EASD2021-Final Programme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2015 Prediabetes Data Summary
The Georgia Department of Public Health Prediabetes Data Summary Diabetes is the 6th leading cause of death among adults and over 800,000 people live with diabetes in Georgia.1 Individuals with prediabetes have an increased risk of developing Type 2 diabetes, heart disease and stroke. Moreover, individuals with prediabetes often possess cardiovascular risk factors such as hypertension, obesity and high cholesterol. Prediabetes almost always occurs among individuals who eventually develop Type 2 diabetes.2 In Type 2 diabetes, the body does not use insulin properly which causes blood glucose (sugar) levels to be higher than normal. Approximately 450,000 adults in Georgia have prediabetes. Prediabetes (also known as borderline diabetes) is a medical condition that occurs when blood glucose levels are higher than normal, but are not high enough to be diagnosed as diabetes.3 Test results among individuals diagnosed with prediabetes include: A1C test value: 5.7% - 6.4% Impaired fasting blood glucose (IFG) levels: 100-125 mg/dl OR Two- hour Oral Glucose Tolerance Test (OGTT) value: 140 mg/dl – 199 mg/dl Making healt hy lifestyle choices, such as eating healthy foods, being physically active and maintaining a healthy weight, may help to bring blood glucose (sugar) levels down to normal and decrease the risk of developing Type 2 diabetes Table 1. Demographic Characteristics among Prediabetics, Georgia, 2013 Demographic Characteristics Percent (%) 95% CI State Total 7.9 (7.2, 8.9) Sex Male 7.8 (6.8, 9.5) Female 7.9 (6.9, 9.1) Race/Ethnicity -

Multifaceted Physiological Roles of Adiponectin in Inflammation And
International Journal of Molecular Sciences Review Multifaceted Physiological Roles of Adiponectin in Inflammation and Diseases Hyung Muk Choi 1, Hari Madhuri Doss 1,2 and Kyoung Soo Kim 1,2,* 1 Department of Clinical Pharmacology and Therapeutics, Kyung Hee University School of Medicine, Seoul 02447, Korea; [email protected] (H.M.C.); [email protected] (H.M.D.) 2 East-West Bone & Joint Disease Research Institute, Kyung Hee University Hospital at Gangdong, Gandong-gu, Seoul 02447, Korea * Correspondence: [email protected]; Tel.: +82-2-961-9619 Received: 3 January 2020; Accepted: 10 February 2020; Published: 12 February 2020 Abstract: Adiponectin is the richest adipokine in human plasma, and it is mainly secreted from white adipose tissue. Adiponectin circulates in blood as high-molecular, middle-molecular, and low-molecular weight isoforms. Numerous studies have demonstrated its insulin-sensitizing, anti-atherogenic, and anti-inflammatory effects. Additionally, decreased serum levels of adiponectin is associated with chronic inflammation of metabolic disorders including Type 2 diabetes, obesity, and atherosclerosis. However, recent studies showed that adiponectin could have pro-inflammatory roles in patients with autoimmune diseases. In particular, its high serum level was positively associated with inflammation severity and pathological progression in rheumatoid arthritis, chronic kidney disease, and inflammatory bowel disease. Thus, adiponectin seems to have both pro-inflammatory and anti-inflammatory effects. This indirectly indicates that adiponectin has different physiological roles according to an isoform and effector tissue. Knowledge on the specific functions of isoforms would help develop potential anti-inflammatory therapeutics to target specific adiponectin isoforms against metabolic disorders and autoimmune diseases. -
Footprints an Informational Newsletter for Patients of APMA Member Podiatrists October 2017
footprints an informational newsletter for patients of APMA member podiatrists october 2017 special EDITION include a DPM for diabetes prevention & Manage Ment According to the CDC, more than 100 million US adults are living with either diabetes or prediabetes. If you have diabetes or prediabetes, it is essential to include a podiatrist for proper diabetes prevention and management. In fact, podiatrists can reduce amputation rates up to 80 percent. In order for you not to become a part of that statistic, here are a few simple things you can do to keep your risk for diabetic ulcers and amputation low: Inspect feet daily. Check your Don’t go barefoot. Don’t go 1 feet and toes every day for 5 without shoes, even in your cuts, bruises, sores, or changes to own home. The risk of cuts and the toenails, such as thickening or infection is too great for those discoloration. with diabetes. Wear thick, soft socks. Avoid Never try to remove calluses, 2 socks with seams, which could 6 corns, or warts by yourself. rub and cause blisters or other Over-the-counter products can burn skin injuries. the skin and cause irreparable damage to the foot for people Exercise. Walking can keep with diabetes. 3 weight down and improve circulation. Be sure to wear See a podiatrist. Regular appropriate athletic shoes when 7 checkups by a podiatrist— exercising. at least annually—are the best WALKING CAN KEEP way to ensure that your feet WEIGHT DOWN AND Have new shoes properly remain healthy. 4 measured and fitted. Foot size IMPROVE CIRCULATION. -

Adiporon, an Orally Active, Synthetic Agonist of Adipor1 and Adipor2 Receptors Has Gastroprotective Effect in Experimentally Induced Gastric Ulcers in Mice
molecules Article AdipoRon, an Orally Active, Synthetic Agonist of AdipoR1 and AdipoR2 Receptors Has Gastroprotective Effect in Experimentally Induced Gastric Ulcers in Mice Hubert Zatorski 1,2, Maciej Salaga 1 , Marta Zieli ´nska 1, Kinga Majchrzak 1, Agata Binienda 1 , Radzisław Kordek 3, Ewa Małecka-Panas 2 and Jakub Fichna 1,4,* 1 Department of Biochemistry, Medical University of Lodz, 92-215 Lodz, Poland; [email protected] (H.Z.); [email protected] (M.S.); [email protected] (M.Z.); [email protected] (K.M.); [email protected] (A.B.) 2 Department of Digestive Tract Diseases, Medical University of Lodz, 93-281 Lodz, Poland; [email protected] 3 Department of Pathology, Medical University of Lodz, 92-215 Lodz, Poland; [email protected] 4 Department of Biochemistry, Faculty of Medicine, Medical University of Lodz, Mazowiecka 6/8, 92-215 Lodz, Poland * Correspondence: jakub.fi[email protected]; Tel.: +48-42-272-57-07 Citation: Zatorski, H.; Salaga, M.; Abstract: Introduction: Adiponectin is a hormone secreted by adipocytes, which exhibits insulin- Zieli´nska,M.; Majchrzak, K.; sensitizing and anti-inflammatory properties and acts through adiponectin receptors: AdipoR1 and Binienda, A.; Kordek, R.; AdipoR2. The aim of the study was to evaluate whether activation of adiponectin receptors AdipoR1 Małecka-Panas, E.; Fichna, J. and AdipoR2 with an orally active agonist AdipoRon has gastroprotective effect and to investigate AdipoRon, an Orally Active, the possible underlying mechanism. Methods: We used two well-established mouse models of Synthetic Agonist of AdipoR1 and gastric ulcer (GU) induced by oral administration of EtOH (80% solution in water) or diclofenac AdipoR2 Receptors Has (30 mg/kg, p.o.). -

December 2016
Search “Santiam Flycasters” SANTIAM FLYCASTERS SANTIAMFLYCASTERS.COM December 2016 December Program — Thursday Dec. 8 Board Meeting Monday December 5 “Fly Fishing Photography 101: How to Capture What 7:00 pm You See” Garibaldi Family Restaurant With Carol Ann Morris General Meeting Over the past two decades Carol Ann Thursday December 8 Morris's photographs have not only Doors open at 6:00 appeared in most of her husband Skip Morris's 18 fly-fishing and -tying books but Meal at 6:30 pm on the covers and interior pages of such Pringle Community Center magazines as Grey's Sporting Journal and Fly Fishing & Tying Journal. Carol also speaks at fly clubs and fly-fishing shows. She has performed her PowerPoint show "Fly-Fishing Photography 101: How to Capture What You See" all over the West- In This Issue -in Washington, Oregon, British Columbia- -and in the East--Michigan, Ohio--at fly- Devil’s Lake Outing Report fishing clubs and sportsmen's shows and 2017 SFC Officers fly-fishing expositions. It seems fly fishers want to record their Fishing Detroit Lake biggest and most beautiful fish, the Pontoon Boat Raffle fascinating rivers and lakes and beaches they fish and explored--the very heart of Welcome to New Members joining their beloved sport--with a camera. Carol in November teaches them how to make their photos crisp and vivid, balanced and expressive. She demonstrates and explains the Rule of Thirds, effective use of light, the Magic Time to Renew Your Membership Hour, UFOs (Unidentified Foreign Objects), how to photograph fish, and many other straightforward concepts anyone can use to improve their photographs. -

Symposium ”Diabetes - a Threat to Mankind”
Symposium ”Diabetes - a Threat to Mankind” 7-8 June, 2013 in Helsinki, Finland The Finnish Diabetic Nephropathy Study Folkhälsan Institute of Genetics, Folkhälsan Research Center Biomedicum Helsinki 1, room C318 Haartmaninkatu 8 FI- 00290, Helsinki www.finndiane.fi Local Organizing Committee Per-Henrik Groop [email protected] tel. +358 9 191 25459 Carol Forsblom [email protected] tel. +358 40 5559556 Asta Mustonen [email protected] tel. +358 44 7883743 Maikki Parkkonen [email protected] tel. +358 9 19125387 Dear Participants, It is my great pleasure and honor to welcome you all to the “Diabetes – A Threat to Mankind” symposium held in Helsinki on June 7-8, 2013. This symposium will include presentations by a roster of award winning keynote speakers exploring both type 1 and type 2 diabetes and cover- ing topics ranging from disease pathogenesis to diabetic complications. This symposium was made possible by an unrestricted educational grant from the Wilhelm and Else Stockmann Foundation. Established in 1953 with the goal of promoting research that aims to prevent or ease the suffering caused by common complex diseases, the Wilhelm and Else Stockmann Foundation has played a major role in supporting dia- betes research in Finland. This symposium will serve to highlight both the 60th anniversary of the Foundation as well as the 15th Anniversary of the Finnish Diabetic Nephropathy Study. My sincere thanks go to all invited speakers and chairmen who, de- spite their busy schedules all agreed to come to Helsinki to share their knowledge and expertise with us. I am also indebted to all of you who accepted the invitation to take part in this event. -
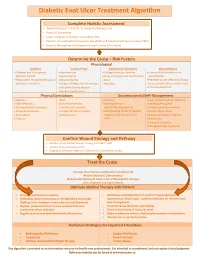
Diabetic Foot Ulcer Treatment Algorithm
Diabetic Foot Ulcer Treatment Algorithm Complete Holistic Assessment Medical/Surgical History & Co-morbidity Management Physical Examination Lower Leg (LLA) including monofilament test Perform Arterial Brachial Pressure Index (ABPI) and Toe Brachial Pressure Index (TBPI) Diabetic Management (Glycemic and Lipid Control & Nutrition) Determine the Cause – Risk Factors Physiological Diabetes Vascular Flow Autoimmune Disorders Wound History Diabetes and sub-optimal Hypertension Collagen vascular diseases History of foot infections or glycemic control Heart disease Immunosuppressant medications osteomyelitis Neuropathic changes with lack of Hyperlipidemia Gout Presence of toe infections (fungal protective sensation History of deep vein thrombosis Vasculitis or bacterial), callous and/or corns Peripheral artery disease Previous ulceration Venous Insufficiency Physical Limitations Socioeconomic/Self-Management Obesity Gait Smoking Lack of awareness for self-care Foot deformity Nutritional deficits Inadequate foot Inadequate hygiene Decreased level of activity Limited joint mobility wear/offloading devices Unsafe home environment Visual disturbances Congenital abnormalities Lack/Inability to afford diabetic Alcohol/drug abuse Amputation Osteoporosis supplies, foot care and foot Decreased Cognitive Ability Trauma wear Depression Financial insecurity Decreased level of activity Confirm Wound Etiology and Pathway Results of LLA, Monofilament Testing and ABPI/ TBPI Results of wound assessment Diagnostic -

Comparative Evaluation of Fructosamine and Hba1c As a Marker of Glycemic Control in Type 2 Diabetes: a Hospital Based Study
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Original Research Article Comparative Evaluation of Fructosamine and HbA1c as a Marker of Glycemic Control in Type 2 Diabetes: A Hospital Based Study Dr. Jyoti Goyal1, Dr. Nibhriti Das2, Dr. Navin Kumar3, Ms. Seema Raghav4, Dr. Paramjeet Singh Bhatia5, Dr. Karunesh Prasad Singh6, Dr. Sabari Das7 1DNB, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India- 281003, 2Ex-Director of Laboratory services and Additional Dean Research and Academics, Nayati Healthcare and Research Centre, Mathura, India- 281003, 3Ph.D, Biostatistitian, Department of Biostatistics, Nayati Healthcare and Research Centre, Mathura, India-281003. 4M.Sc., Certified Diabetes Educator, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India-281003. 5MD, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India-281003. 6MD Physician, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India-281003. 7Department of Laboratory Medicine, Nayati Healthcare and Research Centre, Mathura, India- 281003, Corresponding Author: Dr. Jyoti Goyal ABSTRACT Introduction: Management of type 2 diabetes revolves around achievement of target glycemic control with the help of antidiabetic drugs or insulin. There are various markers for measurement of glyceamic control like HbA1c, Mean Blood Glucose and fructosamine levels. Though HbA1c is a well validated standard method for assessment of glycemic control but it has also got certain limitations. Fructosamine, a less explored method may be used as an alternative marker for an assessment of glycemic control in cases where HbA1c is unreliable or unavailable. The objective of this study is to compare the fructosamine levels with HbA1c in assessment of glycemic control in type 2 diabetics so as to assess the utility of fructosamine as an alternative marker for evaluation of glucose control. -

Associations Between Nutrients and Foot Ulceration in Diabetes: a Systematic Review
nutrients Review Associations between Nutrients and Foot Ulceration in Diabetes: A Systematic Review Nada Bechara 1,2,3, Jenny E. Gunton 2,3,4,* , Victoria Flood 5,6 , Tien-Ming Hng 1 and Clare McGloin 1 1 Department of Diabetes and Endocrinology, Blacktown-Mt Druitt Hospital, Blacktown, NSW 2148, Australia; [email protected] (N.B.); [email protected] (T.-M.H.); [email protected] (C.M.) 2 Westmead Hospital, Sydney Medical School, Faculty of Medicine and Health, The University of Sydney, Westmead, NSW 2145, Australia 3 Centre for Diabetes, Obesity and Endocrinology Research (CDOER), The Westmead Institute for Medical Research, The University of Sydney, Westmead, NSW 2145, Australia 4 Garvan Institute of Medical Research, Darlinghurst, NSW 2010, Australia 5 Westmead Hospital, Research and Education Network, Western Sydney Local Health District, Westmead, NSW 2145, Australia; [email protected] 6 Faculty of Medicine and Health, Sydney School of Health Sciences, The University of Sydney, Camperdown, NSW 2006, Australia * Correspondence: [email protected] Abstract: We reviewed the literature to evaluate potential associations between vitamins, nutrients, nutritional status or nutritional interventions and presence or healing of foot ulceration in diabetes. Embase, Medline, PubMed, and the Cochrane Library were searched for studies published prior to September 2020. We assessed eligible studies for the association between nutritional status or interventions and foot ulcers. Fifteen studies met the inclusion criteria and were included in this Citation: Bechara, N.; Gunton, J.E.; review. Overall, there is a correlation between poor nutritional status and the presence of foot Flood, V.; Hng, T.-M.; McGloin, C. -

Acute Renal Failure in Patients with Type 1 Diabetes Mellitus G
Postgrad Med J: first published as 10.1136/pgmj.70.821.192 on 1 March 1994. Downloaded from Postgrad Med J (1994) 70, 192- 194 C) The Fellowship of Postgraduate Medicine, 1994 Acute renal failure in patients with type 1 diabetes mellitus G. Woodrow, A.M. Brownjohn and J.H. Turney Renal Unit, Leeds General Infirmary, Great George Street, Leeds LSJ 3EX, UK Summary: Acute renal failure (ARF) is a serious condition which still carries a mortality of around 50%. People with diabetes may be at increased risk of developing ARF, either as a complication of diabetic ketoacidosis or hyperosmolar coma, increased incidence of cardiovascular disease, or due to increased susceptibility ofthe kidney to adverse effects in the presence ofunderlying diabetic renal disease. During the period 1956-1992, 1,661 cases of ARF have been treated at Leeds General Infirmary. Of these, we have identified 26 patients also having type 1 diabetes. ARF due to diabetic ketoacidosis is surprisingly uncommon (14 cases out of 23 patients whose notes were reviewed). All cases of ARF complicating ketoacidosis in the last decade have been associated with particularly severe illness requiring intensive care unit support, rather than otherwise 'uncomplicated' ketoacidosis. We discuss the conditions that may result in ARF in patients with diabetes and the particular difficulties that may be encountered in management. Introduction People with diabetes may be at increased risk of Results developing acute renal failure (ARF). Acute pre- copyright. renal failure may occur as a result ofthe severe fluid Of 23 patients with type 1 diabetes complicated by depletion associated with diabetic ketoacidosis and ARF, diabetic ketoacidosis was the main underly- non-ketotic hyperosmolar coma. -

Effect of Biochemical Parameters Showing Atherogenicity in Type 2 Diabetic Nephropathy
International Journal of Basic and Applied Chemical Sciences ISSN: 2277-2073 (Online) An Online International Journal Available at http://www.cibtech.org/jcs.htm 2012 Vol. 2 (4) October-December pp.26-30/Raja and Shaker Research Article EFFECT OF BIOCHEMICAL PARAMETERS SHOWING ATHEROGENICITY IN TYPE 2 DIABETIC NEPHROPATHY *G. Raja and Ivvala Anand Shaker *Department of Biochemistry, Melmaruvathur Adhiparasakthi Institute of Medical Sciences and Research, Melmaruvathur-603319, Tamil Nadu, India *Author for Correspondence ABSTRACT Diabetic nephropathy is one of the major complications of diabetes mellitus characterized by frequent microalbuminuria, elevated arterial blood pressure, a persistent decline in glomerular filtration rate and a high risk of cardiovascular morbidity and mortality. The study comprised of 30 Diabetic mellitus (DM) with microalbuminuria patients (Group 3), 30 DM without microalbuminuria patients (group 2) compared with 30 healthy controls (Group 1). Fasting glucose, post prandial glucose, lipid profile, fructosamine and microalbuminuria were investigated in all the groups. The significant increase in serum fructosamine, fasting and post prandial glucose levels along with increased microalbuminuria observed in group 3 patients compared to group 2 and group 1 patients. Hyperglycemia, increased fructosamine and increased Cholesterol, triglycerides with decreased HDL-cholesterol levels indicates the major risk of atherogenicity. Key Words: Diabetic nephropathy, Microalbuminuria, Fructosamine and Atherogenicity INTRODUCTION Diabetes mellitus (DM) is a disease in which the hallmark feature is elevated blood glucose concentrations due to loss of insulin-producing pancreatic β-cells (type 1 diabetes) or through loss of insulin responsiveness in its target tissues (type 2 diabetes). Type 1 diabetes usually begins to manifest in childhood and early adulthood, but type 2 diabetes is typically a disease for which increased age is a risk factor (Schwarz, 2009). -

Acanthocytes in the Urine Useful Tool to Differentiate Diabetic Nephropathy from Glomerulonephritis?
Pathophysiology/Complications ORIGINAL ARTICLE Acanthocytes in the Urine Useful tool to differentiate diabetic nephropathy from glomerulonephritis? GUNNAR H. HEINE, MD MATTHIAS GIRNDT, MD of patients who are most likely to have a URBAN SESTER, MD HANS K¨OHLER, MD nondiabetic glomerulopathy and to selec- tively perform renal biopsy in this sub- group of patients. Urinary erythrocyte morphology ex- amined by phase-contrast microscopy al- OBJECTIVE — The presence of hematuria has been suggested to indicate nondiabetic ne- lows to differentiation of glomerular and phropathy in diabetic patients with proteinuria. However, hematuria is frequently found in patients with biopsy-proven diabetic glomerulosclerosis without nondiabetic nephropathy. nonglomerular bleeding (10). Glomeru- Urine microscopy allows discrimination of glomerular hematuria, which is defined as acantho- lar bleeding is indicated by urinary excre- cyturia (urinary excretion of acanthocytes, which are dysmorphic erythrocytes with vesicle-like tion of acanthocytes. Acanthocytes are protrusions), from nonglomerular hematuria. We hypothesized that acanthocyturia is an un- characteristic ring-formed erythrocytes common finding in diabetic nephropathy, which suggests the presence of a nondiabetic ne- with vesicle-shaped protrusions (Fig. 1) phropathy in diabetic patients with proteinuria. (11,12) that have been described previ- ously in the peripheral blood of patients RESEARCH DESIGN AND METHODS — Urine samples of patients with the clinical diagnosis of diabetic nephropathy (n ϭ 68), of patients with biopsy-proven glomerulonephritis suffering from certain hereditary neuro- (n ϭ 43), and of age-matched healthy control subjects (n ϭ 20) were examined by phase-contrast logical disorders (abetalipoproteinemia, microscopy for the presence of hematuria (Ն8 erythrocytes/l) and acanthocyturia. Acantho- chorea-acanthocytosis, and McLeod syn- cyturia of Ն5% (5 acanthocytes among 100 excreted erythrocytes) was classified as glomerular drome) (13).