Pittsburgh, PA 15213 412-623-2345
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Local Houses of Worship Local H
Local Houses of Worship Local Houses of Worship Compliments of UPMC Presbyterian Office of Spiritual Care, Compliments of UPMC Presbyterian Office of Spiritual Care, 412-647-7560 412-647-7560 Downtown Monroeville Chabad at Pitt Friends Meeting House Downtown Monroeville Chabad at Pitt Friends Meeting House 215 Lytton Ave. (Quaker) 215 Lytton Ave. (Quaker) Beth Hamedrash Hagodol/ (outside of city) Beth Hamedrash Hagodol/ (outside of city) 443-525-4212 4836 Ellsworth Ave. 443-525-4212 4836 Ellsworth Ave. Beth Jacob Congregation Beth Jacob Congregation Chabad Jewish Center www.chabadpgh.org 412-683-2669 Chabad Jewish Center www.chabadpgh.org 412-683-2669 (Jewish Orthodox) (Jewish Orthodox) of Monroeville www.quaker.org/legacy/ of Monroeville www.quaker.org/legacy/ 810 5th Ave. 810 5th Ave. (Jewish Hassidic) Church of the Ascension pghpamm (Jewish Hassidic) Church of the Ascension pghpamm 412-471-4443 2715 Mosside Blvd. (ACNA) 412-471-4443 2715 Mosside Blvd. (ACNA) 412-372-1000 4729 N. Ellsworth Ave. Heinz Memorial Chapel 412-372-1000 4729 N. Ellsworth Ave. Heinz Memorial Chapel Trinity Episcopal Cathedral Trinity Episcopal Cathedral www.jewishmonroeville.com 412-621-4361 (non-denominational) www.jewishmonroeville.com 412-621-4361 (non-denominational) 328 Sixth Ave. 328 Sixth Ave. www.Ascensionpgh.org Bellefield Ave. www.Ascensionpgh.org Bellefield Ave. 412-232-6404 412-232-6404 Christ’s Church Ministries between Forbes and Fifth Christ’s Church Ministries between Forbes and Fifth www.trinitycathedralpgh.org www.trinitycathedralpgh.org (Hebraic Christian Fellowship) Church of Christ 412-624-4156 (Hebraic Christian Fellowship) Church of Christ 412-624-4156 1622 James St. (non-denominational) www.heinzchapel.pitt.edu 1622 James St. -
General Orientation Handbook 2019
GENERAL ORIENTATION HANDBOOK 2019 -Table of Contents- UPMC Horizon: Organizational Review • Business Unit Mission/Vision/Values • AIDET Plus the Promise • UPMC Horizon Senior Leadership Team Organizational Goals Ethics & Code of Conduct • Human Resources Performance Management License/Certification/Registration & Required Clearances (if applicable) Orientation Period Drug Free Workplace Clean Air/Smoke Free Attendance Guidelines Corrective Action & Discharge Grievance Policy Harassment Employee Rights Equal Employment & Non-Discrimination Fair Labor Standard Act LifeSolutions • Employee Health/MyHealth@ Work Worker’s Compensation Work Related Injuries/Illness Environment of Care • Safety Management Safety Officer Safety Management Plan • Security Management Reporting Security Issues Door Access/Sensitive Areas Workplace Violence • Fire Safety & Response/Life Safety • Medical Equipment/Electrical Safety Safe Medical Device Act • Utility Systems • Emergency Preparedness/Disaster Management Code/Condition Definitions • Hazardous Materials/Waste Management Spill Response • Radiation Safety Infection Prevention & Control • OSHA Bloodborne Pathogens • Employee Health Services • Tuberculosis • Hand Hygiene • PPE/Standard & Isolation Precautions Patient Rights and Safety • Reporting Patient Incidences • MCARE • National Patient Safety Goals • Sentinel Events • Abuse & Neglect • New Born Protection/Safe Haven Program • Fall Prevention • Restraints • Privacy & Security • HIPAA/Confidentiality • Patient Rights & Responsibilities • Organizational -

UPMC Sports Medicine Concussion Program Fellowship Opportunities
UPMC Sports Medicine Concussion Program Fellowship Opportunities Established in 2000, the UPMC Sports Medicine Concussion Program has grown to include seven attending clinical neuropsychologists who work within a multidisciplinary team to assess, diagnose, and treat concussions. This team includes primary care sports medicine, physical medicine and rehabilitation, neurovestibular rehabilitation, neurosurgery, neuro-radiology, behavioral neuro-optometry, and physical therapy, including both musculoskeletal evaluations and sport-specific exertion therapy. In addition to this primary location, there are currently five satellite clinics located throughout the Greater Pittsburgh area including UPMC Lemieux Sports Complex in Cranberry, UPMC Monroeville, UPMC Bethel Park, UPMC Children’s Hospital of Pittsburgh at Pine Township, and UPMC Children’s Hospital of Pittsburgh South in Bridgeville. Clinical Training Model Fellows begin with a one month training intensive working closely with Dr. Collins. Alongside current fellows, new fellows will learn competence with the clinical interview, administration of the vestibular/ocular-motor screening (VOMS), and interpretation of Under the guidance of Michael “Micky” Collins, PhD, clinical computer-based neurocognitive testing, as well as more traditional and executive director, the UPMC Sports Medicine Concussion neuro-psychological evaluation tools. After the first month, fellows Program sees over 17,000 patient visits, involving between will enter into the regular clinical rotation, in which they will work 6,000-7,000 unique patients, each year. The clinical team is in some capacity with all faculty members and rotate amongst involved in the evaluation and management of concussions for the satellite clinics. Fellow offices are located at the UPMC Rooney athletes at all levels of sports participation, including professional, Sports Complex, where all fellows have access to a computer, collegiate, high school, and youth athletes. -

John Innocenti President UPMC Presbyterian Shadyside 200 Lothrop Street - MUH N739 Pittsburgh, PA 15213 Phone: 412-647-5286 [email protected]
John Innocenti President UPMC Presbyterian Shadyside 200 Lothrop Street - MUH N739 Pittsburgh, PA 15213 Phone: 412-647-5286 [email protected] John Innocenti is the President of UPMC Presbyterian Shadyside Hospital, the flagship of the UPMC System, which comprises 16 hospitals in the Western Pennsylvania area. UPMC Presbyterian Shadyside, which includes UPMC Presbyterian, UPMC Shadyside, UPMC Montefiore, UPMC Eye & Ear Institute and Western Psychiatric Institute and Clinic, is located in the Oakland district of Pittsburgh, and comprises over 1200 MedSurg beds, 220 ICU Beds and 310 psychiatric beds. It is also a Level I Trauma Center, and houses the Thomas Starzl Transplant Institute, which comprises one of the nation’s largest transplant programs. The Shadyside campus includes the Hillman Cancer Center and the Posner Pavilion. Mr. Innocenti has both an Industrial Engineering Degree and MBA from the University of Pittsburgh. He is a member of various boards, including the UPMC Monroeville Surgery Center, Family House, as well as the President of the South Park School Board. Mr. Innocenti was the recipient of the University of Pittsburgh 2005 Distinguished Alumni Award from Industrial Engineering, was named the 2011 Corporate Gift of Life Awardee by the National Kidney Foundation, and the 2013 Arthritis Foundation honoree. Mr. Innocenti was at the University Hospitals of Cleveland, as well as several years of consulting prior to joining Montefiore Hospital in 1976. Montefiore Hospital merged with UPMC in 1990, and Mr. Innocenti has varying levels of administrative responsibilities in his 30 years with the Health System. Mr. Innocenti is also an Adjunct faculty member at the University of Pittsburgh, and has taught management courses for over twenty years. -

UPMC INFUSION SERVICES Why Choose UPMC Infusion Services?
UPMC INFUSION SERVICES Why Choose UPMC Infusion Services? Locations Near You Therapy times vary based on the treatment. All therapies must be ordered by a UPMC physician. Services are offered throughout the week at multiple locations. To schedule an appointment at a UPMC Outpatient Infusion Center, please contact that individual facility. For more information visit UPMC.com/InfusionCenter. CENTRAL NOrtH Magee-Womens Hospital of UPMC Hamot UPMC Infusion Center 215 Holland St. 300 Halket St., Suite 5600 Erie, PA 16507 Pittsburgh, PA 15203 814-877-6600 412-641-3615 M-F, 7 a.m. to 6:30 p.m. M-F, 7 a.m. to 5 p.m. UPMC Horizon – UPMC Mercy – Southside Greenville 2000 Mary St. 110 N. Main St. Pittsburgh, PA 15203 Greenville, PA 16125 UPMC Infusion Services offers outpatient infusion services 412-488-5290 724-589-6842 M-F, 7 a.m. to 3:30 p.m. M-F, 7 a.m. to 3:30 p.m. to provide patients with a safe and comfortable outpatient setting to receive infusion therapy. UPMC Presbyterian UPMC Horizon – 200 Lothrop St. Shenango Our outpatient infusion centers are staffed by a highly Pittsburgh, PA 2200 Memorial Dr. experienced team of physicians and registered nurses. 412-647-9608 Farrell, PA 16121 Our staff works with referring physicians to provide quality, M-F, 6:30a.m. to 6p.m. 724-983-7021 M-F, 7 a.m. to 3:30 p.m. personalized infusion care to ensure the patient maintains a UPMC Shadyside normal routine with appointments available at convenient 5230 Centre Ave., Fifth Floor UPMC Northwest times as part of an overall continuum of care. -

Shadyside Hospital
Project Area Master Plan 2014 OAKLAND HOSPITALS 200 Lothrop, Pittsburgh, PA 15213 Submission Date: 11/24/2014 Oakland Hospitals Project Area Master Plan 11/24/2014 TABLE OF CONTENTS I. Master Plan II. Planning Area III. Mission and Objectives IV. Existing Property and Uses V. Institutional Needs VI. Ten Year Development Envelope VII. Twenty-Five Year Development Envelope VIII. Transportation Management Plan IX. Environmental Protection Plan X. Open Space and Pedestrian Circulation Plan XI. Urban Design Guidelines XII. Neighborhood Protection Strategy HARLEY ELLIS DEVEREAUX/Trans Associates 2 Oakland Hospitals Project Area Master Plan 11/24/2014 I. MASTER PLAN Introduction UPMC Presbyterian and Montefiore Hospitals (Oakland), located in the heart of Emergency and Trauma Services Oakland, is an adult medical-surgical referral hospital group and a site of ongoing Endocrine Surgery research and graduate programs in conjunction with the University of Pittsburgh Eye Center School of Medicine. The hospital is a renowned center for organ transplantation, Gastrointestinal Surgery and a recognized leader in cardiology and cardiothoracic surgery, critical care medicine and trauma services, and neurosurgery. UPMC Oakland also is Geriatrics designated as a Level I Regional Resource Trauma Center. Founded in 1893, Inflammatory Bowel Disease UPMC Oakland continues to provide state-of-the-art medical care to patients in the Kidney Disease tri-state area and throughout the world. Liver Cancer Center Minimally Invasive Brain Surgery UPMC Oakland is one hospital with two buildings - UPMC Presbyterian and UPMC Neurological Surgery Montefiore - linked by a pedestrian bridge that crosses over two streets with links to other buildings as well. Staff in both buildings deliver the same high-quality care. -

Return of Organization Exempt from Income
l efile GRAPHIC p rint - DO NOT PROCESS As Filed Data - DLN: 93490135008019 Return of Organization Exempt From Income Tax OMB No 1545-0047 Form 990 Under section 501 (c), 527, or 4947( a)(1) of the Internal Revenue Code ( except black lung benefit trust or private foundation) 2 00 7_ Department of the Open -The organization may have to use a copy of this return to satisfy state reporting requirements Treasury Inspection Internal Revenue Service A For the 2007 calendar year, or tax year beginning 07 -01-2007 and ending 06 -30-2008 C Name of organization D Employer identification number B Check if applicable Please UPMC GROUP 1 Address change use IRS 20-8295721 label or Number and street (or P 0 box if mail is not delivered to street address ) Room/ suite E Telephone number F Name change print or type . See 600 GRANT STREET 58TH FLOOR (412) 647-8762 1 Initial return Specific C /O CORPORATE TAX DEPARTMENT Instruc - City or town, state or country , and ZIP + 4 FAccounting method fl Cash F Accrual F_ Final return tions . PITTSBURGH, PA 15219 (- Other ( specify) 0- (- Amended return (Application pending * Section 501(c)(3) organizations and 4947(a)(1) nonexempt charitable H and I are not applicable to section 527 organizations trusts must attach a completed Schedule A (Form 990 or 990-EZ). H(a) Is this a group return for affiliates? F Yes F No H(b) If "Yes" enter number of affiliates - 36 G Website:1- wwwUPMC COM H(c) Are all affiliates included? F Yes F No (If "No," attach a list See instructions ) I Organization type (check only one) 1- F9!!+ -

School of Medicine Office of Admissions & Financial Aid
University of Pittsburgh School of Medicine FACT BOOK » 2018/2019 UNIVERSITY OF PITTSBURGH 2018–19 SCHOOL OF MEDICINE FACT BOOK 1 Overview 2 About the Dean 3 Demographics 3 Curriculum 6 Global Engagement 7 Opportunities for In-Depth Study 9 Degree Programs 10 Institutes and Centers 11 Research Strengths 13 Research Funding 15 Achievements 19 UPMC (University of Pittsburgh Medical Center) 20 City of Bridges 24 Departments 25 Administration ABOUT THE COVER: Scaife Hall entrance, Terrace Street Overview The University of Pittsburgh School of Medicine has a mission to educate science-based, skilled, and compassionate clinicians prepared to meet the challenges of practicing medicine in the 21st century and conduct cutting-edge biomedical research that betters the human condition and advances the fundamental understanding of medical science. In the only truly objective metric by which the overall stature of research-focused institutions can be assessed in a nationally competitive context, the University of Pittsburgh moved into the top 10 list of recipients of National Institutes of Health (NIH) funding in 1998 and has remained within this enviable echelon ever since. In an analysis of NIH funding for federal fiscal year 2017, the faculty of the University of Pittsburgh ranked fifth in total grants awarded, with more than $528 million in funding—approximately 80 percent of which went to the School of Medicine. The School of Medicine operates on a global stage, with active collaborations connecting Pittsburgh with China, France, Ghana, Honduras, India, Italy, Kazakhstan, Malawi, the Philippines, Vietnam, and many other nations. About the Dean ARTHUR S. LEVINE, MD, is senior Dr. -
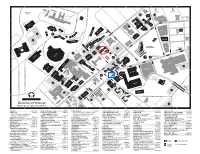
Campus Map 2006–07(09-2006) UPSB
A I B I C I D I E I F I G BRA N E . CKENRIDGE BAPS . T B X CATHO MELWD ATHLETIC T ELLEF E FIELDS P P SP Y DRIV R IS T U AUL D CHDEV E S BELLT LKS I T F K E P AR ELD WEBSR E FA ARKM IN N R AW 1 VA E CR 1 R NUE R T E LEVT C A H AV T Y FIFT S RUSK U E G V S MP A O N N E MUSIC SOUTH CRAIG STREE T N B N LA N A UNIVERSIT R N Y U COS P A W O P S E P VE SO I UCT P LO O . S S U L P HENRY ST T U H E Y N A D L UTD N . Q T C U I L G FR E N T A CRAI S. MELLI L BIG TH B O Y V L C I AT I A N E O BELLEFIELD E CHVR . UE EBER E V HOLD R P MP V A N D I I OP ST. V WINTHR R R IT E M E D D C VE V PANTH N A FRAT I AT ALU H R Y Y U FR T R I T SRC CRGSQ D U S E TH T N I R I Z BELLH V E ID S F S M B P R AW D IG FI HEIN . O L E TH G FILMORE ST L N PAHL V EH UN I ET O SOSA E A E IL A N E F I LO R VE L U PA R S 2 A TR T 2 R RSI W A T N T C LRDC VNGR S CATHEDRAL . -
Upmc-Presbyterian-Visitor-Guide.Pdf
VISITORS INFORMATION GUIDE Welcome Welcome to Pittsburgh and UPMC. An important part of the care we provide is helping our patients and their families to become familiar with their surroundings. Our primary concern is our patients’ health and well-being, but we know this may be a difficult time for their loved ones, too. Inside, you will find information about the hospital, the neighborhood, and the city of Pittsburgh to help you feel more at home. This brochure was created especially for the families and friends of patients at UPMC Presbyterian, which includes UPMC Montefiore. The Eye & Ear Institute as well as Western Psychiatric Institute and Clinic of UPMC are also part of the UPMC Presbyterian family. 1 Please notify your caregiver if you speak [language]. Interpretation services are provided at this facility free of charge. Please let your provider know when you make your appointment that you will need an ASL interpreter. 2 TABLE OF CONTENTS Welcome .................................................................................................1 Quick Telephone Reference ................................................................ 4 Pittsburgh, a “Livable City” .................................................................5 UPMC, a Leader in Health Care ..........................................................5 The Hospital Campus .......................................................................... 6 Arriving on the Oakland Campus ......................................................9 Lodging in the Area .............................................................................12 -

UPMC Interventional Radiology 532 South Aiken Ave
UPMC Interventional Scheduling Radiology Appointments can be scheduled Monday through Friday from 7 a.m. to 3 p.m. through the central scheduling Serving Patients Close to Home numbers listed on the previous page. We have 24-hour emergency coverage at all facilities. For more information or to make referrals, contact us at: UPMC Interventional Radiology 532 South Aiken Ave. Pittsburgh, PA 15232 Telephone: 412-623-2083 Fax: 412-623-0011 To make an appointment, or for more information, call 1-800-533-UPMC (8762) or visit us at UPMC.com . UPMC is an equal opportunity employer. UPMC policy prohibits discrimination or harassment on the basis of race, color, religion, ancestry, national origin, age, sex, genetics, sexual orientation, marital status, familial status, disability, veteran status, or any other legally protected group status. Further, UPMC will continue to support and promote equal employment opportunity, human dignity, and racial, ethnic, and cultural diversity. This policy applies to admissions, employment, and access to and treatment in UPMC programs and activities. This commitment is made by UPMC in accordance with federal, state, and/or local laws and regulations. UPP401450 LGH/SN 10/11 © 2011 UPMC What is interventional Procedures we offer radiology? Vascular: angiogram, balloon angioplasty/stent, DVT, PVD treatment, venous insufficiency, IVC filter placement/retrieval, neurodiagnostics, embolization, adrenal vein sampling Interventional radiologists are board-certified Hematology/Oncology: chemoembolization, physicians who specialize in minimally port placement, pheresis cath placements, Hickman invasive, targeted treatments. They offer the placement, PICC line placement, radiofrequency ablations, TIPS, biliary intervention (PTC) most in-depth knowledge of the least invasive Dialysis: AV fistulagram/declot, vein mapping, treatments available coupled with diagnostic temporary dialysis catheter placement and clinical experience across all specialties. -

Geriatric Medicine Division of Geriatric Medicine
FALL 2018 | UPDATE IN | GERIATRIC MEDICINE DIVISION OF GERIATRIC MEDICINE GERIATRIC OF DIVISION Inside This Edition Message from the Chief 2 Geroscience: Frontiers in the Biology of Aging I am pleased to share our latest issue of Update in Geriatric Medicine, especially our excitement for a 3 New Model of Care Is major augmentation of our research through the creation of a new, focused geroscience initiative led Making a Difference in Osteoporosis Treatment by Toren Finkel, MD, PhD, one of the most distinguished scientists in the field of aging research. 4 UPMC Physician Resources Recruited from the National Institutes of Health in 2017, Dr. Finkel has assembled an impressive team Video Rounds of new investigators to join him. Based on the observation that age itself is the most important risk 5 New Meta-Analysis Shows factor in many diseases affecting our geriatric patients — and data revealing dramatic extension Effects of Interventions on Adverse Drug Reactions of both lifespan and healthspan in experimental models — the goal is to determine which of these experimental strategies might hold the most promise for application in humans. Several of our 6 Testing New Models of Care for Chronic Low Division faculty already are collaborating in this enormous effort. Back Pain 8 Brain Amyloid Deposition Also in this issue of Update in Geriatric Medicine, we showcase new research findings from and the Cognition-Mobility Interface Susan Greenspan, MD, in preventing recurrent hip fractures; an important new initiative in chronic low back pain by Debra Weiner, MD; and new findings fromNeelesh Nadkarni, MD, PhD, on the 10 Welcome New Faculty role of brain amyloid in gait abnormalities.