Chapter 3 Thorax
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Part 1 the Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3
ECA1 7/18/06 6:30 PM Page 1 Part 1 The Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3 Surface anatomy and surface markings The experienced clinician spends much of his working life relating the surface anatomy of his patients to their deep structures (Fig. 1; see also Figs. 11 and 22). The following bony prominences can usually be palpated in the living subject (corresponding vertebral levels are given in brackets): •◊◊superior angle of the scapula (T2); •◊◊upper border of the manubrium sterni, the suprasternal notch (T2/3); •◊◊spine of the scapula (T3); •◊◊sternal angle (of Louis) — the transverse ridge at the manubrio-sternal junction (T4/5); •◊◊inferior angle of scapula (T8); •◊◊xiphisternal joint (T9); •◊◊lowest part of costal margin—10th rib (the subcostal line passes through L3). Note from Fig. 1 that the manubrium corresponds to the 3rd and 4th thoracic vertebrae and overlies the aortic arch, and that the sternum corre- sponds to the 5th to 8th vertebrae and neatly overlies the heart. Since the 1st and 12th ribs are difficult to feel, the ribs should be enu- merated from the 2nd costal cartilage, which articulates with the sternum at the angle of Louis. The spinous processes of all the thoracic vertebrae can be palpated in the midline posteriorly, but it should be remembered that the first spinous process that can be felt is that of C7 (the vertebra prominens). The position of the nipple varies considerably in the female, but in the male it usually lies in the 4th intercostal space about 4in (10cm) from the midline. -

Slipping Rib Syndrome
Slipping Rib Syndrome Jackie Dozier, BS Edited by Lisa E McMahon, MD FACS FAAP David M Notrica, MD FACS FAAP Case Presentation AA is a 12 year old female who presented with a 7 month history of right-sided chest/rib pain. She states that the pain was not preceded by trauma and she had never experienced pain like this before. She has been seen in the past by her pediatrician, chiropractor, and sports medicine physician for her pain. In May 2012, she was seen in the ER after having manipulations done on her ribs by a sports medicine physician. Pain at that time was constant throughout the day and kept her from sleeping. However, it was relieved with hydrocodone/acetaminophen in the ER. Case Presentation Over the following months, the pain became progressively worse and then constant. She also developed shortness of breath. She is a swimmer and says she has had difficulty practicing due to the pain and SOB. AA was seen by a pediatric surgeon and scheduled for an interventional pain management service consult for a test injection. Following good temporary relief by local injection, she was scheduled costal cartilage removal to treat her pain. What is Slipping Rib Syndrome? •Slipping Rib Syndrome (SRS) is caused by hypermobility of the anterior ends of the false rib costal cartilages, which leads to slipping of the affected rib under the superior adjacent rib. •SRS an lead to irritation of the intercostal nerve or strain of the muscles surrounding the rib. •SRS is often misdiagnosed and can lead to months or years of unresolved abdominal and/or thoracic pain. -

Structure of the Human Body
STRUCTURE OF THE HUMAN BODY Vertebral Levels 2011 - 2012 Landmarks and internal structures found at various vertebral levels. Vertebral Landmark Internal Significance Level • Bifurcation of common carotid artery. C3 Hyoid bone Superior border of thyroid C4 cartilage • Larynx ends; trachea begins • Pharynx ends; esophagus begins • Inferior thyroid A crosses posterior to carotid sheath. • Middle cervical sympathetic ganglion C6 Cricoid cartilage behind inf. thyroid a. • Inferior laryngeal nerve enters the larynx. • Vertebral a. enters the transverse. Foramen of C 6. • Thoracic duct reaches its greatest height C7 Vertebra prominens • Isthmus of thyroid gland Sternoclavicular joint (it is a • Highest point of apex of lung. T1 finger's breadth below the bismuth of the thyroid gland T1-2 Superior angle of the scapula T2 Jugular notch T3 Base of spine of scapula • Division between superior and inferior mediastinum • Ascending aorta ends T4 Sternal angle (of Louis) • Arch of aorta begins & ends. • Trachea ends; primary bronchi begin • Heart T5-9 Body of sternum T7 Inferior angle of scapula • Inferior vena cava passes through T8 diaphragm T9 Xiphisternal junction • Costal slips of diaphragm T9-L3 Costal margin • Esophagus through diaphragm T10 • Aorta through diaphragm • Thoracic duct through diaphragm T12 • Azygos V. through diaphragm • Pyloris of stomach immediately above and to the right of the midline. • Duodenojejunal flexure to the left of midline and immediately below it Tran pyloric plane: Found at the • Pancreas on a line with it L1 midpoint between the jugular • Origin of Superior Mesenteric artery notch and the pubic symphysis • Hilum of kidneys: left is above and right is below. • Celiac a. -

1 the Thoracic Wall I
AAA_C01 12/13/05 10:29 Page 8 1 The thoracic wall I Thoracic outlet (inlet) First rib Clavicle Suprasternal notch Manubrium 5 Third rib 1 2 Body of sternum Intercostal 4 space Xiphisternum Scalenus anterior Brachial Cervical Costal cartilage plexus rib Costal margin 3 Subclavian 1 Costochondral joint Floating ribs artery 2 Sternocostal joint Fig.1.3 3 Interchondral joint Bilateral cervical ribs. 4 Xiphisternal joint 5 Manubriosternal joint On the right side the brachial plexus (angle of Louis) is shown arching over the rib and stretching its lowest trunk Fig.1.1 The thoracic cage. The outlet (inlet) of the thorax is outlined Transverse process with facet for rib tubercle Demifacet for head of rib Head Neck Costovertebral T5 joint T6 Facet for Tubercle vertebral body Costotransverse joint Sternocostal joint Shaft 6th Angle rib Costochondral Subcostal groove joint Fig.1.2 Fig.1.4 A typical rib Joints of the thoracic cage 8 The thorax The thoracic wall I AAA_C01 12/13/05 10:29 Page 9 The thoracic cage Costal cartilages The thoracic cage is formed by the sternum and costal cartilages These are bars of hyaline cartilage which connect the upper in front, the vertebral column behind and the ribs and intercostal seven ribs directly to the sternum and the 8th, 9th and 10th ribs spaces laterally. to the cartilage immediately above. It is separated from the abdominal cavity by the diaphragm and communicates superiorly with the root of the neck through Joints of the thoracic cage (Figs 1.1 and 1.4) the thoracic inlet (Fig. -

Subcostal TAP, Rectus Sheath
Station 4: Traditional Transversus Abdominis Plane (TAP), Subcostal TAP, Rectus Sheath Station Faculty: Traditional TAP: Adam Amundson, MD David Olsen, MD Indications: o Surgeries that involve the lower abdominal segment (below umbilicus) ie: Pfannenstiel incision for cesarean-section. Ultrasound settings and Patient Position o High Frequency linear probe; Low Frequency linear probe if morbidly obese (38-50 mm footprint) o Supine, arms to sides, performed with patient either sedated or under general anesthesia Surface Anatomy landmarks o Rib cage, costal margin o Iliac Crest, pelvic brim o Mid-axillary line Sonoanatomy – o Start by placing the ultrasound probe between the iliac crest and costal margin at the mid-axillary line o Identify the 3 muscular layers (external oblique EO, internal oblique IO, transversus abdominis TA) and the peritoneum o TIPS: EO is generally hyperechoic, IO is the largest, TA is thin, Bowel/Peritoneum may move EO EO IO IO Superior Superior TA TA Bowel Bowel Suggested Injection Technique- TA o In-plane short axis approach, sonographically guide a 21 g 4 inch needle in between the fascial plane of the IO and TA in the posterior corner (see white arrow below). o Inject 20 mL of dilute long acting local anesthetic per side, or 30 mL if unilateral EO EO IO IO Superior Superior TA Bowel Bowel Bowel o TIP: When entering fascial planes between IO and TA the needle tip is often positioned deep and you may need to slowly pull the needle back while giving small aliquots of fluid to help define the spread of the fascial planes. -
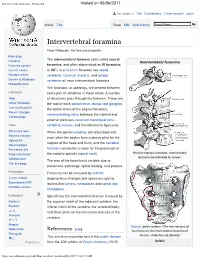
Intervertebral Foramina - Wikipedia Visited on 06/06/2017
Intervertebral foramina - Wikipedia Visited on 06/06/2017 Not logged in Talk Contributions Create account Log in Article Talk Read Edit View history Intervertebral foramina From Wikipedia, the free encyclopedia Main page The intervertebral foramen (also called neural Contents Intervertebral foramina Featured content foramina, and often abbreviated as IV foramina Current events or IVF), is a foramen between two spinal Random article vertebrae. Cervical, thoracic, and lumbar Donate to Wikipedia vertebrae all have intervertebral foramina. Wikipedia store The foramina, or openings, are present between Interaction every pair of vertebrae in these areas. A number Help of structures pass through the foramen. These are About Wikipedia the root of each spinal nerve, dorsal root ganglion, Community portal the spinal artery of the segmental artery, Recent changes communicating veins between the internal and Contact page external plexuses, recurrent meningeal (sinu- Tools vertebral) nerves, and transforaminal ligaments. What links here When the spinal vertebrae are articulated with Related changes each other the bodies form a strong pillar for the Upload file support of the head and trunk, and the vertebral Special pages Permanent link foramen constitutes a canal for the protection of Page information the medulla spinalis (spinal cord). Peculiar thoracic vertebrae. Intervertebral foramina are indicated by arrows. Wikidata item The size of the foramina is variable due to Cite this page placement, pathology, spinal loading, and posture. Print/export Foramina can be occluded by arthritic Create a book degenerative changes and space-occupying Download as PDF lesions like tumors, metastases and spinal disc Printable version herniations. Languages Specifically the intervertebral foramen is bound by Deutsch the superior notch of the adjacent vertebra, the Español inferior notch of the vertebra, the vertebral body, and facet joints on the transverse process of the فارسی Français vertebra. -

Bones, Part 1: the Axial Skeleton
PowerPoint® Lecture Slides The Skeleton prepared by Leslie Hendon University of Alabama, Birmingham • Consists of: • Bones, cartilage, joints, and ligaments Composed of 206 named bones grouped into C H A P T E R • 7 two divisions Part 1 • Axial skeleton (80 bones) Bones, Part 1: • Appendicular skeleton (126 bones) The Axial Skeleton Copyright © 2011 Pearson Education, Inc. Copyright © 2011 Pearson Education, Inc. The Axial Skeleton(in green) The Axial Skeleton Cranium Skull Cranium Facial bones Bones of Clavicle pectoral Clavicle girdle • Formed from 80 Thoracic cage Scapula (ribs and Scapula Sternum sternum) Upper named bones Rib limb Humerus Rib Humerus Vertebra • Consists of skull, Vertebral Vertebra Radius column Radius Ulna Ulna vertebral column, Sacrum Carpals Bones of and bony thorax pelvic girdle Carpals Phalanges Phalanges Metacarpals Metacarpals Femur Femur Patella Lower Tibia limb Tibia Fibula Fibula Tarsals Metatarsals (a) Anterior view Phalanges (b) Posterior view Copyright © 2011 Pearson Education, Inc. Figure 7.1a Copyright © 2011 Pearson Education, Inc. Figure 7.1b The Skull The Cranium • Formed by cranial and facial bones • Is the body’s most complex bony structure Frontal bone Parietal bone Glabella • Formed by cranial and facial bones Squamous part Frontonasal suture of frontal bone Supraorbital foramen Nasal bone (notch) • The cranium Sphenoid bone Supraorbital margin (greater wing) Superior orbital fissure • Encloses and protects brain Temporal bone Optic canal Ethmoid bone Inferior orbital fissure Lacrimal bone • Provides attachment for head and neck Zygomatic bone Middle nasal concha muscles Infraorbital foramen Ethmoid Perpendicular plate bone Maxilla Inferior nasal concha Vomer Mandible Mental foramen Mental protuberance (a) Anterior view of skull Copyright © 2011 Pearson Education, Inc. -
Disorders of the Thoracic Cage and Abdomen
Disorders of the thoracic cage and abdomen CHAPTER CONTENTS Heart (Fig. 1) Referred pain e185 Pain referred from visceral structures . e185 Ischaemic heart disease Pain referred from musculoskeletal structures not The innervation of the heart is derived from the C8–T4 seg- belonging to the thoracic cage . e191 ments. Pain is therefore not only felt in the chest but can also Disorders of the thoracic cage and abdomen e191 be referred to the ulnar side of both upper limbs, though more commonly to the left. Disorders of the inert structures . e191 It is traditionally accepted that pain felt in the chest radiat- Disorders of the contractile structures . e193 ing into the left arm is indicative of myocardial ischaemia, especially when the patient reports it as pressure, constriction, squeezing or tightness. However, none of these descriptions, which are usually regarded as characteristic of ischaemia, is of Pain in the thorax or abdomen can be the result of a local definitive aid in the differential diagnosis from other non- problem of either the thoracic wall or the abdominal muscles cardiogenic problems in the thorax. Even relief of pain after but it is more often referred from a visceral structure or the intake of glyceryl trinitrate does not offer absolute confir- from another musculoskeletal source, most frequently a disc mation of coronary ischaemia. For clinical diagnosis, a combina- protrusion. Therefore, it is wise to remember the only safe tion of several elements must be present, of which the most approach in this area is to achieve a diagnosis by both positive important is pain spreading to both arms and shoulders initi- confirmation of the lesion and exclusion of other possible ated by walking, especially after heavy meals or on cold days.1 disorders. -

Anatomy for the Laparoscopic Surgeon
Anatomy for the laparoscopic surgeon Laparoscopic surgery is a safe and effective option for many patients, provided the surgeon knows the relevant anatomic landmarks and variations created by obesity, prior surgery, and aberrant anatomy. Here’s a primer on minimizing patient morbidity and optimizing outcomes. Emad Mikhail, MD, Lauren Scott, MD, and Stuart Hart, MD, MS CASE Obese patient requests total laparo- enlarged uterus of approximately 14 weeks’ scopic hysterectomy size with minimal descensus. An earlier trial A 45-year-old woman (G2P2), who delivered of hormone therapy failed to provide relief. both children by cesarean section, schedules After you counsel her extensively about her an office visit for a complaint of abnormal treatment options, she elects to undergo uterine bleeding. She is obese, with a body total laparoscopic hysterectomy. mass index (BMI) of 35 kg/m2, and has an What anatomy would you review to help ensure the procedure’s success? IN THIS ARTICLE Dr. Mikhail is Assistant Professor, Department of Obstetrics and lthough the vaginal route is preferred Surface anatomy Gynecology, University of South for hysterectomy, total laparoscopic of anterior Florida Morsani College of hysterectomy is another minimally Medicine (MCM), Tampa, Florida. A abdominal wall invasive option that offers lower morbidity page 50 and a shorter hospital stay than the abdomi- nal approach.1 Perhaps more than any other Dr. Scott is Fellow, Division of Vascular anatomy variable, the key to safe, efficient, and effec- Female Pelvic Medicine and of anterior Reconstructive Surgery, Department tive laparoscopic surgery is a comprehensive of Obstetrics and Gynecology, abdominal wall University of South Florida MCM. -
Structure of the Thoracic Wall
human anatomy 2016 lecture eleven Dr meethak ali ahmed neurosurgeon opening of the thorax The thoracic cavity communicates with the root of the neck through an opening called the thoracic inlet ; is bounded post. by first thoracic vertebra, laterally by the medial border of the first ribs & their costal cartilage , & ant. by the superior border of the manubrium sterni. the opening is obliquely placed facing upward & forward . Through this small opening pass the esophagus &trachea and many vessels & nerve . because of the obliquely of the opening ,the apices of the lung and pleurae project upward into the neck. The thoracic cavity communicates with abdomen through a large opening called the thoracic outlet . The opening is bounded post. by the twelfth thoracic vertebrae , laterally by the curving costal margin ,& ant. by xiphisternal joint . Through this large opening , which is closed by the diaphragm ,pass the esophagus & many large vessels & nerve ,all which pierce the diaphragm. structure of the thoracic wall The thoracic wall is coverd on the outside by skin & by muscles attaching the shoulder girdle to the trunk. lined with parietal pleura . thoracic part of the vertebral column is concave forward & is made up of twelve vertebrae , together with their intervertebral disc. sternum the sternum is flat bone that may be divided into three parts reference, snell clinical anatomy human anatomy 2016 lecture eleven Dr meethak ali ahmed neurosurgeon manubrium; is the upper part of the sternum ,& it articulates with the clavical & the first & upper part of the second costal cartilages on each side . it opposite the third and fourth thoracic vertebrae. -

Internal Fixation of Posterior Pelvic Ring Injuries Using Iliosacral Screws in the Dysmorphic Upper Sacrum
Internal Fixation of Posterior Pelvic Ring Injuries Using Iliosacral Screws in the Dysmorphic Upper Sacrum Saam Morshed, MD, PhD, MPH, Kevin Choo, MD, Utku Kandemir, MD, and Scott Patrick Kaiser, MD Based on an original article: J Bone Surg Am. 2014 Jul 16;96(14):e120. Introduction The surgical procedure starts with appropriate supine positioning and verification of adequate fluoro- The correct usage of preoperative and intraoperative im- scopic inlet, outlet, and lateral sacral views. The coronal aging allows fixation of posterior pelvic ring injuries with and axial angulation measured during preoperative plan- safely positioned iliosacral screws in the setting of sacral ning can then be used to determine the best insertion dysmorphism. site and trajectory of the iliosacral screw. Reduction of Percutaneous treatment of unstable pelvic ring the fracture is enabled by positioning with a longitudinal injuries is a technically demanding procedure with a steep central bump underneath the sacrum. Careful assess- learning curve. An in-depth understanding of pelvic os- ment of the trajectory of the guidewire and drill on outlet, seous, vascular, and neural anatomy is vital to prevent inlet, and lateral sacral fluoroscopic views is necessary serious complications. The surgeon must feel comfortable to ensure an intraosseous trajectory of each iliosacral translating difficult fluoroscopic imaging into a three-dimen- screw12,13. Alternatively, surgical navigation, which allows sional spatial visualization to attain reduction and establish real-time visualization of screw placement without radia- an effective and safe screw trajectory. Even surgeons tion, can be used when combined with intraoperative CT experienced in the use of percutaneous iliosacral screws for registration; however, the same principles regarding must be ready to adjust their technique when confronted accurate screw placement apply (see Clinical Comments with a dysmorphic anatomic phenotype (Video 1). -

Thoracic Rib Cage Lesions Caused by Thiamin Deficiency - Etiology and Physiologic Therapy of Tietze’S Syndrome
Open Access Annals of Nutritional Disorders & Therapy Case Report Thoracic Rib Cage Lesions Caused by Thiamin Deficiency - Etiology and Physiologic Therapy of Tietze’s Syndrome Lee BY1* and Bai JH2 1DepartmentBiochemical Genetics/Pediatrics, Louisiana Abstract State University Health Sciences Center in Shreveport, This paper describes abnormalities of the thoracic rib cage observed in a USA huge labor farm, where every laborer should work terribly hard with inadequate 2Department of Epidemiology, Texas A & M University, food for several years. The lesions involved the the sternum and its surrounding USA rib cartilages articulated with it. A horizontal ridge developed at the sternal *Corresponding author: Benjamin Yuehtung angle; xiphoid processor could be very painful and disfiguring; the costal margin Lee, Department of Biochemical Genetics/Pediatrics, might become opening to the lateral sides and upward. Louisiana State University Health Sciences Center in Twenty-five cases of costochondritis with swelling had been observed Shreveport, 1501 Kings Hwy, Shreveport, LA 71130, USA within 4 years and cured with small dose of thiamin by local infusion because Received: May 07, 2019; Accepted: June 10, 2019; of medicine under supply. The dramatic therapeutic response confirmed that Published: June 17, 2019 thiamin deficiency is the etiology of Tietze’ s syndrome, which was found worldwide only 159 case within 35 years as reported in 1956, and another worldwide 131 cases were added 1955-1960. Keywords: Costochondritis; Costal margin; Rib cage; Sternal angle; Sternum; Thiamine deficiency; Tietze’s syndrome; Xiphoid processor Case Presentation C. Slightly opened costal margins: In a few cases, the two costal margins on both sides opened slightly wider to both lateral Human thoracic rib cage contains and protects lungs, heart and directions and slightly bent upward at their thicker edges.