Resource Manual for Non-GIM Staff Attending Inpatient Medical Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Trauma Treating Traumatic Facial Nerve Paralysis
LETTERS TO EDITOR 205 206 LETTERS TO EDITOR In conclusion, the most frequent type of HBV R. Hepatitis B virus genotype A is more often hearing loss, and an impedance audiogram Strands of facial nerve interconnect with genotype in our study was D type, which associated with severe liver disease in northern showed absent stapedial reflex. CT scan cranial nerves V, VIII, IX, X, XI, and XII and usually causes a mild liver disease. Hence India than is genotype D. Indian J Gastroenterol showed no fracture of the temporal bone and with the cervical cutaneous nerves. This free proper vaccination, e ducational programs, 2005;24:19-22. intact ossicles. The patient was prescribed intermingling of Þ bers of the facial nerve with and treatment with lamivudine are efficient 6. Thakur V, Sarin SK, Rehman S, Guptan RC, high-dose steroids, along with vigorous facial Þ bers of other neural structures (particularly Kazim SN, Kumar S. Role of HBV genotype strategies in controlling HBV infection in our nerve stimulation and massages. the cranial nerve V) has been proposed as in predicting response to lamivudine therapy area. the mechanism of spontaneous return of facial in patients with chronic hepatitis B. Indian J After 3 weeks of treatment, the facial nerve nerve function after peripheral injury to the Gastroenterol 2005;24:12-5. stimulation tests were repeated and the ABDOLVAHAB MORADI, nerve.[4] VAHIDEH KAZEMINEJHAD1, readings were compared to those taken prior to GHOLAMREZA ROSHANDEL, treatment. There was negligible improvement. KHODABERDI KALAVI, Early onset/complete palsy indicates disruption EZZAT-OLLAH GHAEMI2, SHAHRYAR SEMNANI The patient was offered an exploratory of continuity of the nerve. -

Middle Ear Disorders
3/2/2014 ENT CARRLENE DONALD, MMS PA-C ANTHONY MENDEZ, MMS PA-C MAYO CLINIC ARIZONA DEPARTMENT OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY No Disclosures OBJECTIVES • 1. Identify important anatomic structures of the ears, nose, and throat • 2. Assess and treat disorders of the external, middle and inner ear • 3. Assess and treat disorders of the nose and paranasal sinuses • 4. Assess and treat disorders of the oropharynx and larynx • 5. Educate patients on the risk factors for head and neck cancers 1 3/2/2014 Otology External Ear Disorders External Ear Anatomy 2 3/2/2014 Trauma • Variety of presentations. • Rule out temporal bone trauma (battle’s sign & hemotympanum). CT head w/out contrast. • Tx lacerations/avulsions with copious irrigation, closure with dissolvable sutures (monocryl), tetanus update, and antibiotic coverage (anti- Pseudomonal). May need to bolster if concerned for a hematoma . Auricular Hematoma • Due to blunt force trauma. • Drain/aspirate, cover with anti- biotics (anti- Pseudomonals), and apply bolster or passive drain if needed. • Infection and/or cauliflower ear may result if not treated. Chondritis • Inflammation and infection of the auricular cartilage. usually due to Pseudomonas aeruginosa. • Cultures • Treat with empiric antibiotics (anti-Pseudomonal) and I&D if needed. • Differentiate from relapsing polychondritis, which is an autoimmune disorder. 3 3/2/2014 External Auditory Canal Foreign Body • Children –Foreign bodies • Adults – Cerumen plugs • May present with hearing loss, ear pain and drainage • Exam under microscopic otoscopy. Check for otitis externa. • Remove under direct visualization. Can try to neutralize bugs with mineral oil. Do not attempt to irrigate organic material with water as this may cause an infection. -

Ventricular Rhythms Originate Below the Branching Portion of The
Northwest Community Healthcare Paramedic Program VENTRICULAR DYSRHYTHMIAS Pacemakers Connie J. Mattera, M.S., R.N., EMT-P Reading assignments: Bledsoe Vol 3; pp. 96-109 SOPs: VT with pulse; Ventricular fibrillation/PVT; Asystole/PEA Drugs: Amiodarone, magnesium, epinephrine 1mg/10mL Procedure manual: Defibrillation; Mechanical Circulatory Support (MCS) using a Ventricular Assist Device KNOWLEDGE OBJECTIVES: Upon completion of the reading assignments, class and homework questions, reviewing the SOPs, and working with their small group, each participant will independently do the following with at least an 80% degree of accuracy and no critical errors: 1. Identify the intrinsic rates, morphology, conduction pathways, and common ECG features of ventricular beats/rhythms. 2. Identify on a 6-second strip the following: a) Idioventricular rhythm b) Accelerated idioventricular rhythm c) Ventricular tachycardia: monomorphic & polymorphic d) Ventricular escape beats e) Premature Ventricular Contractions (PVCs) f) Ventricular fibrillation g) Asystole h) Paced rhythms i) Intraventricular conduction defects (Bundle branch blocks) 3. Systematically evaluate each complex/rhythm for the following: a) Rate (atrial and ventricular) b) Rhythm: Regular/irregular - R-R Interval, P-P Interval c) Presence/absence/morphology of P waves d) Presence/absence/morphology of QRS complexes d) P-QRS relationships f) QRS duration 4. Correlate the cardiac rhythm with patient assessment findings to determine the emergency treatment for each rhythm according to NWC EMSS SOPs. 5. Discuss the action, prehospital indications, side effects, dose and contraindications of the following during VT a) Amiodarone b) Magnesium 6. Describe the indications, equipment needed, critical steps, and patient monitoring parameters for cardioversion and defibrillation. 7. Identify the management of a patient with an implanted defibrillator and/or pacemaker. -
Final Program N
XXII Congress The International Society on Thrombosis and Haemostasis B July 11-16 2009 O 55th Annual Meeting S of the Scientific and Standardization Committee of the ISTH T O Final Program N Boston - July 11-16 2009 XXII Congress of the International Society on Thrombosis and Haemostasis 2009 Table ISTH of Contents Venue and Contacts 2 Wednesday 209 Welcome Messages 3 – Plenary Lectures 210 Committees 7 – State of the Art Lectures 210 Congress Awards and Grants 15 – Abstract Symposia Lectures 212 Other Meetings 19 – Oral Communications 219 – Posters 239 ISTH Information 20 Program Overview 21 Thursday 305 SSC Meetings and – Plenary Lectures 306 Educational Sessions 43 – State of the Art Lectures 306 – Abstract Symposia Lectures 309 Scientific Program 89 – Oral Communications 316 Monday 90 – Posters 331 – Plenary Lectures 90 Nursing Program 383 – State of the Art Lectures 90 Special Symposia 389 – Abstract Symposia Lectures 92 Satellite Symposia 401 – Oral Communications 100 – Posters 118 Technical Symposia Sessions 411 Exhibition and Sponsors 415 Tuesday 185 – Plenary Lectures 186 Exhibitor and Sponsor Profiles 423 – State of the Art Lectures 186 Congress Information 445 – Abstract Symposia Lectures 188 Map of BCEC 446 – Oral Communications 196 Hotel and Transportation Information 447 ISTH 2009 Congress Information 452 Boston Information 458 Social Events 463 Excursions 465 Authors’ Index 477 1 Venue & Contacts Venue Boston Convention & Exhibition Center 415 Summer Street - Boston, Massachusetts 02210 - USA Phone: +1 617 954 2800 - Fax: +1 617 954 3326 The BCEC is only about 10 minutes by taxi from Boston Logan International Airport. The 2009 Exhibition is located in Hall A and B of the Exhibit Level of the BCEC, along with posters and catering. -

Approach to the Trauma Patient Will Help Reduce Errors
The Approach To Trauma Author Credentials Written by: Nicholas E. Kman, MD, The Ohio State University Updated by: Creagh Boulger, MD, and Benjamin M. Ostro, MD, The Ohio State University Last Update: March 2019 Case Study “We have a motor vehicle accident 5 minutes out per EMS report.” 47-year-old male unrestrained driver ejected 15 feet from car arrives via EMS. Vital Signs: BP: 100/40, RR: 28, HR: 110. He was initially combative at the scene but now difficult to arouse. He does not open his eyes, withdrawals only to pain, and makes gurgling sounds. EMS placed a c-collar and backboard, but could not start an IV. What do you do? Objectives Upon completion of this self-study module, you should be able to: ● Describe a focused rapid assessment of the trauma patient using an organized primary and secondary survey. ● Discuss the components of the primary survey. ● Discuss possible pathology that can occur in each domain of the primary survey and recommend treatment/stabilization measures. ● Describe how to stabilize a trauma patient and prioritize resuscitative measures. ● Discuss the secondary survey with particular attention to head/central nervous system (CNS), cervical spine, chest, abdominal, and musculoskeletal trauma. ● Discuss appropriate labs and diagnostic testing in caring for a trauma patient. ● Describe appropriate disposition of a trauma patient. Introduction Nearly 10% of all deaths in the world are caused by injury. Trauma is the number one cause of death in persons 1-50 years of age and results in significant life years lost. According to the National Trauma Data Bank, falls were the leading cause of trauma followed by motor vehicle collisions (MVCs) and firearm related injuries with an overall mortality rate of 4.39% in 2016. -

Joint Faculty of Intensive Care Medicine
Joint Faculty of Intensive Care Medicine Australian and New Zealand The Royal Australasian College of Anaesthetists College of Physicians ABN 82 055 042 852 Exam Report Oct 2009 This report is prepared to provide candidates, tutors and their supervisors of training with information about the way in which the Examiners assessed the performance of candidates in the Examination. Answers provided are not model answers but guides to what was expected. Candidates should discuss the report with their tutors so that they may prepare appropriately for the future examinations The exam included two 2.5 hour written papers comprising of 15 ten-minute short answer questions each. Candidates were required to score at least 50% in the written paper before being eligible to sit the oral part of the exam. The oral exam comprised 8 interactive vivas and two separate hot cases. This is the fourth examination with the new regulations which came into force in 2008. The tables below provide an overall statistical analysis as well as information regarding performance in the individual sections. A comparison with April 2008, October 2008 and April 2009 data is also provided. Examiner comments Written paper 1) Lack of specificity and precision in the answers. 2) Poor pass rate on clinical methods questions – suggests that candidates are not taking clinical examination seriously and they will need to read books like Talley and O’Connor thoroughly. 3) Candidates seem to score well largely on Data interpretation / OSCE type questions. The inability to score well on other questions reflects a general lack of preparation and knowledge even of common topics in intensive care. -
A Simplified and Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity
R e v i e w Med Princ Pract 2014;23:1–6 Received: February 27, 2013 DOI: 10.1159/000354195 Accepted: July 2, 2013 Published online: August 13, 2013 A Simplified and Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity a b a, c L a s z l o L i t t m a n n Devin J. Bustin Michael W. Haley a b c D e p a r t m e n t s o f Internal Medicine and Emergency Medicine, and Pulmonary and Critical Care Consultants, Carolinas Medical Center, Charlotte, N.C., USA K e y W o r d s Introduction Pulseless electrical activity · Cardiopulmonary resuscitation · Electrocardiogram · Echocardiogram Patients with pulseless electrical activity (PEA) ac- count for up to 30% of cardiac arrest victims [1, 2] . The survival rate of patients with PEA is much worse than that A b s t r a c t of cardiac arrest patients with shockable rhythms [1, 3] . Cardiac arrest victims who present with pulseless electrical Studies suggest that cause-specific treatment of PEA is activity (PEA) usually have a grave prognosis. Several condi- more effective than general treatments offered by ad- tions, however, have cause-specific treatments which, if ap- vanced cardiac life support (ACLS) guidelines such as plied immediately, can lead to quick and sustained recovery. cardiac massage, epinephrine and vasopressin [4] . High- Current teaching focuses on recollection of numerous con- er-dose epinephrine has actually been shown to be associ- ditions that start with the letters H or T as potential causes of ated with worse outcomes [5] . -

SAEMS Cardiac Arrest Standing Order Self-Learning Module
SAEMS Cardiac Arrest Standing Order Self-Learning Module Robert Callan University Physicians Hospital September 8, 2009 SAEMS Standing Order Training Module Cardiac Arrest PURPOSE This SAEMS Standing Order Training Module has been developed to serve as a template for EMS provider training. The intent is to provide consistent and concise information to all providers practicing within the SAEMS Region. The content of the Training Module has been developed by the Protocol Development and Review Committee and includes the specific Standing Order, resource and reference material and instructions for completing the Training Module to obtain continuing education credit. One hour of SAEMS continuing education credit may be issued following successful completion of the module. OBJECTIVES 1. Review basic cardiac arrest evaluation techniques 2. Recognize cardiac arrest pathology 3. Apply the Cardiac Arrest Standing Order appropriately Instructions 1. Review the accompanying information, Standing Order and any additional reference material as necessary. 2. Complete the attached posttest and return it to your supervisor or base hospital coordinator. 3. A SAEMS CE Form will be issued to providers scoring greater than _____% on the posttest. 4. Please contact your Base Hospital Manager/Coordinator for questions, suggestions or concerns. TABLE OF CONTENTS 1. Purpose 2. Objectives 3. Instructions 4. Table of Contents 5. Cardiac Arrest 6. Glossary 7. Cardiac Arrest Center (CAC) Triage Protocol 8. Standing Order 9. Posttest 2 INTRODUCTION Cardiac Arrest Cardiac arrest, also known as cardiopulmonary arrest or circulatory arrest, is the sudden abrupt cessation of normal circulation of the blood due to failure of the heart to contract effectively during systole. -
2015 AHA BLS And
Update 2015 AHA BLS and 40 l Nursing2016 l Volume 46, Number 2 www.Nursing2016.com Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved. ACLS guidelines By Karen Jean Craig-Brangan, BS, RN, EMT-P, and Mary Patricia Day, MSN, RN, CRNA ADVANCED CARDIOVASCULAR life support (ACLS) encompasses the entire spectrum of care from basic life support (BLS) to postcardiac arrest care. The 2015 American Heart Association (AHA) guidelines include recommendations on the use of I.V./intraosseous (I.O.) epinephrine, I.V./I.O. vasopressin during cardiac arrest, and end-tidal carbon dioxide (ETCO2) measurements to predict patient outcome.1 Let’s take a closer look at these changes and more. Managing cardiac arrest in an adult The Adult Cardiac Arrest Algorithm outlines a plan of care for the patient in cardiac arrest sec- ondary to pulseless ventricular tachycardia (pVT)/ ventricular fibrillation (VF). After determining unresponsiveness, apnea, and pulselessness, the clinician administers chest compressions and ventilations at a ratio of 30:2 respectively until an advanced airway is in place. Advanced air- ways include an endotracheal tube (ETT) or supraglottic airway (SGA) device such as a laryn- geal mask airway, laryngeal tube, or esophageal obturator airway. The new BLS guidelines recommend a com- pression rate of at least 100/minute and no great- er than 120/minute, and a compression depth of at least 2 in (5 cm) and no greater than 2.4 in (6 cm) for an average adult.2 Upper limits for both compression rate and depth have been provided TOCK in the updated guidelines based on preliminary /iS data suggesting that excessive compression MAGES I rates and depths can adversely affect patient out- comes. -
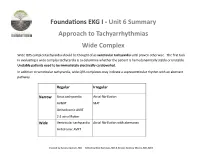
Foundations EKG I - Unit 6 Summary Approach to Tachyarrhythmias Wide Complex
Foundations EKG I - Unit 6 Summary Approach to Tachyarrhythmias Wide Complex Wide QRS complex tachycardia should be thought of as ventricular tachycardia until proven otherwise. The first task in evaluating a wide complex tachycardia is to determine whether the patient is hemodynamically stable or unstable. Unstable patients need to be immediately electrically cardioverted. In addition to ventricular tachycardia, wide QRS complexes may indicate a supraventricular rhythm with an aberrant pathway. Regular Irregular Narrow Sinus tachycardia Atrial fibrillation AVNRT MAT Orthodromic AVRT 2:1 atrial flutter Wide Ventricular tachycardia Atrial fibrillation with aberrancy Antidromic AVRT Created by Ashley Deutsch, MD Edited by Nick Hartman, MD & Kristen Grabow Moore, MD, MEd Ventricular tachycardia is likely if there is: • AV dissociation • QRS over 140s • Positive precordial QRS complexes Sustained ventricular tachycardia lasts over 30 seconds. Treatment of hemodynamically stable ventricular tachycardia may include administration of lidocaine, procainamide, or amiodarone. It is important to consider reversible causes (commonly referred to as the “Hs and Ts”). Unstable ventricular tachycardia mandates immediate synchronized cardioversion. SVT with aberrant conduction pathways may also cause wide complex tachycardia. Conduction of AVRT may be ortho- dromic (traveling down the normal direction of the nerve fibers) or antidromic (opposite to the normal conduction path- way). Antidromic conduction tends to cause a wide QRS complex whereas orthodromic often causes a narrow complex . Courtesy of Edward Burns of Life in the Fast Lane Creative Commons License Wolff-Parkinson-White (WPW) is a pre-excitation syndrome. Evidence of the accessory pathway causing tachycardia can be seen in the delta wave causing upslurring to the QRS with a short PR interval. -

Endovascular Treatment of Pseudoaneurysms with Electrolytically Detachable Coils
AJNR Am J Neuroradiol 19:907–911, May 1998 Endovascular Treatment of Pseudoaneurysms with Electrolytically Detachable Coils Todd E. Lempert, Van V. Halbach, Randall T. Higashida, Christopher F. Dowd, Ross W. Urwin, Peter A. Balousek, and Grant B. Hieshima PURPOSE: We describe the clinical presentation, angiographic findings, and clinical out- come in a group of patients with pseudoaneurysms treated by a new endovascular technique using Guglielmi electrolytically detachable platinum coils (GDCs). METHODS: We retrospectively reviewed the angiographic and clinical findings in a series of 11 patients with pseudoaneurysms occurring in a variety of locations: seven in the cavernous carotid artery, one in the petrous carotid artery, two in the anterior cerebral artery, and one in the cervical vertebral artery. RESULTS: All aneurysms were cured with GDC embolization. The only complication was a branch occlusion, which resolved with heparinization and produced no clinical sequelae. CONCLUSION: Pseudoaneurysms can be safely and effectively treated by embolization with GDCs. Consideration needs to be given to the anatomic location of the pseudoaneurysm and the acuity of onset. Treatment efficacy may by improved if there are bony confines around the aneurysm or if therapy takes place in the subacute period, when the wall of the pseudoaneurysm has matured and stabilized. Pseudoaneurysms of intracranial and neck vessels seconds. Maintenance heparin was given as half the initial dose are a well-described entity. They can carry a high rate every hour. A 6F or 7F guidecatheter was positioned to permit of morbidity and mortality and, depending on their digital roadmapping. A Tracker (Target Therapeutics) or Rapid Transit (Cordis Corp, Miami, Fla) microcatheter was location, be extremely difficult to treat by surgical navigated into the aneurysm using a 0.014-inch platinum tip means without sacrificing the parent artery. -

The IOC Manual of Emergency Sports Medicine
Trim Size: 216 mm X 279 mm fm.indd 03:4:4:PM 02/09/2015 Page ii Trim Size: 216 mm X 279 mm fm.indd 03:4:4:PM 02/09/2015 Page i THE IOC MANUAL OF EMERGENCY SPORTS MEDICINE Trim Size: 216 mm X 279 mm fm.indd 03:4:4:PM 02/09/2015 Page ii Trim Size: 216 mm X 279 mm fm.indd 03:4:4:PM 02/09/2015 Page iii THE IOC MANUAL OF EMERGENCY SPORTS MEDICINE EDITED BY DAVID McDonagh and DAVID ZIDEMAN Trim Size: 216 mm X 279 mm fm.indd 03:4:4:PM 02/09/2015 Page iv This edition first published 2015 © 2015 by the International Olympic Committee Wiley-Blackwell is an imprint of John Wiley & Sons, formed by the merger of Wiley’s global Scientific, Technical and Medical business with Blackwell Publishing. Registered office: John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offices: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offices, for customer services and for information about how to apply for permis- sion to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identified as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher.