Long Melford Practice Local Patient Participation Report 2012/13
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1. Parish: Little Waldingfield
1. Parish: Little Waldingfield Meaning: Open area of the dwellers by the ‘wold’ or wood 2. Hundred: Babergh Deanery: Sudbury (-1864), Sudbury (Western) (1864-1884), Lavenham (1884-1957), Sudbury (1957-) Union: Sudbury RDC/UDC: (W. Suffolk) Melford RD (–1974), Babergh DC (1974–) Other administrative details: Melford Petty Sessional Division Sudbury County Court District 3. Area: 1630 acres (1912) 4. Soils: Some slowly permeable calcareous/ non calcareous clay soils, slight risk water erosion 5. Types of farming: 1500–1640 Thirsk: Wood-pasture region, mainly pasture, meadow, engaged in rearing and dairying with some pig-keeping, horse breeding and poultry. Crops mainly barley with some wheat, rye, oats, peas, vetches, hops and occasionally hemp 1818 Marshall: Course of crops varies usually including summer fallow as preparation for corn products 1937 Main crops: Barley, wheat, oats 1969 Trist: More intensive cereal growing and sugar beet 6. Enclosure: Will of John Wyncoll (1580) refers to ’12 acres of land taken and enclosed on the Church Field’. Beyond Living Memory by H. Clive (1979) 7. Settlement: 1977 Compact development. Church centrally situated. Some scattered farms. Inhabited houses: 1674 – 40, 1801 – 75,1851–93, 1871 –87, 1901 –74, 1951 –81, 1981 – 135 1 8. Communications: Road: To Brent Eleigh, Edwardstone and Gt. Waldingfield 1844 Carrier to Ipswich on Monday, Wednesday and Friday Rail: 1891 4½ miles Sudbury station, opened 1849, line to Shelford opened 1854, line to Haverhill opened 1865, closed for goods 1966, closed for passengers 1967 9. Population: 1086 — 66 recorded (includes Great Waldingfield) 1327 —16 taxpayers paid £1. 13s. 3d. 1524 — 57 taxpayers paid £21. -

Bildeston - Hadleigh 112 Sudbury - Chelsworth 112A MONDAYS, WEDNESDAYS, THURSDAYS & SATURDAYS (Except Public Holidays) From: 16Th April 2012
BEESTONS, TravEL SErviCES Sudbury - Bildeston - Hadleigh 112 Sudbury - Chelsworth 112A MONDAYS, WEDNESDAYS, THURSDAYS & SATURDAYS (Except Public Holidays) From: 16th April 2012 Operator TS TS TS TS BE Service 112 112A 112A 112 112 Notes MW Th Th MW S Sch Sch Sch Sch Sudbury, Bus Station .............................................. 0930 0930 1200 1255 1345 Great Waldingfield, The Heath, opp Post Office ....... 0938 0938 1208 1303 1353 Little Waldingfield, The Street, The Swan ................ 0942 0942 1212 1307 1356 Brent Eleigh, A1141, opp Milden Road ...................... 0949 0949 1219 1314 1403 Monks Eleigh, The Street, The Swan ........................ 0952 0952 1222 1317 1406 Chelsworth, The Street, The Peacock ....................... | 0955 1225 | 1409 Bildeston, Market Place, opp Clock Tower ................ | -- -- | 1420 Semer, B1115, opp Semer Bridge .............................. | -- -- | 1427 Semer, adj Sayers Farm ............................................. 0957 -- -- 1322 | Hadleigh, Calais Street, Buyright ............................... 1007 -- -- 1332 | Hadleigh, Bus Station .............................................. 1009 -- -- 1334 1435 Hadleigh, Highlands Road, High School .................... 1011 -- -- 1336 -- Hadleigh, Bus Station .............................................. 1013 -- -- 1338 -- What the notes mean: MW - Mondays & Wednesdays only S - Saturdays only Sch - Schooldays only Th - Thursdays only Operator Contact: BE - Beestons 01473 823243 TS - Travel Services 01473 341500 Further Information -
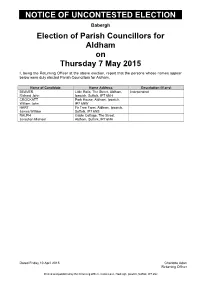
Notice of Uncontested Election
NOTICE OF UNCONTESTED ELECTION Babergh Election of Parish Councillors for Aldham on Thursday 7 May 2015 I, being the Returning Officer at the above election, report that the persons whose names appear below were duly elected Parish Councillors for Aldham. Name of Candidate Home Address Description (if any) BEAVER Little Rolls, The Street, Aldham, Independent Richard John Ipswich, Suffolk, IP7 6NH CROCKATT Park House, Aldham, Ipswich, William John IP7 6NW HART Fir Tree Farm, Aldham, Ipswich, James William Suffolk, IP7 6NS RALPH Gable Cottage, The Street, Jonathan Michael Aldham, Suffolk, IP7 6NH Dated Friday 10 April 2015 Charlotte Adan Returning Officer Printed and published by the Returning Officer, Corks Lane, Hadleigh, Ipswich, Suffolk, IP7 6SJ NOTICE OF UNCONTESTED ELECTION Babergh Election of Parish Councillors for Alpheton on Thursday 7 May 2015 I, being the Returning Officer at the above election, report that the persons whose names appear below were duly elected Parish Councillors for Alpheton. Name of Candidate Home Address Description (if any) ARISS Green Apple, Old Bury Road, Alan George Alpheton, Sudbury, CO10 9BT BARRACLOUGH High croft, Old Bury Road, Richard Alpheton, Suffolk, CO10 9BT KEMP Tresco, New Road, Long Melford, Independent Richard Edward Suffolk, CO10 9JY LANKESTER Meadow View Cottage, Bridge Maureen Street, Alpheton, Suffolk, CO10 9BG MASKELL Tye Farm, Alpheton, Sudbury, Graham Ellis Suffolk, CO10 9BL RIX Clapstile Farm, Alpheton, Farmer Trevor William Sudbury, Suffolk, CO10 9BN WATKINS 3 The Glebe, Old Bury Road, Ken Alpheton, Sudbury, Suffolk, CO10 9BS Dated Friday 10 April 2015 Charlotte Adan Returning Officer Printed and published by the Returning Officer, Corks Lane, Hadleigh, Ipswich, Suffolk, IP7 6SJ NOTICE OF UNCONTESTED ELECTION Babergh Election of Parish Councillors for Assington on Thursday 7 May 2015 I, being the Returning Officer at the above election, report that the persons whose names appear below were duly elected Parish Councillors for Assington. -

1 the Street, Brent Eleigh, Sudbury, Suffolk. Co10 9Nr
1 THE STREET, BRENT ELEIGH, SUDBURY, SUFFOLK. CO10 9NR Brent Eleigh is a charming Suffolk village surrounded by open countryside with a well-supported local pub and parish church. The village enjoys close links with the medieval village of Lavenham (2 miles) which provides a comprehensive range of amenities. A commuter rail link is available in nearby Sudbury (8 miles). This one bedroom ground floor maisonette is set in the heart of the popular village of Brent Eleigh. The property is in the need of updating and would be a good investment for both first time buyers and ‘buy to let’ clients. The property benefits from a wet room, large reception room, communal garden and outside store. A ground floor maisonette located in the heart of this popular Suffolk village. Guide £79,995 LONG MELFORD (01787) 883144 Castle Hedingham Clare Leavenheath Newmarket Woolpit London EC1 w w w . d a v i dburr.co.uk 1 THE STREET, BRENT ELEIGH, SUDBURY, SUFFOLK. CO10 9NR ENTRANCE HALL: LEASEHOLD: The property is subject to a 125 year lease with approximately 125 years SITTING/DINING ROOM: 4.46m x 4.04m. remaining. Service charge: £220.00 per annum. (14’7” x 13’3”). Built in double cupboard and Ground rent: £10.00 per annum. large window overlooking the rear garden. SERVICES: Main water, drainage and electricity connected. NOTE: None of the services have been tested by the agent. EPC RATING: Band E - A copy of the energy performance certificate is available on request. LOCAL AUTHORITY: Babergh and Mid Suffolk District Councils, Endeavour House, 8 Russell Road, Ipswich, Suffolk. -

Boxford • Edwardstone • Groton • Little Waldingfield • Newton Green Vol 19 No 8 RBEV Roob Mxov ESR in Iver News
August 2019 Boxford • Edwardstone • Groton • Little Waldingfield • Newton Green Vol 19 No 8 RBEV RoOB MxOV ESR IN iver News ‘Bishop’s Move’! Revd Rob standing in front of the removals van outside the rectory in Boxford after he moved from Orpington to Boxford on 10th July. In welcoming Rob and his family to the benefice, we hope that his next ‘bishop’s move’ won’t occur for many years yet! TEAM ITFC CYCLE TO AMSTERDAM FOR PROSTATE CHARITY INSTITUTION AND INDUCTION of THE REVD ROBERT PARKER-McGEE as RECTOR OF THE BOX RIVER BENEFICE Tuesday 20 August 2019 at 7.30 pm St Lawrenceʼs Church, Little Waldingfield Guests at Stoke by Nayland Hotel, were joined by a few familiar faces on Friday 7th June, as former ITFC midfielder Simon Milton and his team of ALL ARE WELCOME TO THIS SERVICE charity cyclists rode in for lunch on their way from Ipswich to Amsterdam. WHEN ROB IS FORMALLY COMMISSIONED The annual charity bike ride in aid of Prostate Cancer UK, sees teams of fans and former professional footballers cycle from as far afield as London and TO START HIS MINISTRY AMONG US Yorkshire to Amsterdam. Team ITFC, which comprised of 21 riders including Town legends Titus DO COME ! Bramble and Alan Lee, set off from Ipswich on Friday 7th June. Cycling across the East Anglian countryside on Friday, the team stopped at the Hotel Refreshments will be served after the service. to fill up on an energising lunch, before setting off to Harwich where they arrived safely (though a little wet!) on Friday evening. -

Patient Participation Group Survey Report 2013/14
Long Melford Practice Patient Participation Group Survey Report 2013/14 1 CONTENTS 1.0 Introduction 3 2.1 Practice Profile 3 2.2 Patient Participation Group 4 3.0 Local Practice Survey 5 3.1 2013/2014 Patient Survey Results 6 3.2 Patient Comments 28 4.0 Practice comments and feedback 29 5.0 Actions and Plans for the future 29 5.1 Final Note 30 6.0 Access 30 2 1.0 Introduction The Long Melford Practice established a Patient Participation Group (PPG) to encourage patients to become more involved in decisions relating to both the quality and range of services provided by the Long Melford Practice. It was envisaged that while still in its infancy, the PPG would grow in membership and become a representative voice of the local patient population and have an increasing influence on how the practice develops/ commissions its services. In April 2013 the new governing bodies, National Commissioning Board, West Suffolk Clinical Commissioning Group, Suffolk County Council came into effect. These bodies oversee, the provision of Primary Health Care in West Suffolk. As mentioned in last year’s survey Primary Health Care is going through a period of extreme change. The support and contribution from the PPG at this time is an integral part of our ongoing focus to ensure that our patients are more involved in decisions relating to both the quality and range of services provided by the Long Melford Practice to the local community. The survey commissioned for the year ending March 2014 was based on the General Practice Assessment Questionnaire (GPAQ) survey and adapted for local use by asking questions relevant to the issues raised by the PPG, these included patient access and practice refurbishment. -

EDWARDSTONE PARISH COUNCIL Minutes of the Meeting of Edwardstone Parish Council at Edwardstone Parish Hall on Monday 15 July 2019 at 7.30Pm
EDWARDSTONE PARISH COUNCIL Minutes of the Meeting of Edwardstone Parish Council at Edwardstone Parish Hall on Monday 15 July 2019 at 7.30pm. Present: P Baker, S Norman, P Clarke, M Gibson In attendance: R Jones (Clerk) J Finch (SCC), B Hurren (BDC) 1. Apologies for absence – D Williams. 2. Councillors’ Declarations of Interest in any item on this Agenda – None 3. Reports from Suffolk County Council and Babergh District Council 3.1 Councillor James Finch reported the following: Electric vehicle charging points to be installed at 100 business premises across the County. Reduction in Bus services due to removal of some public funding. Services were currently costing SCC roughly £25 per customer journey which was unsustainable. Applications were being taken from local people over 18 for placements at museums across Suffolk and Essex following a National Lottery Grant. Superfast Broadband should be connected in Priory Green area by the end of July. Councillors were asked to provide Councillor Finch with details of any properties not receiving the service or with poor signal. Suffolk Health and Wellbeing Board working with Public Health England to improve mental health provision in the County. Councillor Finch was taking part in a number of Sponsored Walks to help raise awareness and funding for Suffolk Mind, his chosen charity as Chairman of SCC. Members of the public in attendance asked Councillor Finch for an update on the changes to School bus provision for Edwardstone which was adversely affecting local families. Councillor Finch to make enquiries and contact them directly. 3.2 Councillor Bryn Hurren reported the following: First meeting of the new BDC Council had taken place with less members due to the boundary changes. -

BABERGH DISTRICT COUNCIL BAMBRIDGE HALL, FURTHER STREET ASSINGTON Grid Reference TL 929 397 List Grade II Conservation Area No D
BABERGH DISTRICT COUNCIL BAMBRIDGE HALL, FURTHER STREET ASSINGTON Grid Reference TL 929 397 List Grade II Conservation Area No Description An important example of a rural workhouse of c.1780, later converted to 4 cottages. Timber framed and plastered with plaintiled roof. 4 external chimney stacks, 3 set against the rear wall and one on the east gable end. C18-C19 windows and doors. The original building contract survives. Suggested Use Residential Risk Priority C Condition Poor Reason for Risk Numerous maintenance failings including areas of missing plaster, missing tiles at rear and defective rainwater goods. First on Register 2006 Owner/Agent Lord and Lady Bambridge Kiddy, Sparrows, Cox Hill, Boxford, Sudbury CO10 5JG Current Availability Not for sale Notes Listed as ‘Farend’. Some render repairs completed and one rear chimney stack rebuilt but work now stalled. Contact Babergh / Mid Suffolk Heritage Team 01473 825852 BABERGH DISTRICT COUNCIL BARN 100M NE OF BENTLEY HALL, BENTLEY HALL ROAD BENTLEY Grid Reference TM 119 385 List Grade II* Conservation Area No Description A large and fine barn of c.1580. Timber-framed, with brick- nogged side walls and brick parapet end gables. The timber frame has 16 bays, 5 of which originally functioned as stables with a loft above (now removed). Suggested Use Contact local authority Risk Priority A Condition Poor Reason for Risk Redundant. Minor slippage of tiles; structural support to one gable end; walls in poor condition and partly overgrown following demolition of abutting buildings. First on Register 2003 Owner/Agent Mr N Ingleton, Ingleton Group, The Old Rectory, School Lane, Stratford St Mary, Colchester CO7 6LZ (01206 321987) Current Availability For sale Notes This is a nationally important site for bats: 7 types use the building. -

Notice of Poll Babergh
Suffolk County Council ELECTION OF COUNTY COUNCILLOR FOR THE BELSTEAD BROOK DIVISION NOTICE OF POLL NOTICE IS HEREBY GIVEN THAT :- 1. A Poll for the Election of a COUNTY COUNCILLOR for the above named County Division will be held on Thursday 6 May 2021, between the hours of 7:00am and 10:00pm. 2. The number of COUNTY COUNCILLORS to be elected for the County Division is 1. 3. The names, in alphabetical order and other particulars of the candidates remaining validly nominated and the names of the persons signing the nomination papers are as follows:- SURNAME OTHER NAMES IN HOME ADDRESS DESCRIPTION PERSONS WHO SIGNED THE FULL NOMINATION PAPERS 16 Two Acres Capel St. Mary Frances Blanchette, Lee BUSBY DAVID MICHAEL Liberal Democrats Ipswich IP9 2XP Gifkins CHRISTOPHER Address in the East Suffolk The Conservative Zachary John Norman, Nathan HUDSON GERARD District Party Candidate Callum Wilson 1-2 Bourne Cottages Bourne Hill WADE KEITH RAYMOND Labour Party Tom Loader, Fiona Loader Wherstead Ipswich IP2 8NH 4. The situation of Polling Stations and the descriptions of the persons entitled to vote thereat are as follows:- POLLING POLLING STATION DESCRIPTIONS OF PERSONS DISTRICT ENTITLED TO VOTE THEREAT BBEL Belstead Village Hall Grove Hill Belstead IP8 3LU 1.000-184.000 BBST Burstall Village Hall The Street Burstall IP8 3DY 1.000-187.000 BCHA Hintlesham Community Hall Timperleys Hintlesham IP8 3PS 1.000-152.000 BCOP Copdock & Washbrook Village Hall London Road Copdock & Washbrook Ipswich IP8 3JN 1.000-915.500 BHIN Hintlesham Community Hall Timperleys Hintlesham IP8 3PS 1.000-531.000 BPNN Holiday Inn Ipswich London Road Ipswich IP2 0UA 1.000-2351.000 BPNS Pinewood - Belstead Brook Muthu Hotel Belstead Road Ipswich IP2 9HB 1.000-923.000 BSPR Sproughton - Tithe Barn Lower Street Sproughton IP8 3AA 1.000-1160.000 BWHE Wherstead Village Hall Off The Street Wherstead IP9 2AH 1.000-244.000 5. -

3 the Street, Little Waldingfield, Sudbury, Suffolk. Co10 0Sq
3 THE STREET, LITTLE WALDINGFIELD, SUDBURY, SUFFOLK. CO10 0SQ PHOTO TO BE APPENDED 3 The Street Long Melford 01787 883144 Leavenheath 01206 263007 Clare 01787 277811 Castle Hedingham 01787 463404 Woolpit 01359 245245 Newmarket 01638 669035 Little Waldingfield, Sudbury,Bury St Edmunds Suffolk 01284 725525 London 020 78390888 Linton & Villages 01440 784346 3 THE STREET, LITTLE WALDINGFIELD, SUDBURY, SUFFOLK. CO10 0SQ Little Waldingfield is a most attractive village with a pub and church. The market town of Sudbury, with its comprehensive amenities (including a commuter rail link with London’s Liverpool Street) is about 5 miles away. The historic settlement of Lavenham is some 4 miles distant.) This spacious village house occupies a lovely position and enjoys far reaching field views. The property has been sympathetically enlarged and offers extensive ground floor living space of considerable versatility. Further benefits include ample off-road parking and a particularly generous garden. A spacious village house with a large garden and far reaching views. Front door opening to: UTILITY ROOM: (2.46m x 1.98m) 8’1” x 6’6” A useful room with a tiled ENTRANCE HALL: A spacious area with a tiled floor, staircase off and floor, door to side garden, plumbing for washing machine and space for a Suffolk latch doors to: tumble dryer. Fitted work top and useful storage cupboards. Door to: SITTING ROOM: (5.05m x 4.29m) 16’7” x 14’1” Over-looking the front CLOAKROOM: Fitted WC and wash hand basin. garden and finished with a fire place that includes a log burning stove on a slate hearth. -

New Home, Brent Eleigh Road, Monks Eleigh, Suffolk
NEW HOME ADJ FEN COTTAGE, BRENT ELEIGH ROAD, MONKS ELEIGH, SUFFOLK. IP7 7JG New Home, Brent Eleigh Road, Long Melford 01787 883144 Leavenheath 01206 263007 Clare 01787 277811 Castle Hedingham 01787 463404 Woolpit 01359 245245 Newmarket 01638 669035 Monks Eleigh, Suffolk. Bury St Edmunds 01284 725525 London 020 78390888 Linton & Villages 01440 784346 NEW HOME ADJ FEN COTTAGE, BRENT ELEIGH ROAD, MONKS ELEIGH, SUFFOLK. IP7 7JG Monks Eleigh is a pretty Suffolk village, bisected by the river Brett and surrounded by undulating countryside. There is a strong sense of community with well supported pub, shop, post office and Parish Church. The market town of Sudbury, 8 miles, provides a comprehensive range of amenities with a commuter rail service to London Liverpool Street, whilst the smaller town of Hadleigh stands about 4 miles to the East. Ipswich is 16 miles and provides fast access to the A14 and A12 trunk roads. A detached three bedroom house situated on the edge of a picturesque and well-served Suffolk village. Due for completion in Autumn/Winter 2021 the property will offer an accommodation schedule which includes a spacious entrance hall with a ground floor cloakroom off, large drawing room with a wood- burning stove, open-plan island kitchen/dining room and a further family room with bi-folding doors opening onto the garden. There is the additional benefit of a utility room and plenty of storage. Upstairs are three double bedrooms and a family bathroom together with an ensuite for the master bedroom. To the right hand side of the property, a private vehicular access will give way to an area of off-road parking and to the left hand side is a landscaped garden and terrace. -

Apm 290 Lindsey Parish Council
APM 290 LINDSEY PARISH COUNCIL CLERK TO THE COUNCIL The Annual Parish Meeting for Lindsey was held on 15th May 2019 at 7.00pm in the Village Hall. The Chair of the Parish Council, Councillor Arthey would take the Chair for the meeting. He continued by welcoming the newly elected Parish Councillors R. Corcoran; M. Hainsworth; Mrs. R. Howe and A. Sturgeon, as well as Mrs V Waples (Clerk), District Councillor Leigh Jamieson and past District Councillor Bryn Hurren. 1. The Chair of the Parish Council welcomed all to the meeting. 2. Apologies for absence were received from County Cllr. James Finch 3. The minutes of the previous meeting of 9th May 2018 were approved by all present and signed by the Chairman of the Parish Council as a true and accurate record. 4. To receive a report on Village Issues that have arisen over the past year: there were no issues raised at the previous Annual Parish Meeting. The following reports were then given as follows 5. MR JAMES FINCH - COUNTY COUNCILLOR – no report was received from County Cllr. James Finch. The clerk agreed to contact Mr. Finch to ascertain if he wanted to submit his report for circulation by email. 6. MR BRYN HURREN – EX DISTRICT COUNCILLOR – Mr Hurren was invited to submit his report to the meeting as the outgoing District Councillor and commented on the following items: Ward changes - after last year’s appraisal of the district by the Government Boundary Commission, the representation of Councillors at Babergh has been cut from 43 to 32. This has meant that each Councillor will now be responsible for more residents and villages.