairnsmore of Fleet 8 The Reedbed Ramble 12 Baker’s Burn Path For information and to book accommodation go to visitscotland.com To find out more about Dumfries & Galloway go to visitdumfriesandgalloway.co.uk 01 A walk on the wild side… Dumfries & Galloway is the perfect place to see amazing wildlife in unspoiled, natural habitats and whatever time of year you choose to visit there is always something new and exciting to witness. -

Beautifully Presented Traditional HOUSE in Historic Gatehouse of Fleet Cushat Wood Ann Street, Gatehouse of Fleet, Castle Douglas, Kirkcudbrightshire, Dg7 2Hu
BEAUTIFULLY PRESENTED TRADITIONAL HOUSE IN HISTORIC GATEHOUSE OF FLEET cushat wood ann street, gatehouse of fleet, castle douglas, kirkcudbrightshire, dg7 2hu cushat wood ann street, gatehouse of fleet, castle douglas, kirkcudbrightshire, dg7 2hu Entrance porch w Reception hallway w Morning room w Library/sitting room Drawing room w Dining room w Study w Kitchen/breakfasting room Larder w Utility room w Cloakroom w Master bedroom with en suite bathroom w 3 further bedrooms (1 with en suite) w Family bathroom Lower floor flat w Open plan sitting room and kitchen w Dining area w Bathroom w 2 bedrooms Mature gardens w Hobby room w Greenhouse w Double garage and workshop Situation Cushat Wood is set in the finest position overlooking the town of Gatehouse of Fleet and surrounded by extensive mature gardens, including a walled garden with former tennis court. There are beautiful open aspects to the front, side and rear over the town and the Galloway countryside beyond. Gatehouse of Fleet is a charming Georgian town, widely admired for its historic buildings. It owes its development in the 18th century to the entrepreneur James Murray of Broughton whose mansion, Cally Palace, is now an acclaimed hotel. In Murray’s day, Gatehouse became a thriving centre of water-powered industry and in 1795 had four cotton mills, a brass foundry, a brewery, brickworks, tanneries and a substantial population. Today it is better known for the remarkable beauty of its setting. Gatehouse of Fleet lies within the Fleet Valley National Scenic Area and is surrounded by ancient woods and hills. The mild southwest climate is reflected in the many exotic plants that grow in its gardens.