August 26, 2021 the Honorable Richard Neal Chair, Ways And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dear Massachusetts Congressional Delegation
Honorable Scott Brown Honorable John Kerry 59 Dirksen Senate Office Building 218 Russell Senate Office Building Washington, DC 20510 Washington D.C. 20510 Honorable Michael Capuano Honorable Barney Frank 1414 Longworth House Office Building 2252 Rayburn House Office Building Washington, DC 20515 Washington, DC 20515 Honorable Bill Keating Honorable Stephen Lynch 315 Cannon House Office Building 2348 Rayburn House Office Building Washington, DC 20515 Washington, DC 20515 Honorable Edward Markey Honorable James McGovern 2108 Rayburn House Office Building 438 Cannon House Office Building Washington, DC 20515 Washington, D.C. 20515 Honorable Richard Neal Honorable John Olver 2208 Rayburn House Office Building 1111 Longworth House Office Building Washington, DC 20515 Washington, DC 20515 Honorable John Tierney Honorable Niki Tsongas 2238 Rayburn House Office Building 1607 Longworth House Office Building Washington, DC 20515 Washington, DC 20515 Dear Massachusetts Congressional Delegation, We, the undersigned nonprofit organizations of Massachusetts, are concerned by reports that Congress is considering a cap or elimination of the itemized charitable deduction as part of a deal to avert the fiscal cliff. We urge you to protect this deduction—a unique and cherished incentive for Americans to invest directly in important community needs. The nonprofit sector plays a central role in the social and economic vitality of the Commonwealth of Massachusetts. Our organizations educate and keep the citizenry healthy; care for the most vulnerable populations; and preserve the state’s cherished historical, cultural and environmental resources. Nonprofits employ 16.7% of the workforce, or nearly 500,000 Massachusetts residents, and are responsible for $250 billion in annual revenues. Congress codified the strong American tradition of giving back to our communities in the tax code nearly a century ago, when it provided for deductions on charitable contributions in the Revenue Act of 1917. -

Committee Tax” How the Parties Pressured Legislative Leaders to Raise Huge Sums of Campaign Cash During the 116Th Congress — and Are Poised to Do So Again This Year
New Congress, Same “Committee Tax” How the parties pressured legislative leaders to raise huge sums of campaign cash during the 116th Congress — and are poised to do so again this year By Amisa Ratliff One of the open secrets of Washington is that both the Democratic and Republican parties strong-arm influential legislators to raise astronomical amounts of campaign cash. Referred to as paying “party dues,” lawmakers are pressured to transfer huge sums from their campaigns and affiliated PACs to the parties as well as spend countless hours “dialing for dollars” to raise six- and seven-figure amounts for the parties, often by soliciting corporations, labor unions, and other special interests that have business before Congress. These fundraising demands have morphed into a “committee tax” levied Approximately $1 of by the political parties onto legislators. The more influential the role in every $5 spent during Congress, the more money party leaders expect legislators to raise, with the last election cycle by committee chairs being expected to raise more funds than other members several top Democratic of their caucus. This is especially true for the chairs of the most powerful and Republican committees in the U.S. House of Representatives — the Appropriations, lawmakers were simply Energy and Commerce, Financial Services, and Ways and Means Committees, transfers to the DCCC which are sometimes referred to as “A” committees for their prestige and and NRCC. influence. In fact, according to a new analysis of campaign finance filings by Issue One, approximately $1 of every $5 spent during the 2019-2020 election cycle by several of the top Democratic and Republican lawmakers on these exclusive “A” committees were simply transfers to the Democratic Congressional Campaign Committee (DCCC) and National Republican Congressional Committee (NRCC). -

1 March 11, 2020 the Honorable Richard Neal the Honorable Kevin
March 11, 2020 The Honorable Richard Neal The Honorable Kevin Brady Chairman Ranking Member Committee on Ways and Means Committee on Ways and Means 1102 Longworth House Office Building 1102 Longworth House Office Building Washington, DC 20515 Washington, DC 20515 Dear Chairman Neal and Ranking Member Brady: The Americans for Free Trade Coalition, a broad alliance of American businesses, trade organizations and workers united against tariffs, respectfully submits this written statement to include in the public record of the Ways and Means Committee hearing on U.S.-China Trade and Competition, which took place on February 27, 2020. We appreciate the Committee holding the hearing on this important matter. Our coalition represents every part of the U.S. economy including manufacturers, farmers and agribusinesses, retailers, technology companies, service suppliers, natural gas and oil companies, importers, exporters, and other supply chain stakeholders. Collectively, we support tens of millions of American jobs through our vast supply chains. We agree that our trading partners must abide by global trade rules, but the Administration must also pursue its trade policies in a manner that best serves the American economy. Accordingly, we support the Administration’s efforts to address China’s unfair trading practices, including intellectual property violations, forced technology transfer, market-distorting subsidies, and more. We also appreciate the progress made by the “Phase One” agreement with China and the lifting of a small number of tariffs on Chinese imports. Nevertheless, we object to the unconventional and unpredictable methods the Administration has used – and Congress has allowed – to achieve those goals. The Section 301 tariffs have sown uncertainty in the world’s economy and mistrust with trading partners. -

March 17, 2021 Steve Poftak MBTA General Manager Massachusetts
March 17, 2021 Steve Poftak MBTA General Manager Massachusetts Bay Transportation Authority 10 Park Plaza Boston, MA 02116 Dear Mr. Poftak, We write to follow up on our letter of December 11, 2020 to again express our concerns regarding the MBTA’s Forging Ahead proposal. We have yet to receive a reply to our request for information justifying the level of service cuts the MBTA has implemented. Moreover, since our original letter, Congress has secured over $250 million for the MBTA, and the American Rescue Plan will provide an estimated $1 billion in additional transit funding to the Commonwealth. We urge you to provide evidence that justifies decreased service despite this robust federal relief, as we previously requested, or immediately reverse the recent service cuts, which disproportionately harm essential workers and low-income communities who rely on the MBTA for commutes and access to critical services. We consider mass transit to be a public good, a vital tool for combatting climate change, and an integral part of our post-COVID recovery. As such, we again request that the MBTA provide clear evidence demonstrating the continued need for this degree of service reduction in light of the significant federal assistance the Authority has received. Finally, we hope you can reassure us that the federal assistance Congress has provided will be used to completely restore any and all service cuts as soon as possible. We appreciate your time and attention to this matter and look forward to your prompt response. Sincerely, Katherine M. Clark Elizabeth Warren Member of Congress United States Senator Edward J. -

Summer 2012 Vol 17 • No
You could win something next! something win could You Summer 2012 Vol 17 • No. 2 Connected to the Community contest. Community the to Connected Mighty Red HD Radio Radio HD Red Mighty they won in the last MBA MBA last the in won they displays the the displays IN THIS ISSUE Ray Auger, Auger, Ray Multi Media Director from WMRC-AM in Milford Milford in WMRC-AM from Director Media Multi you” for the entry! the for you” Letter from the Editor We might even send you a little something to say “thank “thank say to something little a you send even might We some of the best entries in future Airwaves newsletters! newsletters! Airwaves future in entries best the of some Political Advertising Rules to share to [email protected]. We’ll feature feature We’ll [email protected]. to share to station success stories along with any photos you want want you photos any with along stories success station Continuing Education still buzzing about? We want to hear from you! Send your your Send you! from hear to want We about? buzzing still Or have you held a wicked cool contest that your station is is station your that contest cool wicked a held you have Or Reimbursement Program you and your team created a brag-worthy charity event? event? charity brag-worthy a created team your and you FROM THE EDITOR Have lately?” to up been station your has “What know, Sound Bites Annual Meeting The Massachusetts Broadcasters Association wants to to wants Association Broadcasters Massachusetts The & Mingling Request AIRWAVES Alec Baldwin’s character in Glengarry Glen Ross is famous for saying, “A-B-C. -

Politicians and Their Professors the Discrepancy Between Climate Science and Climate Policy
Better Future Project 30 Bow Street Cambridge, MA. 02138 Politicians and Their Professors The Discrepancy between Climate Science and Climate Policy By Craig S. Altemose and Hayley Browdy Massachusetts Edition Better Future Project 1 Politicians and Their Professors: The Discrepancy between Climate Science and Climate Policy By Craig Altemose and Hayley Browdy With research and editing assistance provided by Elana Sulakshana, Alli Welton, and Kristen Wraith © 2012, Better Future Project 30 Bow Street, Cambridge, MA 02138 About This Report This report seeks to highlight the discrepancy between the overwhelming consensus on climate change that exists among the nation’s scientific community and the lack of action by federal leaders. Past studies have shown that 97-98% of climate scientists who publish in peer-reviewed journals agree with the consensus that climate change is real, happening now, and man-made. Since many politicians seem to disregard the views of such scientific “elites” as a whole, we decided to compare politicians’ views on climate change to those of the climate experts at their alma maters. These politicians clearly valued the expertise of the academics at their schools enough that they chose to (usually) spend tens of thousands of dollars and up to four years of their lives absorbing knowledge from these institutions’ experts. We thought that even if these politicians choose to disregard the consensus of national experts, they might be persuaded by the consensus of the higher education institutions in which they trusted enough to invest great amounts of their time and money. This report and the research supporting it are available online at www.betterfutureproject.org/resources. -

June 10, 2020 the Honorable Richard Neal the Honorable Kevin Brady
June 10, 2020 The Honorable Richard Neal The Honorable Kevin Brady Chair Ranking Member House Committee on Ways and Means House Committee on Ways and Means Washington, DC 20515 Washington, DC 20515 Dear Chairperson Neal and Ranking Member Brady: On behalf of the American Academy of Family Physicians (AAFP), which represents 136,700 family physicians and medical students across the country, I write to express our appreciation for your interest in issues associated with coronavirus (COVID-19), including your recent hearing titled, “Disproportionate Impact of COVID-19 on Communities of Color.” The AAFP shares your concerns about addressing the factors driving these health disparities and we write to share our policy recommendations. According to the U.S. Centers for Disease Control and Prevention (CDC), there are over 1.9 million cases of COVID-19 and over 100,000 deaths. Higher hospitalization and mortality rates occur among racial and ethnic populations and the CDC indicates that socioeconomic factors have a strong influence on health risks associated with COVID-19. These conditions, which are also known as the social determinants of health (SDoH), predispose individuals to develop chronic health conditions and heighten both infection and mortality risks. Racial and ethnic minorities are likely to live in densely populated settings and reside in communities that are farther away from economic resources and medical facilities. They also are likely to live in multi-generational housing and serve as family caregivers. Compared to other groups, minority groups are overrepresented in environments and are employed where they often encounter the public. They are essential workers yet often lack paid sick leave. -

April 30, 2021 the Honorable Richard Neal Chairman Committee on Ways and Means United States House of Representatives Washingto
April 30, 2021 The Honorable Richard Neal The Honorable Kevin Brady Chairman Ranking Member Committee on Ways and Means Committee on Ways and Means United States House of Representatives United States House of Representatives Washington, DC 20515 Washington, DC 20515 The Honorable Lloyd Doggett The Honorable Devin Nunes Chairman Ranking Member Committee on Ways and Means Committee on Ways and Means Health Subcommittee Health Subcommittee United States House of Representatives United States House of Representatives Washington, DC 20515 Washington, DC 20515 Re: Comments for the Record for the April 28, 2021 Hearing on Charting the Path Forward on Telehealth (submitted to [email protected]) Dear Chairmen Neal and Doggett and Ranking Members Brady and Nunes: On behalf of national organizations representing consumers, family members, mental health and addiction professionals, advocates, payers and other stakeholders, we thank you for your ongoing leadership to advance telehealth both during the COVID-19 Public Health Emergency (PHE) and beyond. As you are well aware, the flexibilities granted by the §1135 emergency telehealth waivers have provided critical stability for healthcare professionals, patients and families across the nation during this challenging time. In particular, telehealth access for mental health and substance use disorder treatment services have served as a lifeline for many Americans struggling with isolation, grief, future uncertainty, and other new stressors this past year. On August 14, 2020, the Centers for Disease Control and Prevention (CDC) reported that rates of substance abuse, anxiety, severe depression, and suicidal ideation increased across many demographics.1 Of grave concern, the report indicated that over 1 in 4 young adults had recently contemplated suicide. -

August 3, 2021 the Honorable Ron Wyden the Honorable Mike Crapo
August 3, 2021 The Honorable Ron Wyden The Honorable Mike Crapo Chairman Ranking Member U.S. Senate Finance Committee U.S. Senate Finance Committee 219 Dirksen SOB 219 Dirksen SOB Washington, DC 20510 Washington, DC 20510 The Honorable Frank Pallone The Honorable Cathy McMorris-Rodgers Chairman Ranking Member U.S. House Energy & Commerce Committee U.S. House Energy & Commerce Committee 2125 Rayburn HOB 2125 Rayburn HOB Washington, DC 20515 Washington, DC 20515 The Honorable Richard Neal The Honorable Kevin Brady Chairman Ranking Member U.S. House Ways & Means Committee U.S. House Ways & Means Committee 1102 Longworth HOB 1102 Longworth HOB Washington, DC 20515 Washington, DC 20515 Re: Mitigate the Medicare Part B Payment Differential for Rehabilitation Therapy Assistants Dear Sens. Wyden and Crapo and Reps. Pallone, McMorris-Rodgers, Neal, and Brady: On behalf of the undersigned, we write to convey our concerns with the implementation of the pending Medicare 15% payment differential for services furnished by physical therapist assistants (PTA) and occupational therapy assistants (OTA) beginning on Jan. 1, 2022. This 15% cut compounds significant payment reductions already imposed on rehabilitation therapy and will have a pervasive and pernicious impact on our patients. The rehabilitation therapy sector is still recovering from the devasting impact of COVID-19 on patients and staff as we continue to provide services during the public health emergency (PHE). Especially early in the pandemic, access to care was curtailed. The AMA reported the early pandemic’s effect on rehab therapy as among the hardest hit among the Medicare Physician Fee Schedule specialties, with up to a 34% drop in spending for services. -

Massachusetts Delegation Calls on NRC to Reject Request to Exempt Pilgrim Nuclear Power St
UNITED STATES OF AMERICA NUCLEAR REGULATORY COMMISSION BEFORE THE NUCLEAR REGULATORY COMMISSION In the Matter of Pilgr im 50-293-EA Entergy’s Request for Extension to Comply With NRC Order EA-13-109, Pilgrim Station September 23, 2016 Pilgrim Watch on behalf of Co-Petitioners requests that the Press Release, Massachusetts Delegation Calls on NRC to Reject Request to Exempt Pilgrim Nuclear Power Station from Safety Upgrades (September 22, 2016) and the delegation’s letter to NRC chairman Stephen Burns, “Exempting Pilgrim from the NRC’s safety requirements would allow Entergy to abdicate that responsibility, unjustifiably exposing Massachusetts communities to danger” be placed in the Pilgrim 50-293-EA docket; and hereby provides notice to all parties. Both the Press Release and letter are attached. Respectfully submitted by Pilgrim Watch on behalf of Co-Petitioners, (Signed (electronically) by, Mary Lampert Pilgrim Watch, Director 148 Washington Street, Duxbury, MA 02332 Tel. 781-934-0389/Email: [email protected] September 23, 2016 ATTACHMENT Massachusetts Delegation Calls on NRC to Reject Request to Exempt Pilgrim Nuclear Power Station from Safety Upgrades Thursday, September 22, 2016 Entergy has requested extension to comply with post-Fukushima safety updates until 2019, the date of closure Washington (September 22, 2016) – The Massachusetts Congressional delegation yesterday sent a letter to the Nuclear Regulatory Commission (NRC) asking it to deny Entergy’s request for an extension for critical safety upgrades to the Pilgrim Nuclear Power Station. When Entergy announced its intention to cease operations at Pilgrim by 2019, the NRC stated that the closure “will not relieve [Entergy] of the responsibility of running that plant as safely as possible until the end of its life.” If approved by NRC, Entergy’s request for extension would run directly counter to that responsibility, as it would increase the risk of a containment failure and a catastrophic radioactive release in the event of a terrorist attack or severe accident. -

GUIDE to the 117Th CONGRESS
GUIDE TO THE 117th CONGRESS Table of Contents Health Professionals Serving in the 117th Congress ................................................................ 2 Congressional Schedule ......................................................................................................... 3 Office of Personnel Management (OPM) 2021 Federal Holidays ............................................. 4 Senate Balance of Power ....................................................................................................... 5 Senate Leadership ................................................................................................................. 6 Senate Committee Leadership ............................................................................................... 7 Senate Health-Related Committee Rosters ............................................................................. 8 House Balance of Power ...................................................................................................... 11 House Committee Leadership .............................................................................................. 12 House Leadership ................................................................................................................ 13 House Health-Related Committee Rosters ............................................................................ 14 Caucus Leadership and Membership .................................................................................... 18 New Members of the 117th -
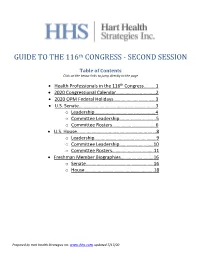
GUIDE to the 116Th CONGRESS
th GUIDE TO THE 116 CONGRESS - SECOND SESSION Table of Contents Click on the below links to jump directly to the page • Health Professionals in the 116th Congress……….1 • 2020 Congressional Calendar.……………………..……2 • 2020 OPM Federal Holidays………………………..……3 • U.S. Senate.……….…….…….…………………………..…...3 o Leadership…...……..…………………….………..4 o Committee Leadership….…..……….………..5 o Committee Rosters……….………………..……6 • U.S. House..……….…….…….…………………………...…...8 o Leadership…...……………………….……………..9 o Committee Leadership……………..….…….10 o Committee Rosters…………..…..……..…….11 • Freshman Member Biographies……….…………..…16 o Senate………………………………..…………..….16 o House……………………………..………..………..18 Prepared by Hart Health Strategies Inc. www.hhs.com, updated 7/17/20 Health Professionals Serving in the 116th Congress The number of healthcare professionals serving in Congress increased for the 116th Congress. Below is a list of Members of Congress and their area of health care. Member of Congress Profession UNITED STATES SENATE Sen. John Barrasso, MD (R-WY) Orthopaedic Surgeon Sen. John Boozman, OD (R-AR) Optometrist Sen. Bill Cassidy, MD (R-LA) Gastroenterologist/Heptalogist Sen. Rand Paul, MD (R-KY) Ophthalmologist HOUSE OF REPRESENTATIVES Rep. Ralph Abraham, MD (R-LA-05)† Family Physician/Veterinarian Rep. Brian Babin, DDS (R-TX-36) Dentist Rep. Karen Bass, PA, MSW (D-CA-37) Nurse/Physician Assistant Rep. Ami Bera, MD (D-CA-07) Internal Medicine Physician Rep. Larry Bucshon, MD (R-IN-08) Cardiothoracic Surgeon Rep. Michael Burgess, MD (R-TX-26) Obstetrician Rep. Buddy Carter, BSPharm (R-GA-01) Pharmacist Rep. Scott DesJarlais, MD (R-TN-04) General Medicine Rep. Neal Dunn, MD (R-FL-02) Urologist Rep. Drew Ferguson, IV, DMD, PC (R-GA-03) Dentist Rep. Paul Gosar, DDS (R-AZ-04) Dentist Rep.