Amrids/JICA Project - Field Visit - Trip Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Lupinus Albus L.) Landraces
AJCS 11(1):55-62 (2017) ISSN:1835-2707 doi: 10.21475/ajcs.2017.11.01.pne226 Genotype by trait biplot analysis to study associations and profiles of Ethiopian white lupin (Lupinus albus L.) landraces Mulugeta Atnaf*, Kassahun Tesfaye, Kifle Dagne and Dagne Wegary Supplementary Table 1: Ethiopian white lupin landraces considered for the study. (a). Ethiopian white lupin landraces considered for the first study EBI EBI Acc no code Zone District Altitude Acc no code Zone District Altitude Acc1 242279 Awi Ankesha 2310 Acc37 238993 BD Sp Bahir dar 1990 Acc2 242280 Awi Ankesha 2185 Acc38 238994 BD Sp Bahir dar 2020 Acc3 242281 Awi Ankesha 2310 Acc39 239011 BD Sp Bahir dar 2090 Acc4 242282 Awi Ankesha 2410 Acc40 239020 BD Sp Bahir dar 1940 Acc5 242266 WG Dembecha 2110 Acc41 239022 BD Sp Bahir dar 1930 Acc6 239044 Awi Banja 2600 Acc42 239023 BD Sp Bahir dar 1930 Acc7 242277 Awi Banja 2560 Acc43 228519 SG Dera Acc8 242278 Awi Banja 2560 Acc44 242311 SG Dera 1860 Acc9 242283 Awi Banja 2160 Acc45 242312 SG Dera 1960 Acc10 242284 Awi Banja 1960 Acc46 242313 SG Dera 1960 Acc11 236619 Awi Banja 2570 Acc47 242314 SG Dera 2160 Acc12 239045 Awi Banja 2600 Acc48 242315 SG Dera 2380 Acc13 242273 Awi Banja 2490 Acc49 242316 SG Dera 2460 Acc14 242274 Awi Banja 2450 Acc50 242268 WG Dembecha 2010 Acc15 242276 Awi Banja 2590 Acc51 239018 WG BD Z 1950 Acc16 105018 Acc52 242319 SG Dera 2510 Acc17 105005 Awi Dangila 1940 Acc53 105002 SG Este 2420 Acc18 228520 Awi Dangila Acc54 226034 SG Este 2560 Acc19 242290 Awi Dangila 2240 Acc55 242321 SG Este 2630 Acc20 242291 -

The Ethiopian Journal of Social Sciences Volume 7, Number 1, May 2021
The Ethiopian Journal of Social Sciences Volume 7, Number 1, May 2021 The 2016 Mass Protests and the Responses of Security Forces in ANRS, Ethiopia: Awi and West Gojjam Zones in Focus 1Kidanu Atinafu Abstract This study examined security forces’ abuse of power and their accountability in connection with the 2016 mass protests that unfolded in the Amhara National Regional State (ANRS) in general and Awi and West Gojjam Zones in particular. Specifically, the study assessed the nature of the use of force and the consequent investigations to punish security forces who abused their power. To address these objectives, the study employed a mixed methods research approach with a concurrent parallel design. Data for this research was obtained both from primary and secondary data sources. Interview, questionnaire and document analysis were used to collect data. A sample of 384 respondents was selected randomly to complete the questionnaire, whereas key informants were selected for the interview through snowball sampling technique. Based on the data gathered from all these sources, the study revealed that security forces committed arbitrary and extrajudicial killings and inflicted injuries against protesters who were chiefly unarmed and non-violent. The measures taken were found excessive and arbitrary with several civilians risking their lives and physical wellbeing. With few exceptions, the administrations at different levels of the government failed to investigate these extrajudicial and arbitrary killings and injuries inflicted in the process of punishing alleged perpetrators of the protest using civil and criminal laws. It is finally recommended to undertake independent investigations into the legitimacy of the murders, injuries, beatings and other forms of violence committed by the security forces. -
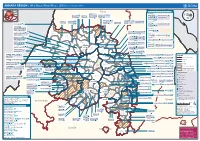
AMHARA REGION : Who Does What Where (3W) (As of 13 February 2013)
AMHARA REGION : Who Does What Where (3W) (as of 13 February 2013) Tigray Tigray Interventions/Projects at Woreda Level Afar Amhara ERCS: Lay Gayint: Beneshangul Gumu / Dire Dawa Plan Int.: Addis Ababa Hareri Save the fk Save the Save the df d/k/ CARE:f k Save the Children:f Gambela Save the Oromia Children: Children:f Children: Somali FHI: Welthungerhilfe: SNNPR j j Children:l lf/k / Oxfam GB:af ACF: ACF: Save the Save the af/k af/k Save the df Save the Save the Tach Gayint: Children:f Children: Children:fj Children:l Children: l FHI:l/k MSF Holand:f/ ! kj CARE: k Save the Children:f ! FHI:lf/k Oxfam GB: a Tselemt Save the Childrenf: j Addi Dessie Zuria: WVE: Arekay dlfk Tsegede ! Beyeda Concern:î l/ Mirab ! Concern:/ Welthungerhilfe:k Save the Children: Armacho f/k Debark Save the Children:fj Kelela: Welthungerhilfe: ! / Tach Abergele CRS: ak Save the Children:fj ! Armacho ! FHI: Save the l/k Save thef Dabat Janamora Legambo: Children:dfkj Children: ! Plan Int.:d/ j WVE: Concern: GOAL: Save the Children: dlfk Sahla k/ a / f ! ! Save the ! Lay Metema North Ziquala Children:fkj Armacho Wegera ACF: Save the Children: Tenta: ! k f Gonder ! Wag WVE: Plan Int.: / Concern: Save the dlfk Himra d k/ a WVE: ! Children: f Sekota GOAL: dlf Save the Children: Concern: Save the / ! Save: f/k Chilga ! a/ j East Children:f West ! Belesa FHI:l Save the Children:/ /k ! Gonder Belesa Dehana ! CRS: Welthungerhilfe:/ Dembia Zuria ! î Save thedf Gaz GOAL: Children: Quara ! / j CARE: WVE: Gibla ! l ! Save the Children: Welthungerhilfe: k d k/ Takusa dlfj k -

Determinants of Maize Market Supply, Production and Marketing Constraints: the Case of Dembecha District, West Gojjam Zone, Ethiopia
International Journal of Economy, Energy and Environment 2020; 5(5): 83-89 http://www.sciencepublishinggroup.com/j/ijeee doi: 10.11648/j.ijeee.20200505.13 ISSN: 2575-5013 (Print); ISSN: 2575-5021 (Online) Determinants of Maize Market Supply, Production and Marketing Constraints: The Case of Dembecha District, West Gojjam Zone, Ethiopia Desalegn Wondim 1, *, Tewodros Tefera 2, Yitna Tesfaye 2 1Department of Agribusiness and Value Chain Management, Burie Campus, Debre Markos University, Burie, Ethiopia 2School of Environment, Gender and Development Studies, Hawassa University, Hawassa, Ethiopia Email address: *Corresponding author To cite this article: Desalegn Wondim, Tewodros Tefera, Yitna Tesfaye. Determinants of Maize Market Supply, Production and Marketing Constraints: The Case of Dembecha District, West Gojjam Zone, Ethiopia. International Journal of Economy, Energy and Environment . Vol. 5, No. 5, 2020, pp. 83-89. doi: 10.11648/j.ijeee.20200505.13 Received : July 22, 2020; Accepted : August 31, 2020; Published : October 7, 2020 Abstract: West Gojjam is one of the maize belt zones in Ethiopia, and Dembecha district is among the potential districts in West Gojjam zone. However, despite its maize production potential of the district, marketed supply determinants, maize production and marketing constraints hampered producer’s decision and engagement on maize production and marketing. Thus, this study was attempts to address the determinants of marketed supply of maize, constraints and opportunities in Dembecha district in the year 2018. Data were collected from primary and secondary sources using appropriate tools. Primary data were collected from randomly selected 155 maize producers, 20 consumers as well as 40 maize grain traders, 10 alcohol processors using semi-structured questionnaire. -

Ethiopia: Amhara Region Administrative Map (As of 05 Jan 2015)
Ethiopia: Amhara region administrative map (as of 05 Jan 2015) ! ! ! ! ! ! ! ! ! ! Abrha jara ! Tselemt !Adi Arikay Town ! Addi Arekay ! Zarima Town !Kerakr ! ! T!IGRAY Tsegede ! ! Mirab Armacho Beyeda ! Debark ! Debarq Town ! Dil Yibza Town ! ! Weken Town Abergele Tach Armacho ! Sanja Town Mekane Berhan Town ! Dabat DabatTown ! Metema Town ! Janamora ! Masero Denb Town ! Sahla ! Kokit Town Gedebge Town SUDAN ! ! Wegera ! Genda Wuha Town Ziquala ! Amba Giorges Town Tsitsika Town ! ! ! ! Metema Lay ArmachoTikil Dingay Town ! Wag Himra North Gonder ! Sekota Sekota ! Shinfa Tomn Negade Bahr ! ! Gondar Chilga Aukel Ketema ! ! Ayimba Town East Belesa Seraba ! Hamusit ! ! West Belesa ! ! ARIBAYA TOWN Gonder Zuria ! Koladiba Town AMED WERK TOWN ! Dehana ! Dagoma ! Dembia Maksegnit ! Gwehala ! ! Chuahit Town ! ! ! Salya Town Gaz Gibla ! Infranz Gorgora Town ! ! Quara Gelegu Town Takusa Dalga Town ! ! Ebenat Kobo Town Adis Zemen Town Bugna ! ! ! Ambo Meda TownEbinat ! ! Yafiga Town Kobo ! Gidan Libo Kemkem ! Esey Debr Lake Tana Lalibela Town Gomenge ! Lasta ! Muja Town Robit ! ! ! Dengel Ber Gobye Town Shahura ! ! ! Wereta Town Kulmesk Town Alfa ! Amedber Town ! ! KUNIZILA TOWN ! Debre Tabor North Wollo ! Hara Town Fogera Lay Gayint Weldiya ! Farta ! Gasay! Town Meket ! Hamusit Ketrma ! ! Filahit Town Guba Lafto ! AFAR South Gonder Sal!i Town Nefas mewicha Town ! ! Fendiqa Town Zege Town Anibesema Jawi ! ! ! MersaTown Semen Achefer ! Arib Gebeya YISMALA TOWN ! Este Town Arb Gegeya Town Kon Town ! ! ! ! Wegel tena Town Habru ! Fendka Town Dera -

Ethiopian Flags and History)
Ethiopian Constitution, the Flag, Map, and Federalism by Mastewal There have been contentions to the Ethiopian present constitution and even the flag and its administrative arrangement in the way it is governed federally. In the forefront of these oppositions have been the political parties and the Ethiopian diaspora, who have been airing their concerns. Some, who oppose the present flag, are seen with the flag used during the Emperor Haile Selassie’s rule with the lion carrying the cross. Some use the civil flag of Ethiopia. Why changes have been made in the Ethiopian flag and its administrative regions have their historical backgrounds. But, the argument goes on and on as pros and cons in fear of disintegration of the country. The contentions can be damaging if the struggle for changing the above if not made in a civilized way and go out of hand as evidenced in some instances. Innocents can be incited to adopt radical changes. If you remember Aesop, the Greek fabulist and storyteller in your school time, then you come across in what he is presumed to have said, “the injuries we do and those we suffer are seldom weighted in the same scales.” I just want to quote George M. Church in respect to changes. He is taking the comparison between a dinosaur and ostrich. As you all know dinosaur is an extinct creature, which lived in our world over hundred millions years ago. May be the dinosaur evolved to an ostrich. “What dinosaur traits are missing from an ostrich? The ostrich has a toothless beak, but there are mutations that cause teeth and claws to come back to their mouth and limbs. -

Narratives of Environmental Disaster in Ethiopia: the Political Ecology of Famine
Narratives of Environmental Disaster in Ethiopia: The Political Ecology of Famine By Abeal Biruk Supervised by Dr. Nirupama Agrawal A Major Paper submitted to the Faculty of Environmental Studies in partial fulfilment of the requirements for the degree of Master in Environmental Studies York University, Toronto, Ontario Canada July 31st, 2020 Abstract: The conception and inheritance of narratives are an important component of being human. At the foundation of many societies, narratives take shape through verbal and written stories, songs, artifacts, records of events, testimonials, and even memories. These narratives are carried forward to the next generation in the hopes of remembering and educating those who look to the past to understand their present and future environments. Despite ethnic and cultural differences, groups of people find ways to preserve the narratives that can either form or unite their identities together. This statement by no means disparages the impact of historical forces, such as European colonialism, that has tampered the narratives of countless Indigenous groups in North America, the Global South and Africa. The pursuit of identifying narratives can aid in the unravelling of so-called truths of history, seeking justice for people who can no longer do so themselves, and healing generations of systematic oppression in countless broken communities. Ethiopia has spent over a century facing significant drought conditions that have rendered many of the nation’s northern regions vulnerable to famine. For this reason, this paper focuses on the impacts of anthropogenic environmental disasters in Ethiopia, specifically the famine of 1983- 1985. The goal of this research is to analyze the 1983-1985 famine to understand its significance in relation to contemporary Ethiopian disaster management. -

AMHARA Demography and Health
1 AMHARA Demography and Health Aynalem Adugna January 1, 2021 www.EthioDemographyAndHealth.Org 2 Amhara Suggested citation: Amhara: Demography and Health Aynalem Adugna January 1, 20201 www.EthioDemographyAndHealth.Org Landforms, Climate and Economy Located in northwestern Ethiopia the Amhara Region between 9°20' and 14°20' North latitude and 36° 20' and 40° 20' East longitude the Amhara Region has an estimated land area of about 170000 square kilometers . The region borders Tigray in the North, Afar in the East, Oromiya in the South, Benishangul-Gumiz in the Southwest and the country of Sudan to the west [1]. Amhara is divided into 11 zones, and 140 Weredas (see map at the bottom of this page). There are about 3429 kebeles (the smallest administrative units) [1]. "Decision-making power has recently been decentralized to Weredas and thus the Weredas are responsible for all development activities in their areas." The 11 administrative zones are: North Gonder, South Gonder, West Gojjam, East Gojjam, Awie, Wag Hemra, North Wollo, South Wollo, Oromia, North Shewa and Bahir Dar City special zone. [1] The historic Amhara Region contains much of the highland plateaus above 1500 meters with rugged formations, gorges and valleys, and millions of settlements for Amhara villages surrounded by subsistence farms and grazing fields. In this Region are located, the world- renowned Nile River and its source, Lake Tana, as well as historic sites including Gonder, and Lalibela. "Interspersed on the landscape are higher mountain ranges and cratered cones, the highest of which, at 4,620 meters, is Ras Dashen Terara northeast of Gonder. -

Ethiopian and Eritrean Askaris in Libya (1911- 1932) Dechasa Abebe1
Ethiopian Journal of the Social Sciences and Humanities (EJOSSAH) ISSN (online): 2520-582X ISSN (print): 1810-4487 Ethiopian and Eritrean Askaris in Libya (1911- 1932) Dechasa Abebe1 Abstract A number of books and articles were published on the three consecutive Italian wars in Libya and its resistances during the first three decades of the twentieth century. However, the role and experiences of the Ethiopian and Eritrean askaris were rarely studied. Thus, this article is an attempt to disclose their role in the wars, why they were interested in being employed by the Italians and why Italy relied heavily on them instead of the Italian soldiers and the Libyan askaris. Historical sources, like the memoires of Italian military commanders and the askaris, travellers’ accounts mainly that of journalists, correspondence documents, and popular songs particularly that of Tigrigna were consulted to write this article. Moreover, publications produced by military historians on the Italian wars in Libya were also referred. While starvation and famines, poverty, unemployment and maladministration were the driving force from Eritrea and Ethiopia; salary, military uniform, guns and bullets, rations, protections and relative freedom were some of the attractions from the Italian side for the Ethiopians and Eritreans to be employed as askaris. In relation to these, political expediency or loss aversion, cost, fighting skill and courage, adaptability to Libyan topography and loyalty were some of the qualities of Ethiopians and Eritrean askaris that initiated the Italians to rely on. As a result, about 68 battalions fought in the wars. In the process, the askaris were identified by their Italian commanders as “warlike race” and best soldiers in contrast to the Italian soldiers and Libyan collaborators. -

The Battle for the Battle of Adwa: Collective Identity and Nation- Building
City University of New York (CUNY) CUNY Academic Works Dissertations and Theses City College of New York 2020 The Battle For The Battle of Adwa: Collective Identity and Nation- Building Joseph A. Steward CUNY City College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/cc_etds_theses/836 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] The Battle for The Battle of Adwa: Collective Identity and Nation-Building Joseph Steward May 2020 Master’s Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of International Affairs at the City College of New York COLIN POWELL SCHOOL FOR CIVIC AND GLOBAL LEADERSHIP Thesis Advisor: Professor Nicolas Rush Smith Second Reader: Professor Jean Krasno “I beg your majesty to defend me against everyone as I don’t know what European kings will say about this. Let others know that this region is ours.” - Emperor Menelik II Abstract On March 1st, 1896, an Ethiopian army lead by Emperor Menelik II dealt a shocking defeat to the invading Italian forces in the Battle of Adwa. In victory, Menelik was able to exert his authority over a vast territory which included both the historical, ancient kingdoms of the northern and central parts of Ethiopia, and also the vast, resource-rich territories in the west and south which he had earlier conquered. The egalitarian nature of the victory united the various peoples of Ethiopia against a common enemy, giving Menelik the opportunity to create a new Ethiopian nation. -

The Horn of Africa: Regional Conflict and Super Power Involvement
CANBERRA TO PERS ON STRATEGY AND DEFENCE "N O . 18 ) / MOHAMMED AYOOB The Horn of Africa: Regional Conflict and Super Power Involvement Canberra Papers on Strategy and Defence The Horn of Africa Regional Conflict and Super Power Involvement Mohammed Ayoob A publication of The Strategic and Defence Studies Centre The Research School of Pacific Studies The Australian National University Canberra 1978 Printed and Published in Australia at the Australian National University 1978 © 1978. Mohammed Ayoob This book is copyright. Apart from any fair dealing for the purposes of private study, research, criticism, or review as permitted under the Copyright Act, no part may be reproduced by any process without written permission. National Library of Australia Cataloguing-in-Publication entry Ayoob, Mohammed, 1942- The Horn of Africa: Regional Conflict and Super Power Involvement. (Canberra papers on strategy and defence; no. 18). ISBN 0 909851 19 0 1. East Africa — Foreign relations. 2. Intervention (International law). I. Title. (Series). 327’.67 Designed by ANU Graphic Design Printed by Central Printing The Strategic and Defence Studies Centre, Research School of Pacific Studies, The Australian National University, Box 4 PO, Canberra ACT 2600. Regional rivalries in the Horn of Africa have been intense for many centuries but never has there been such a clash between neighbours as the present full- scale war between Ethiopia and Somalia. However this conflict is more than simply a local war between neighbours because of the involvement of the superpowers, the U.S.A. and the U.S.S.R., and several other regional powers. Furthermore it is a contest replete with dramatic changes and sudden switches of allegiance such as the shattering of the close military relationship between Ethiopia and the U.S.A., the expulsion of the Soviets from Somalia and the substantial military support given by the U.S.S.R. -

The Two-Faced Amhara Identity
Siegfried Pausewang Chr. Michelsen Institute Bergen THE TWO-FACED AMHARA IDENTITY In the St. Petersburg Journal of African Studies, the late Sevir B. Cherne- tsov published in 1993 a remarkable article which, even more remarkably, was not noticed by the majority of scholars on Ethiopia. To my knowledge, not a single serious academic comment underscored its main thesis or its important historical and political significance. And no later publication on relevant issues I know of has quoted the article or indeed given S. Chernetsov credit for his contribution through referencing it. Even Tronvoll and Vaug- han, who in their Culture of Power1 describe in some detail the difference between urban Amhara identity and rural ethnic Amhara culture, do not men- tion Chernetsov in their reference list. The article by S. Chernetsov, entitled «On the Origins of the Amhara»,2 described Amhara culture as a culture of assimilation. The language and the culture of the Imperial Court was Amharic since the reign of Yekunno Amlak and, through him, the «Solomonic line» of kings emanating from the historic- al Amhara province. S. Chernetsov observes that today the Amhara are counted as the second largest ethnic group in Ethiopia, much more populous than what the tiny province of Amhara could be expected to procreate. This is because whoever wanted to advance in the court, the administration or in the military of the Emperors had to speak Amharic reasonably well and usually also had to adopt the Orthodox Christian religion. The court retained an Amhara culture, but attracted ambitious and bright individuals from other ethnic groups, provided they volunteered to adopt the language, the religion and the customs at the court.