Clinical Findings and Management of Myopia Control and Orthokeratology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Enhance Your SMILE with Orthokeratology: a Case Report on the Use of Orthokeratology to Treat Myopia Regression After SMILE Surgery
Enhance your SMILE with Orthokeratology: A Case Report on the Use of Orthokeratology to Treat Myopia Regression After SMILE Surgery Shuyi (Suzy) Chen*, Elton Wong, Sharon P. Keh OD FAAO BACKGROUND Patient was motivated to pursue orthokeratology to address her declining distance acuity DISCUSSION Despite recent advancements in laser refractive procedures, including the Fitting post-refractive surgical patients with orthokeratology can be challenging OS, as she had worn Paragon CRT® lenses prior to SMILE surgery. introduction of small-incision lenticule extraction (SMILE), some post- because of their iatrogenic, oblate corneal shape. In this case, proper centration, refractive surgery patients still experience myopic regression over time. While fluorescein pattern, and desired myopia reduction were achieved with the the mechanism of regression following refractive treatment is not fully Lens 1 (Initial Lens) customization of a Paragon CRT Dual Axis® lens. This case study also investigated understood, the process is clearly multifactorial, involving the corneal Based on patient’s refraction and topography, the following Paragon CRT Dual Axis ® lens 1 the effect of orthoK treatment on additional factors which may affect visual epithelium and stroma. was ordered empirically with consultation. performance. At each follow up visit of the final lens, patient’s contrast sensitivity was assessed with Pelli-Robson contrast sensitivity chart and corneal aberrations Amongst numerous treatment modalities for myopia, orthokeratology BC RZD LZA Diameter were measured on the OPD-Scan III Wavefront Aberrometer. (orthoK) is capable of satisfying patients’ visual needs with low risk, thereby Lens 1 9.40 475/550 31 11.0 benefiting the same group of highly motivated potential refractive surgery Lens 3 (Final lens) candidates. -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Diagnostic Tools for Dry Eye Disease
Review Ocular Surface Disease Diagnostic Tools for Dry Eye Disease Sarah Dougherty Wood and Shahzad I Mian Department of Ophthalmology and Visual Sciences, Medical School, University of Michigan, Ann Arbor, Michigan, US DOI: https://doi.org/10.17925/EOR.2016.10.02.101 ry eye disease is multifactorial in aetiology and complex in pathophysiology that makes its diagnosis clinically challenging. Although there are numerous tools for assessment of dry eye disease, no single test is sufficient for the diagnosis. Typically a combination of D subjective symptoms and objective tests are used. The aim of this article is to review the available tests, including traditional tools and emerging technologies. This review includes a description of the test methodology, type of data collected, diagnostic reliability of data, benefits and limitations of each test, expected outcomes and tips for practical application. Keywords The International Dry Eye Workshop Dry Eye Workshop (DEWS) defined dry eye as “a multifactorial Dry eye disease, dry eye diagnosis, tear film disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear film instability with potential damage of the ocular surface. It is accompanied by increased Disclosure: Sarah Dougherty Wood and Shahzad I Mian osmolarity of the tear film and inflammation of the ocular surface”.1 This condition is divided into do not have financial or proprietary interest in any materials or methods mentioned. No funding was two general types: deficient aqueous production by the lacrimal gland and increased evaporation received in the publication of this article. This study of the tear film, with the latter being more prevalent. -

Cataract Surgery Co-Management Information
Cataract Surgery Co-Management Phacoemulsification, Clear-Lens Extraction, and LensX INCLUSION CRITERIA: Significant visual complaints (decreased VA, increased glare, decreased Activities of Daily Living [ADLs], etc.) Treatment of secondary ocular disease (phacomorphic glaucoma, uveitis) Management of ocular disease (diabetic retinopathy, etc.) The patient’s Snellen best-corrected visual acuity must be 20/50 or worse. They may also be eligible for surgery if their BCVA is 20/40 or better and have significant difficulty with glare. Complaints of glare should be confirmed by brightness acuity testing or another suitable diagnostic test. EXCLUSION CRITERIA: Patients who are unable to receive proper postoperative care Patients in poor overall health (Primary Care Physician will not clear patient for surgery) TYPES OF CATARACT PATIENTS: Congenital: If cataract obscures visual axis (> or equal to 3mm) or is causing secondary disease, extraction should be performed within days to weeks after diagnosis in infants and small children to prevent amblyopia. If the cataract is not causing complications, closely observe for progression. Often patients with visually-significant, unilateral, congenital cataracts have strabismus and may require muscle surgery after extraction. Acquired: Most often, senile (Nuclear sclerosis, cortical degeneration, subcapsular) Due to systemic disease: (not limited to those listed below) Diabetes Mellitus Hypocalcemia Myotonic Dystrophy Frabry’s Disease Down’s Syndrome Atopic Dermatitis Wilson’s Disease -

Slit-Lamp Examination of the Vitreous and the Fundus* by H
Br J Ophthalmol: first published as 10.1136/bjo.33.4.242 on 1 April 1949. Downloaded from 242 H. GOLDMANN REFERENCES ANGELUCCI (1905).-Encycloqedie fran9aise. BAILLIART and BIDAULT (1939).-In Traiti d'Ophtalmologie, 8. Masson. COLLE, DUKE-ELDER, P. M., and DUKE-ELDER, W. S. (1931).-Jl. Physiol., 71, 1. COLOMBO (1923).-Boll. d'Ocul., 2. ;CRISTINI, G. (1947) -Ann. d'Ocul., 80, 530. (1948).-Gior. Ital. Oftal., 1, 5. (1948).-ibid., 1, 385. DIETER (1925).-Arch. f. A ugenhesilk., 96, 179 264. DUKE-ELDER, W. S. (1938).-Text-Book of Ophthalmology, Kimpton. DUKE-ELDER, W. S. and DAVSON, H. (1948).-Brit. Ji. Ophthal., 32, 555, ELSCHNIG.-Henke Lubarsch, 11, 911. FORTIN (1929).-Arch. d'Oftal., B.A., 359, 454. (1939).-Semana Medica., 1, 1128. GALA (1939).-Quoted by Magitot in Tratt d'Ophtalmologie, 6, 264. Masson. HAMBURGER (1923).-Med. Klin., 19, 1215. (1924).-lbid., 20, 267, (1925).-Ibid., 21, 1495, IiENDERSON and STARLING (1904).-Jl. Physiol., 31, 305. v. HIPPEL and GRUENHAGEN (1868).-Arch. f. Ophthal., 14,219. KOELLNER (1916).-Arch. f. Augenheilk., 80, 245. KUESEL (1906).-Klin. Monatsbl. f. Augenheilk., 44, 80, 236. LUCIANI-Fisiologia dell'uomo, 1, 381. MAGITOT (1939).-Traite d'Ophtalmologie, 11. Masson. MICHAIL and VANCEA (1926).-Ann. d'Ocul., 126, 561, PARSONS (1902).-The Pathology of the Eye. London. Poos (1931).-Arch. f. Ophthal., 127, 489. STOCKER (1947).-Arch. Ophthal., 37, 583. THIEL (1924).-Zentralbl. f. d. ges. Ophthal., 12, 305. Kurzes Handb,f. Oihthal. (Glaukom.), 781. THOMASSEN (i947).-Acta Ophthal., 25, 221. copyright. - (1947).-Ibid., 25,252. WEBER (1877).-Arch. f. Ophthal., 23, 1. -
Intraocular Lenses and Spectacle Correction
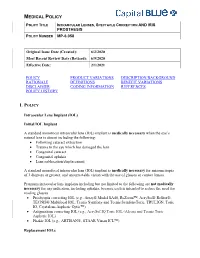
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

Orthokeratology on Patient with Ectasic Cornea
DOI 10.5935/0034-7280.20190154 CASE REPORT 327 Orthokeratology on patient with ectasic cornea Ortoceratologia no paciente com córnea ectásica Brunno Dantas1 https://orcid.org/0000-0003-3993-5244 Mylene Leal Matsuhara2 https://orcid.org/0000-0002-3539-3444 Leonardo Simões Duarte3 https://orcid.org/0000-0001-6133-9284 ABSTRACT A 26-year-old man, single, business student, reveals a ectasic cornea during corneal topography exam. Among some procedures, the patient chose Orthokeratology to do a corneal reshape and got successfully a good visual acuity, going against the most authors guidance. Keywords: Keratoconus/diagnosis; Orthokeratologic procedures; Orthokeratology; Ectasic cornea RESUMO Estudante de 26 anos, masculino, estudante de economia, apresentou ao exame topográfico de córneas, ectasia corneal. Dentre todos os procedimentos apresentados, optou pela ortoceratologia para o remodelamento corneal, e obteve sucesso com melhora da acuidade visual, indo contra a orientação da maioria dos autores. Descritores: Ceratocone/diagnóstico; Procedimentos ortoceratológicos; Ortoceratologia; Córnea ectásica 1 Contact Lenses Department, Hospital Federal dos Servidores do Estado, Rio de Janeiro, RJ, Brazil. 2 Santa Casa de Belo Horizonte, Belo Horizonte, MG, Brazil. 3 CEMA, São Paulo, SP, Brazil. Institution of the Scientific Study: Hospital Federal dos Servidores do Estado, Rio de Janeiro, RJ, Brazil. The authors declare no conflicts of interests. Received for publication 24/04/2017 - Accepted for publication 12/07/2019. Rev Bras Oftalmol. 2019; 78 (5): 327-9 328 Dantas B, Matsuhara ML, Duarte LS INTRODUCTION Why Orthokeratology has been forbidden for ectasic cornea?(1-7) That´s the question. If we avoid a touch on the surface vernight Orthokeratology (Ortho-K), corneal reshaping of the cornea apex, perhaps it will be possible to have a good result or vision-shaping treatment (usually generically referred in some cases. -

CAUSES, COMPLICATIONS &TREATMENT of A“RED EYE”
CAUSES, COMPLICATIONS & TREATMENT of a “RED EYE” 8 Most cases of “red eye” seen in general practice are likely to be conjunctivitis or a superficial corneal injury, however, red eye can also indicate a serious eye condition such as acute angle glaucoma, iritis, keratitis or scleritis. Features such as significant pain, photophobia, reduced visual acuity and a unilateral presentation are “red flags” that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features to know which patients require referral to an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? inflammation of the choroid (choroiditis). Complications include glaucoma, cataract and macular oedema. The most likely cause of a red eye in patients who present to 4. Scleritis is inflammation of the sclera. This is a very rare general practice is conjunctivitis. However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease, e.g. rheumatoid arthritis. treatment due to a missed diagnosis can result in permanent 5. Penetrating eye injury or embedded foreign body; red visual loss. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes to antimicrobial 6. Acid or alkali burn to the eye resistance. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access to specialised or chemical burn to the eye, but further assessment may be equipment for eye examination, e.g. -

Refractive Errors
Refractive Errors - Epidemiology & Risk Factors (("refractive errors/epidemiology"[MAJR:noexp]) OR ("refractive errors/ethnology"[MAJR:noexp]) OR (hyperopia/epidemiology[MAJR:noexp]) OR (hyperopia/ethnology[MAJR:noexp]) OR (myopia/epidemiology[MAJR:noexp]) OR (myopia/ethnology[MAJR:noexp]) OR (astigmatism/epidemiology[MAJR:noexp]) OR (astigmatism/ethnology[MAJR:noexp]) OR (presbyopia/epidemiology[MAJR:noexp]) OR (presbyopia/ethnology[MAJR:noexp])) ((Refractive Errors[MAJR:noexp]) OR (Hyperopia[MAJR:noexp]) OR (Myopia[MAJR:noexp]) OR (Astigmatism[MAJR:noexp]) OR (Presbyopia[MAJR:noexp])) AND (Prevalence[MeSH Terms) ((Refractive Errors[MAJR:noexp]) OR (Hyperopia[MAJR:noexp]) OR (Myopia[MAJR:noexp]) OR (Astigmatism[MAJR:noexp]) OR (Presbyopia[MAJR:noexp])) AND (Risk Factors[MeSH Terms]) (("myopia/epidemiology"[MeSH Terms]) OR (("myopia"[MeSH Terms]) AND ("risk factors"[MeSH Terms]))) AND ((reading[tiab]) OR (near work[tiab]) OR (nearwork[tiab]) OR (cylinder power[tiab]) OR (optical power[tiab]) OR (accommodation[tiab])) (refractive error*[tiab] OR hyperopia[tiab] OR myopia[tiab] OR astigmatism[tiab] OR presbyopia[tiab]) AND (epidemiolog*[tiab] OR ethnolog*[tiab] OR prevalen*[tiab] OR risk factor*[tiab]) (myopia[tiab]) AND (reading[tiab] OR nearwork[tiab] OR near work[tiab]) Diagnosis – Reproducibility of Results ("refractive errors/diagnosis"[MAJR]) AND ("reproducibility of results"[MeSH Terms]) (refractive error*[tiab] OR hyperopia[tiab] OR myopia[tiab] OR astigmatism[tiab] OR presbyopia[tiab]) AND (diagnos*[tiab] OR reproducib*[tiab]) -

JSZ Orthokeratology (Oprifocon A) Contact Lenses for Overnight Wear
JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear IMPORTANT: The following basic information about contact lens wear and JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear is provided for you. If you are interested in JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear, please see a licensed eye care professional trained and certified in fitting the product. Based on your individual needs, your certified professional will determine if JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear are right for you. What are .JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear? JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear are a unique rigid gas permeable contact lens design that temporarily corrects myopia (nearsightedness) by gently reshaping your cornea while you sleep. You may then be able to go throughout the day without any lenses. JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear is made from an approved extended wear contact lens material in a special design intended for this purpose. Can everyone wear JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear? Not everyone can wear JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear. These lenses are intended for individuals with low to moderate myopia (nearsightedness up to -5 diopters) and moderate astigmatism (1.50 diopters or less). How likely is it that JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear will work for me? Of the 210 eyes that completed the study with complete efficacy data (core cohort), 73% obtained 20/20 or better without other correction and 95% obtained 20/40 or better at 9 months. -

Orthokeratology and Presbyopia
COVER STORY Orthokeratology and Presbyopia Motivated patients can achieve suitable far and near UCVA. BY ANTONIO CALOSSI, DIP OPTOM, FBCLA, FIACLE rthokeratology is a clinical technique that uses The ESA for hyperopia (Figure 1) is a customizable hexa- fitted rigid contact lenses to reshape the curve reverse geometry lens of my own design that my corneal profile, temporarily modifying or elimi- patients have used with successful outcomes. In selected nating refractive error. It is not a new and motivated patients, we were able to achieve suitable far O1 8,9 procedure, but it has undergone a resurgence of interest in and near UCVA. Our results demonstrate that the central the past decade.2,3 In orthokeratology, patients wear corneal region steepened after lens wear and the paracentral reverse-geometry contact lenses overnight for temporary regions flattened and then steepened again (Figure 2). I will correction of low to moderate ametropia.4,5 describe two successful cases. Orthokeratology contact lenses produce corneal reshap- ing because of the plasticity of the cornea, particularly that CASE REPORT NO. 1 of the epithelial layer. If the amount of corneal molding is A 43-year-old occasional soft contact lens wearer with properly controlled, the eye can be brought into correct hyperopia and normal ocular and general health reported focus to compensate for the patient’s refractive error. increased difficulty focusing on close work with her current Overnight wear of modern orthokeratology contact lenses monofocal spectacles and contact lenses. With the follow- produces rapid change, with most results noticeable after ing manifest refractions in her right and left eyes, respective- the first night. -

The Combined Effect of Low-Dose Atropine with Orthokeratology in Pediatric Myopia Control
Journal of Clinical Medicine Review The Combined Effect of Low-dose Atropine with Orthokeratology in Pediatric Myopia Control: Review of the Current Treatment Status for Myopia José-María Sánchez-González 1,2,* , Concepción De-Hita-Cantalejo 1, María-José Baustita-Llamas 1, María Carmen Sánchez-González 1 and Raúl Capote-Puente 1 1 Department of Physics of Condensed Matter, Optics Area, University of Seville, 41012 Seville, Spain; [email protected] (C.D.-H.-C.); [email protected] (M.-J.B.-L.); [email protected] (M.C.S.-G.); [email protected] (R.C.-P.) 2 Department of Ophthalmology & Optometry, Tecnolaser Clinic Vision, 41018 Seville, Spain * Correspondence: [email protected] Received: 25 May 2020; Accepted: 23 July 2020; Published: 24 July 2020 Abstract: Pediatric myopia has become a major international public health concern. The prevalence of myopia has undergone a significant increase worldwide. The purpose of this review of the current literature was to evaluate the peer-reviewed scientific literature on the efficacy and safety of low-dose atropine treatment combined with overnight orthokeratology for myopia control. A search was conducted in Pubmed and Web of Science with the following search strategy: (atropine OR low-dose atropine OR 0.01% atropine) AND (orthokeratology OR ortho-k) AND (myopia control OR myopia progression). All included studies improved myopia control by the synergistic effect of orthokeratology with low-dose atropine, compared with orthokeratology treatment alone. All studies included a short or medium follow-up period; therefore longer-term studies are necessary to validate these results. Keywords: atropine; orthokeratology; myopia control; refractive errors; peripheral refraction; myopia progression 1.