A Novel Method for the Quantitative Evaluation of Fibrinogen Coagulation YIDAN LIU [email protected]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proteinase K Dna Extraction Protocol
FT-85870n Proteinase K Product data Proteinase K, from Tritirachium album timber (Engyodontium album) Syn.: peptidase K, Tritirachium alkaline proteinase Protein K powder #858706 Proteinase K solution #718961 CAS: [ 39450-01-6 ] MW: 8,900 daltons (28.9 kDa). primary sequence for proteinase K: GAAQTNAPWGLARISSTSPGTSTYYYDESAGQGSCVYVIDTGIEASHPEF EGRAQMVKTYYYSSRDGNGHGTHCAGTVGSRTYGVAKKTQLFGVKVLDDN GSGQYSTIIAGMDFVASDKNNRNCPKGVVASLSLGGGYSSSVNSAAARLQ SSGVMVAVAAGNNNADARNYSPASEPSVCTVGASDRYDRRSSFSNYGSVL DIFGPGTSILSTWIGGSTRSISGTSMATPHVAGLAAYLMTLGKTTAASAC Proteinase K Protein Structure RYIADTANKGDLSNIPFGTVNLLAYNNYQA FAQ & Technical tips What is Proteinase K? PProteinase K (also protease K or endopeptidase K) is a broad-spectrum serine protease widely used in molecular biology. Proteinase K is able to digest native keratin (hair), hence, the name “Proteinase K”. It is commonly used because of its broad specificity, that makes it useful to clean nucleic acid complexe samples and to lyse cells. It has been used for isolation of mRNA, high molecular weight DNA and to inactivate other enzymatic activities. The enzyme was discovered in 1974 in extracts of the fungus Engyodontium album (formerly Tritirachium album). What are proteinase K applications? Proteinase K is ideal for many molecular biology applications because it is able to break down proteins and inactivate DNases and RNases that would otherwise degrade a desired sample of DNA or RNA. - Digestion of unwanted proteins in molecular biology applications - Removal of endotoxins bound to cationic proteins such as lysozyme and RNaseA - Removal of nucleases for in situ hybridization - Prion research with respect to TSE (transmissible spongiform encephalopathies) - Protease footprinting - Mitochontrial isolation - Isolation of genomic DNA - Isolation of cytoplasmic RNA - Isolation of highly native DNA or RNA Proteinase K is commonly used in molecular biology to digest protein and remove contamination from preparations of nucleic acid. -

Proteinase K # GE010.0100 – 100 Mg (FOR RESEARCH ONLY)
Product Info GE010 1 V6.0 – 6/2020 Proteinase K # GE010.0100 – 100 mg (FOR RESEARCH ONLY) Proteinase K is a broad-spectrum serine protease (28.9kDa monomer) that cleaves peptide bonds at the carboxylic sides of aliphatic, aromatic, and hydrophobic amino acids. Quantity 100 mg lyophilized powder purified from Pichia pastoris harbouring the gene encoding endolytic protease from Tritirachium album. Supplied with 1 ml of a 10x concentrated Storage Buffer. Applications Isolation of genomic DNA from cultured cells and tissues; removal of DNases and RNases during DNA and/or RNA purification; determination of enzyme locations. Specifications Free of DNases and RNases. Specific Activity: >30 units per mg. Quality Control Enzyme activity is assayed by digesting hemoglobin at a concentration of 16.7 mg/ml in a solution of 80mM potassium phosphate (pH 7.5), 5M urea, 4mM NaCl, 3mM CaCl2. Absence of endodeoxyribonucleases, exodeoxyribonucleases, and ribonucleases was confirmed by appropriate assays. Storage Store lyophilized powder at +4ºC for several months or -20ºC for at least 2 years. The concentrated (10x) storage buffer (500mM Tris-HCl, 50mM CaCl2) can be stored at room temperature or +4ºC. GRiSP Research Solutions 2020 Product Info GE010 2 V6.0 – 6/2020 Prior to use Reconstitute Proteinase K at a desired concentration (e.g. 10 mg/ml) using either ultrapure water or 1x Storage Buffer (50mM Tris-HCl pH8.0) [dilute storage buffer with ultrapure DNase/RNase-free water with or without glycerol (see below)]. Reconstituted Proteinase K should be stored at +4ºC for up to a few months. If longer storage is required, reconstitute Proteinase K in 1x Storage Buffer containing 50% glycerol and store at -20ºC Enzyme activity Proteinase K is activated by calcium (1-5mM). -

AEBSF Catalog Number: EI001 Lot Number: 1384335
AEBSF Catalog Number: EI001 Lot Number: 1384335 Specifications and Use Product ♦ 4-(2-Aminoethyl-benzensulfonyl fluoride hydrochloride) (AEBSF) Molecular Mass ♦ 239.7 Da Purity ♦ > 96% by high performance liquid chromatography Quantity ♦ 250 mg Effective ♦ 0.1 - 1.0 mM Concentration Activity and ♦ Measured by its ability to inhibit trypsin cleavage of a peptide substrate (R&D Systems, Applications Catalog # ES002). ♦ The IC50 is < 15 µM, as measured under the described conditions. See Activity Assay Protocol on next page for details. ♦ AEBSF is an irreversible inhibitor of serine proteases. As compared to PMSF (Phenylmethanesulphonyl fluoride), which is another commonly used serine protease inhibitor, AEBSF is water soluble, less toxic and more stable.1 ♦ AEBSF also inhibits NADH oxidase activation through a non-proteolytic route.2 Formulation ♦ Powder was obtained from a solvent containing absolute ethanol and ether. Reconstitution ♦ It is recommended that small amounts of powder be weighed and dissolved in water to give a stock solution at 100 mM. Aliquot and store at -20° C in a manual defrost freezer. Storage ♦ Powder is stable for up to twelve months from date of receipt at -20° C to -70° C. ♦ Upon reconstitution, the samples can be stored at 2° - 8° C for 1 - 2 months or at -20° C to -70° C in a manual defrost freezer for three months. ♦ Avoid repeated freeze-thaw cycles. References: 1. Beynon, R. and J.S. Bond, 2001, Proteolytic Enzymes: A Practical Approach, Oxford University Press. 2. Diatchuk, V. et al. 1997, J. Biol. Chem. 272:13292 - 13301. FOR RESEARCH USE ONLY. NOT FOR USE IN HUMANS. -

Proteinase K
Proteinase K Catalog number: AR0056 Boster’s Proteinase K is a Tris-HCl buffered concentrated enzyme stock solution that is to be used as assistant pre-treatment reagent in Western blot and IHC assay procedures. This package insert must be read in its entirety before using this product. For research use only. Not for use in diagnostic procedures. BOSTER BIOLOGICAL TECHNOLOGY 3942 B Valley Ave, Pleasanton, CA 94566 Phone: 888-466-3604 Fax: 925-215-2184 Email:[email protected] Web: www.bosterbio.com Proteinase K Catalog Number: AR0056 Overview Physical State Liquid Pack Size 5mL Form Supplied 1:100 Concentrated stock solution of Proteinase K in Tris-HCl buffer Content 10 mg/ml Proteinase K, 50mM Tris-HCl (pH 7.5), 150mM NaCl Reagent Type Assistant Reagent Enzyme Concentration 10 mg/ml Recommended working 50-100µg/ml for protein removal and enzyme inactivation; up to 2mg/ml for tissue treatment concentration pH 7.5-9.0 Storage Store at -20˚C for one year Equivalent Abcam (Product No. ab64220) Cite This Product Proteinase K (Boster Biological Technology, Pleasanton CA, USA, Catalog # AR0056) Precautions FOR RESEARCH USE ONLY. NOT FOR DIAGNOSTIC AND CLINICAL USE Assay Principle Proteinase K is a Tris-HCl buffered concentrated enzyme stock solution that is to be used as assistant pre-treatment reagent in Western blot and IHC assay procedures for general protein digestion in tissue lysates during sample preparation, for eliminating comigrating protein antigens prior to SDS-PAGE, as well as for proteolytic antigen retrieval prior to antibody -
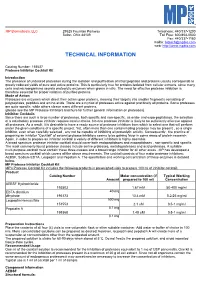
Technical Information
MP Biomedicals, LLC 29525 Fountain Parkway Telephone: 440/337-1200 Solon, Ohio 44139 Toll Free: 800/854-0530 Fax: 440/337-1180 mailto: [email protected] web: http://www.mpbio.com TECHNICAL INFORMATION Catalog Number: 158837 Protease Inhibitor Cocktail Kit Introduction The presence of undesired proteases during the isolation and purification of intact peptides and proteins usually corresponds to greatly reduced yields of pure and active proteins. This is particularly true for proteins isolated from cellular extracts, since many cells and microorganisms secrete proteolytic enzymes when grown in vitro. The need for effective protease inhibition is therefore essential for proper isolation of purified proteins. Mode of Action Proteases are enzymes which direct their action upon proteins, cleaving their targets into smaller fragments consisting of polypeptides, peptides and amino acids. There are a myriad of proteases active against practically all proteins. Some proteases are quite specific, while others cleave many different proteins. (please see the MP Protease Inhibitors brochure for further general information on proteases). Inhibitor Cocktails Since there are such a large number of proteases, both specific and non-specific, as endo- and expo-peptidases, the selection of a satisfactory protease inhibitor requires careful choice. No one protease inhibitor is likely to be sufficiently effective against all proteases. As a result, it is desirable to have a ready source of protease inhibitors from which to select one that will perform under the given conditions of a specific project. Yet, often more than one contaminating protease may be present , so a single inhibitor, even when carefully selected , any not be capable of inhibiting all proteolytic activity. -

The Protease Inhibitor 4-(2-Aminoethyl) Benzenesulfonyl Fluoride Covalently Modifies Human Plasma Proteins and Changes Protein Isoform Profiles
The Protease Inhibitor 4-(2-Aminoethyl) Benzenesulfonyl HUPO 3rd Annual World Congress, Beijing 2004 Poster No. MC-010 Fluoride Covalently Modifies Human Plasma Proteins and Changes Protein Isoform Profiles 1. Sigma-Aldrich Biotechnology, 2909 Laclede Ave., St. Louis, MO 63103. 1 1 1 1 2. The Johns Hopkins University School of Medicine, Mark D. Schuchard , Richard J. Mehigh , Steven L. Cockrill , Justin Wildsmith , Department of Pathology, Division of Clinical Chemistry, William K. Kappel1, Alex J. Rai2 and Graham B. I. Scott1. 600 N. Wolfe St., Meyer B-121, Baltimore, MD 21287 Abstract Figure 4a The presence of protease inhibitors in serum or plasma samples has been found to significantly Panel A impact the isoform profile of selected plasma proteins as seen on two-dimensional electrophoresis (2-DE) gels. With the inclusion of a protease inhibitor cocktail, many human plasma protein trains (depleted of albumin and IgG) exhibited higher isoelectric point (pI) isoforms. This shift was especially apparent for Apolipoprotein A1 (Apo A1), a relatively high abundance protein. The six protease inhibitor components of the cocktail were individually investigated with albumin Apo A1 train and IgG depleted human plasma and it was shown that the observed effects were caused by 4-(2-Aminoethyl) Benzenesulfonyl Fluoride (AEBSF), a serine protease inhibitor which covalently modifies serine resides. Several serine-containing peptides of Apo A1 were modified with a concomitant mass increase of 183 Da, consistent with the mass increase expected following reaction with AEBSF. These modifications were predominantly seen in the high pI spots. An increase in the number and proportion of modified peptides with increasing pI was also observed. -

Proteinase K # GE010.0100 – 100 Mg
Product Info Version 1.4 Proteinase K # GE010.0100 – 100 mg Proteinase K is a broad-spectrum serine protease (28.9kDa monomer) that cleaves peptide bonds at the carboxylic sides of aliphatic, aromatic, and hydrophobic amino acids. Quantity 100 mg lyophilized powder purified from purified from Pichia pastoris harbouring the gene encoding endolytic protease from Tritirachium album. Applications Isolation of genomic DNA from cultured cells and tissues, removal of DNAses and RNAses during DNA and/or RNA purification, determination of enzyme locations Specifications Free of DNAses and RNAses. Specific Activity ~30 Kunitz units per mg. Quality Control Enzyme activity is assayed by digesting hemoglobin at a concentration of 16,7 mg/ml in a solution of 0.08M potassium phosphate (pH 7,5), 5M urea, 4mM NaCl, 3mM CaCl2. Absence of endodeoxyribonucleases, exodeoxyribonucleases, and ribonucleases was confirmed by appropriate assays. GRiSP Research Solutions 2015 Storage For short term, store lyophilized powder at +4ºC. Before use, reconstitute Proteinase K at a desired concentration using either ultrapure water or 50mM Tris-HCl pH 7,5 containing 5mM CaCl2 and 50% glycerol. Reconstituted Proteinase K should be stored at -20ºC. Enzyme activity Proteinase K is activated by calcium (1-5mM). Although Ca2+ does not directly influences catalytic activity it does contributes to the protein stability (protection against autolysis, increasing thermal stability). Removal of Ca2+ (e.g. by adding EDTA) reduces proteolytic activity by 80%, however, the residual activity is sufficient to digest proteins, which usually contaminate nucleic acid preparations. Therefore, the digest with Proteinase K for the purification of nucleic acids is performed in the presence of EDTA (inhibition of magnesium-dependent enzymes such as DNAses). -
Www .Alfa.Com
Bio 2013-14 Alfa Aesar North America Alfa Aesar Korea Uni-Onward (International Sales Headquarters) 101-3701, Lotte Castle President 3F-2 93 Wenhau 1st Rd, Sec 1, 26 Parkridge Road O-Dong Linkou Shiang 244, Taipei County Ward Hill, MA 01835 USA 467, Gongduk-Dong, Mapo-Gu Taiwan Tel: 1-800-343-0660 or 1-978-521-6300 Seoul, 121-805, Korea Tel: 886-2-2600-0611 Fax: 1-978-521-6350 Tel: +82-2-3140-6000 Fax: 886-2-2600-0654 Email: [email protected] Fax: +82-2-3140-6002 Email: [email protected] Email: [email protected] Alfa Aesar United Kingdom Echo Chemical Co. Ltd Shore Road Alfa Aesar India 16, Gongyeh Rd, Lu-Chu Li Port of Heysham Industrial Park (Johnson Matthey Chemicals India Toufen, 351, Miaoli Heysham LA3 2XY Pvt. Ltd.) Taiwan England Kandlakoya Village Tel: 866-37-629988 Bio Chemicals for Life Tel: 0800-801812 or +44 (0)1524 850506 Medchal Mandal Email: [email protected] www.alfa.com Fax: +44 (0)1524 850608 R R District Email: [email protected] Hyderabad - 501401 Andhra Pradesh, India Including: Alfa Aesar Germany Tel: +91 40 6730 1234 Postbox 11 07 65 Fax: +91 40 6730 1230 Amino Acids and Derivatives 76057 Karlsruhe Email: [email protected] Buffers Germany Tel: 800 4566 4566 or Distributed By: Click Chemistry Reagents +49 (0)721 84007 280 Electrophoresis Reagents Fax: +49 (0)721 84007 300 Hydrus Chemical Inc. Email: [email protected] Uchikanda 3-Chome, Chiyoda-Ku Signal Transduction Reagents Tokyo 101-0047 Western Blot and ELISA Reagents Alfa Aesar France Japan 2 allée d’Oslo Tel: 03(3258)5031 ...and much more 67300 Schiltigheim Fax: 03(3258)6535 France Email: [email protected] Tel: 0800 03 51 47 or +33 (0)3 8862 2690 Fax: 0800 10 20 67 or OOO “REAKOR” +33 (0)3 8862 6864 Nagorny Proezd, 7 Email: [email protected] 117 105 Moscow Russia Alfa Aesar China Tel: +7 495 640 3427 Room 1509 Fax: +7 495 640 3427 ext 6 CBD International Building Email: [email protected] No. -

Protease Inhibitors: Summary and Applications
Protease Inhibitors: Summary and Applications Depending on the binding of the inhibitor, you may find both reversible and irreversible inhibition. In reversible enzyme inhibition the inhibitor doesn't bind closely to the enzyme and can be separated or displaced in succession. It lowers its activity and/or the speed constant of the reaction of the substrate to the product. It also establishes a balance between the enzyme-inhibitor complexes with or without substrate. Metabolic processes are typical examples of this, which, depending on the physiological state of the cells, either are enhanced or inhibited. Competitive inhibitors are reagents which compete with substrate (A) for the binding site in the enzyme's active centre and increase the Michaelis Menten constant of the enzyme. They are either extremely similar to the substrate (but are not converted and can be displaced again by the substrate) or even represent a second substrate and thereby competitively inhibit the conversion of substrate A. In non-competitive inhibition the inhibitor does not bind in the active centre but through binding, it changes the enzyme's tertiary structure to such an extent that a product can no longer be produced/set free. Uncompetitive inhibition is a special case where the inhibitor can only interact with the enzyme-substrate complex and it changes both the MM-constant as well as the maximum reaction speed. In partial-competitive inhibition, binding of the inhibitor lowers the affinity of the enzyme to the substrate without influencing the speed constants. In irreversible inhibition, the inhibitor binds so closely that it can no longer be separated from the enzyme and thus the activity of the enzyme is permanently reduced or destroyed. -

Pefabloc® SC AEBSF, 4-(2-Aminoethyl)-Benzenesulfonyl Fluoride Hydrochloride Y Version: 17 Content Version: December 2020
For life science research only. Not for use in diagnostic procedures. R Pefabloc® SC AEBSF, 4-(2-Aminoethyl)-benzenesulfonyl fluoride hydrochloride y Version: 17 Content Version: December 2020 Cat. No. 11 429 868 001 100 mg Cat. No. 11 585 916 001 500 mg Cat. No. 11 429 876 001 1 g Store the product at +2 to +8°C. sigma-aldrich.com 1. General Information ............................................................................................................................3 1.1. Contents ................................................................................................................................................................................................... 3 1.2. Storage and Stability ........................................................................................................................................................................... 3 Storage Conditions (Product) .......................................................................................................................................................... 3 Storage Conditions (Working Solution) ........................................................................................................................................ 3 Reconstitution ........................................................................................................................................................................................ 3 1.3. Application ............................................................................................................................................................................................. -

Protease Inhibitors
Protease Inhibitors Proteases are ubiquitous enzymes which direct their action upon proteins, cleaving those proteins into smaller fragments consisting of polypeptides, peptides and amino acids. There are many proteases active against many proteins, and some are very specific while others cleave many different proteins. In general proteases are classified into two main subclasses: endopeptidases and exopeptidases, dependent upon how and where the protease cleaves the protein. Endopeptidases attack proteins internally, typically at a specific amino acid site, and they cleave the protein into smaller fragments as they digest it. Exopeptidases, as their name suggests, begin digesting their target protein at the ends of the protein chain. There are two main classes of exopeptidases, depending upon which functional group of the amino acid they attack, the N-terminus or the carboxy terminus. In both cases, the proteases begin digesting the protein and proceed along the amino acid backbone until they encounter a specific amino acid that signals the protease to stop. The presence of undesired proteases during isolation and purification of intact proteins and peptides usually corresponds to greatly reduced yields and denatured proteins. The need for effective protease inhibition is therefore essential in sensitive protein research. Alfa Aesar is pleased to present a versatile range of protease inhibitors and protease inhibitor cocktails for sensitive applications in protein research. www.alfa.com Protease Inhibitors Item Description Application Sizes Irreversible, covalent binding serine protease inhibitor. Belongs to the family of sulfonyl fluorides that block trypsin AEBSF, [4-(2-Aminoethyl)- H26473 and chymotrypsin-like enzymes. Similar to PMSF, AEBSF offers 250mg,1gm benzesulfonyl fluoride HCl much lower toxicity than PMSF, more solubility in water, higher inhibitory activity and better stability. -

Proteinase K - Solution 20 Mg / Ml
Proteinase K - Solution 20 mg / mL From Tritirachium album Product No. A4392 Description Molecular weight: 27000 g/mol CAS-No.: [39450-01-6] HS-No.: 35079090 EINECS: 2544578 E.C.: 3.4.21.14 Composition Proteinase K: 20 mg/ml CaCl2 2H2O 1 mM Glycerol (v/v) 40 % Tris HCl (pH7.5) 10 mM Specification Activity: min. 600 mAnsonU/ml DNases/RNases: not detectable Unit definition: One milliAnson Unit (mAU) is the activity that releases folin-positive amino acids and peptides corresponding to 1 µmol tyrosine per minute.* pH optimum: 7.5 - 12.0 pI: 8.9 Inactivation (temperature): > 65°C Working concentration: varies from approx. 10 - 100 µg/ml Stability (in solution): 12 months Storage: 2-8°C; it is recommended to prepare aliquots for single use * Alternative Unit definition: 1 DMC-unit catalyzes the hydrolysis of 1 µmol dimethyl casein per minute at 25 °C, pH 7.0. The liberated amino groups are determined with 2,4,6-trinitrobenzene sulfonic acid. Comment Proteinase K belongs to the family of the subtilisin type serine proteases. It shows endo- and exoproteolytic activity. Activated by calcium (1-5 mM), the enzyme cleaves proteins preferably behind hydrophobic amino acids (aliphatic, aromatic and other hydrophobic amino acids). Proteins will be completely digested, if the incubation time is long enough and the protease concentration is high. Temperatures above 65°C or the serine proteinase inhibitors AEBSF, PMSF or DFP inhibit the activity. Proteinase K is not inactivated by EDTA (see Ref. 5), iodoacetic acid or, interestingly, by other serine protease inhibitors like TLCK and TPCK.