A Genome-Wide Functional Enrichment Pathway Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sex Differences in Glutamate Receptor Gene Expression in Major Depression and Suicide
Molecular Psychiatry (2015) 20, 1057–1068 © 2015 Macmillan Publishers Limited All rights reserved 1359-4184/15 www.nature.com/mp IMMEDIATE COMMUNICATION Sex differences in glutamate receptor gene expression in major depression and suicide AL Gray1, TM Hyde2,3, A Deep-Soboslay2, JE Kleinman2 and MS Sodhi1,4 Accumulating data indicate that the glutamate system is disrupted in major depressive disorder (MDD), and recent clinical research suggests that ketamine, an antagonist of the N-methyl-D-aspartate (NMDA) glutamate receptor (GluR), has rapid antidepressant efficacy. Here we report findings from gene expression studies of a large cohort of postmortem subjects, including subjects with MDD and controls. Our data reveal higher expression levels of the majority of glutamatergic genes tested in the dorsolateral prefrontal cortex (DLPFC) in MDD (F21,59 = 2.32, P = 0.006). Posthoc data indicate that these gene expression differences occurred mostly in the female subjects. Higher expression levels of GRIN1, GRIN2A-D, GRIA2-4, GRIK1-2, GRM1, GRM4, GRM5 and GRM7 were detected in the female patients with MDD. In contrast, GRM5 expression was lower in male MDD patients relative to male controls. When MDD suicides were compared with MDD non-suicides, GRIN2B, GRIK3 and GRM2 were expressed at higher levels in the suicides. Higher expression levels were detected for several additional genes, but these were not statistically significant after correction for multiple comparisons. In summary, our analyses indicate a generalized disruption of the regulation of the GluRs in the DLPFC of females with MDD, with more specific GluR alterations in the suicides and in the male groups. -

Supplementary Material
Supplementary Material Table S1: Significant downregulated KEGGs pathways identified by DAVID following exposure to five cinnamon- based phenylpropanoids (p < 0.05). p-value Term: Genes (Benjamini) Cytokine-cytokine receptor interaction: FASLG, TNFSF14, CXCL11, IL11, FLT3LG, CCL3L1, CCL3L3, CXCR6, XCR1, 2.43 × 105 RTEL1, CSF2RA, TNFRSF17, TNFRSF14, CCNL2, VEGFB, AMH, TNFRSF10B, INHBE, IFNB1, CCR3, VEGFA, CCR2, IL12A, CCL1, CCL3, CXCL5, TNFRSF25, CCR1, CSF1, CX3CL1, CCL7, CCL24, TNFRSF1B, IL12RB1, CCL21, FIGF, EPO, IL4, IL18R1, FLT1, TGFBR1, EDA2R, HGF, TNFSF8, KDR, LEP, GH2, CCL13, EPOR, XCL1, IFNA16, XCL2 Neuroactive ligand-receptor interaction: OPRM1, THRA, GRIK1, DRD2, GRIK2, TACR2, TACR1, GABRB1, LPAR4, 9.68 × 105 GRIK5, FPR1, PRSS1, GNRHR, FPR2, EDNRA, AGTR2, LTB4R, PRSS2, CNR1, S1PR4, CALCRL, TAAR5, GABRE, PTGER1, GABRG3, C5AR1, PTGER3, PTGER4, GABRA6, GABRA5, GRM1, PLG, LEP, CRHR1, GH2, GRM3, SSTR2, Chlorogenic acid Chlorogenic CHRM3, GRIA1, MC2R, P2RX2, TBXA2R, GHSR, HTR2C, TSHR, LHB, GLP1R, OPRD1 Hematopoietic cell lineage: IL4, CR1, CD8B, CSF1, FCER2, GYPA, ITGA2, IL11, GP9, FLT3LG, CD38, CD19, DNTT, 9.29 × 104 GP1BB, CD22, EPOR, CSF2RA, CD14, THPO, EPO, HLA-DRA, ITGA2B Cytokine-cytokine receptor interaction: IL6ST, IL21R, IL19, TNFSF15, CXCR3, IL15, CXCL11, TGFB1, IL11, FLT3LG, CXCL10, CCR10, XCR1, RTEL1, CSF2RA, IL21, CCNL2, VEGFB, CCR8, AMH, TNFRSF10C, IFNB1, PDGFRA, EDA, CXCL5, TNFRSF25, CSF1, IFNW1, CNTFR, CX3CL1, CCL5, TNFRSF4, CCL4, CCL27, CCL24, CCL25, CCL23, IFNA6, IFNA5, FIGF, EPO, AMHR2, IL2RA, FLT4, TGFBR2, EDA2R, -

Ion Channels
UC Davis UC Davis Previously Published Works Title THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels. Permalink https://escholarship.org/uc/item/1442g5hg Journal British journal of pharmacology, 176 Suppl 1(S1) ISSN 0007-1188 Authors Alexander, Stephen PH Mathie, Alistair Peters, John A et al. Publication Date 2019-12-01 DOI 10.1111/bph.14749 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Ion channels. British Journal of Pharmacology (2019) 176, S142–S228 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels Stephen PH Alexander1 , Alistair Mathie2 ,JohnAPeters3 , Emma L Veale2 , Jörg Striessnig4 , Eamonn Kelly5, Jane F Armstrong6 , Elena Faccenda6 ,SimonDHarding6 ,AdamJPawson6 , Joanna L Sharman6 , Christopher Southan6 , Jamie A Davies6 and CGTP Collaborators 1School of Life Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK 2Medway School of Pharmacy, The Universities of Greenwich and Kent at Medway, Anson Building, Central Avenue, Chatham Maritime, Chatham, Kent, ME4 4TB, UK 3Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK 4Pharmacology and Toxicology, Institute of Pharmacy, University of Innsbruck, A-6020 Innsbruck, Austria 5School of Physiology, Pharmacology and Neuroscience, University of Bristol, Bristol, BS8 1TD, UK 6Centre for Discovery Brain Science, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2019/20 is the fourth in this series of biennial publications. The Concise Guide provides concise overviews of the key properties of nearly 1800 human drug targets with an emphasis on selective pharmacology (where available), plus links to the open access knowledgebase source of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. -

WO 2019/068007 Al Figure 2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2019/068007 Al 04 April 2019 (04.04.2019) W 1P O PCT (51) International Patent Classification: (72) Inventors; and C12N 15/10 (2006.01) C07K 16/28 (2006.01) (71) Applicants: GROSS, Gideon [EVIL]; IE-1-5 Address C12N 5/10 (2006.0 1) C12Q 1/6809 (20 18.0 1) M.P. Korazim, 1292200 Moshav Almagor (IL). GIBSON, C07K 14/705 (2006.01) A61P 35/00 (2006.01) Will [US/US]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., C07K 14/725 (2006.01) P.O. Box 4044, 7403635 Ness Ziona (TL). DAHARY, Dvir [EilL]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., P.O. (21) International Application Number: Box 4044, 7403635 Ness Ziona (IL). BEIMAN, Merav PCT/US2018/053583 [EilL]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., P.O. (22) International Filing Date: Box 4044, 7403635 Ness Ziona (E.). 28 September 2018 (28.09.2018) (74) Agent: MACDOUGALL, Christina, A. et al; Morgan, (25) Filing Language: English Lewis & Bockius LLP, One Market, Spear Tower, SanFran- cisco, CA 94105 (US). (26) Publication Language: English (81) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of national protection available): AE, AG, AL, AM, 62/564,454 28 September 2017 (28.09.2017) US AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, 62/649,429 28 March 2018 (28.03.2018) US CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (71) Applicant: IMMP ACT-BIO LTD. -
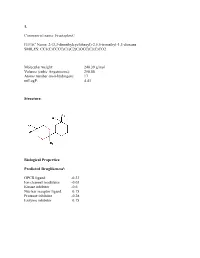
Sean Raspet – Molecules
1. Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Molecular weight: 240.39 g/mol Volume (cubic Angstroems): 258.88 Atoms number (non-hydrogen): 17 miLogP: 4.43 Structure: Biological Properties: Predicted Druglikenessi: GPCR ligand -0.23 Ion channel modulator -0.03 Kinase inhibitor -0.6 Nuclear receptor ligand 0.15 Protease inhibitor -0.28 Enzyme inhibitor 0.15 Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Predicted Olfactory Receptor Activityii: OR2L13 83.715% OR1G1 82.761% OR10J5 80.569% OR2W1 78.180% OR7A2 77.696% 2. Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Molecular weight: 239.36 Volume (cubic Angstroems): 252.83 Atoms number (non-hydrogen): 17 miLogP: 4.33 Structure: Biological Properties: Predicted Druglikeness: GPCR ligand -0.6 Ion channel modulator -0.41 Kinase inhibitor -0.93 Nuclear receptor ligand -0.17 Protease inhibitor -0.39 Enzyme inhibitor 0.01 Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Predicted Olfactory Receptor Activity: OR52D1 71.900% OR1G1 70.394% 0R52I2 70.392% OR52I1 70.390% OR2Y1 70.378% 3. Commercial name: Hyperflor© IUPAC Name: 2-benzyl-1,3-dioxan-5-one SMILES: O=C1COC(CC2=CC=CC=C2)OC1 Molecular weight: 192.21 g/mol Volume -
Neuroplasticity Pathways and Protein-Interaction Networks Are
Waller et al. BMC Neurosci (2017) 18:56 DOI 10.1186/s12868-017-0376-x BMC Neuroscience RESEARCH ARTICLE Open Access Neuroplasticity pathways and protein‑interaction networks are modulated by vortioxetine in rodents Jessica A. Waller1, Sara Holm Nygaard2, Yan Li1, Kristian Gaarn du Jardin3, Joseph A. Tamm4, Aicha Abdourahman4, Betina Elfving3, Alan L. Pehrson1, Connie Sánchez1* and Rasmus Wernersson2,5* Abstract Background: The identifcation of biomarkers that predict susceptibility to major depressive disorder and treatment response to antidepressants is a major challenge. Vortioxetine is a novel multimodal antidepressant that possesses pro-cognitive properties and diferentiates from other conventional antidepressants on various cognitive and plastic- ity measures. The aim of the present study was to identify biological systems rather than single biomarkers that may underlie vortioxetine’s treatment efects. Results: We show that the biological systems regulated by vortioxetine are overlapping between mouse and rat in response to distinct treatment regimens and in diferent brain regions. Furthermore, analysis of complexes of physically-interacting proteins reveal that biomarkers involved in transcriptional regulation, neurodevelopment, neu- roplasticity, and endocytosis are modulated by vortioxetine. A subsequent qPCR study examining the expression of targets in the protein–protein interactome space in response to chronic vortioxetine treatment over a range of doses provides further biological validation that vortioxetine engages neuroplasticity networks. Thus, the same biology is regulated in diferent species and sexes, diferent brain regions, and in response to distinct routes of administration and regimens. Conclusions: A recurring theme, based on the present study as well as previous fndings, is that networks related to synaptic plasticity, synaptic transmission, signal transduction, and neurodevelopment are modulated in response to vortioxetine treatment. -

Personal Receptor Repertoires: Olfaction As a Model
Olender et al. BMC Genomics 2012, 13:414 http://www.biomedcentral.com/1471-2164/13/414 RESEARCH ARTICLE Open Access Personal receptor repertoires: olfaction as a model Tsviya Olender1*, Sebastian M Waszak2, Maya Viavant1, Miriam Khen1, Edna Ben-Asher1, Alejandro Reyes3, Noam Nativ1, Charles J Wysocki4, Dongliang Ge5 and Doron Lancet1* Abstract Background: Information on nucleotide diversity along completely sequenced human genomes has increased tremendously over the last few years. This makes it possible to reassess the diversity status of distinct receptor proteins in different human individuals. To this end, we focused on the complete inventory of human olfactory receptor coding regions as a model for personal receptor repertoires. Results: By performing data-mining from public and private sources we scored genetic variations in 413 intact OR loci, for which one or more individuals had an intact open reading frame. Using 1000 Genomes Project haplotypes, we identified a total of 4069 full-length polypeptide variants encoded by these OR loci, average of ~10 per locus, constituting a lower limit for the effective human OR repertoire. Each individual is found to harbor as many as 600 OR allelic variants, ~50% higher than the locus count. Because OR neuronal expression is allelically excluded, this has direct effect on smell perception diversity of the species. We further identified 244 OR segregating pseudogenes (SPGs), loci showing both intact and pseudogene forms in the population, twenty-six of which are annotatively “resurrected” from a pseudogene status in the reference genome. Using a custom SNP microarray we validated 150 SPGs in a cohort of 468 individuals, with every individual genome averaging 36 disrupted sequence variations, 15 in homozygote form. -

The Genes Encoding the Glutamate Receptor Subunits Kal And
Proc. Nati. Acad. Sci. USA Vol. 91, pp. 11849-11853, December 1994 Neurobiology The genes encoding the glutamate receptor subunits KAl and KA2 (GRIK4 and GRIK5) are located on separate chromosomes in human, mouse, and rat (lgand-gated ion channels/human chromosomes 19q13.2 and 11q22-23/mouse chromosomes 7 and 9/rat chromosomes 8 and 1) CLAUDE SZPIRER*, MONTSE MOLNOt, RACHELE ANTONACCI*, NANCY A. JENKINS§, PALMA FINELLI*, JOSIANE SZPIRER*, MICHELE RivIERE*, MARIANO ROCCHIt, DEBRA J. GILBERT§, NEAL G. COPELAND§, AND VITTORIO GALLOt¶ *Departement de Biologie Moleculaire, Universitd Libre de Bruxelles, B-1640 Rhode-St.-Genese, Belgium; tLaboratory of Cellular and Molecular Neurophysiology, National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD 20892; tlstituto di Genetica, University of Bari, 70126 Bari, Italy; Mammalian Genetics Laboratory, Advanced BioScience Laboratories-Basic Research Program, National Cancer Institute, Frederick Cancer Research and Development Center, Frederick, MD 21702 Communicated by E. Costa, August 10, 1994 ABSTRACT The chromosomal alization of the human (AMPA)-preferring family (GluR1-4, or GluRA-D; GRIA and rat genes encoding the kalnate-preferring glutamate recep- gene family) and the two kainate-preferring families tor subunits KAl and KA2 (GRIK4 and GRIKS, respectively) (GluR5-7 and KA1 and KA2; in the two GRIK gene was determined by Southern analysis ofrat x mouse and human families). The kainate-preferring subunits KA1 and KA2 x mouse somatic cell hybrid panels and by fluorescence in situ display 68% identity in their amino acid sequence and code hybridization. The localization of the mouse genes (Grik4 and for proteins that do not form functional homomeric ionic Gri5) was established by interspecific backcross mapping. -

Kava for the Treatment of Generalised Anxiety Disorder (K-GAD): Study Protocol for a Randomised Controlled Trial Karen M
Savage et al. Trials (2015) 16:493 DOI 10.1186/s13063-015-0986-5 TRIALS STUDY PROTOCOL Open Access Kava for the treatment of generalised anxiety disorder (K-GAD): study protocol for a randomised controlled trial Karen M. Savage1,2*, Con K. Stough2, Gerard J. Byrne3, Andrew Scholey2, Chad Bousman2,4,5,6, Jenifer Murphy1, Patricia Macdonald3, Chao Suo7, Matthew Hughes8, Stuart Thomas9, Rolf Teschke10, Chengguo Xing11 and Jerome Sarris1,2 Abstract Background: Generalised anxiety disorder (GAD) is a chronic and pervasive condition that generates high levels of psychological stress, and it is difficult to treat in the long term. Current pharmacotherapeutic options for GAD are in some cases only modestly effective, and may elicit undesirable side effects. Through targeted actions on the gamma-aminobutyric acid (GABA) pathway, the South Pacific medicinal plant kava (Piper methysticum)isa non-addictive, non-hypnotic anxiolytic with the potential to treat GAD. The evidence for the efficacy of kava for treating anxiety has been affirmed through clinical trials and meta-analyses. Recent research has also served to lessen safety concerns regarding the use of kava due to hepatotoxic risk, which is reflected in a recent German court overturning the previous kava ban in that country (which may in turn influence a reinstatement by the European Union). The aim of current research is to assess the efficacy of an ‘aqueous noble cultivar rootstock extract’ of kava in GAD in a larger longer term study. In addition, we plan to investigate the pharmacogenomic influence of GABA transporters on response, effects of kava on gene expression, and for the first time, the neurobiological correlates of treatment response via functional and metabolic imaging. -

The Hypothalamus As a Hub for SARS-Cov-2 Brain Infection and Pathogenesis
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.08.139329; this version posted June 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. The hypothalamus as a hub for SARS-CoV-2 brain infection and pathogenesis Sreekala Nampoothiri1,2#, Florent Sauve1,2#, Gaëtan Ternier1,2ƒ, Daniela Fernandois1,2 ƒ, Caio Coelho1,2, Monica ImBernon1,2, Eleonora Deligia1,2, Romain PerBet1, Vincent Florent1,2,3, Marc Baroncini1,2, Florence Pasquier1,4, François Trottein5, Claude-Alain Maurage1,2, Virginie Mattot1,2‡, Paolo GiacoBini1,2‡, S. Rasika1,2‡*, Vincent Prevot1,2‡* 1 Univ. Lille, Inserm, CHU Lille, Lille Neuroscience & Cognition, DistAlz, UMR-S 1172, Lille, France 2 LaBoratorY of Development and PlasticitY of the Neuroendocrine Brain, FHU 1000 daYs for health, EGID, School of Medicine, Lille, France 3 Nutrition, Arras General Hospital, Arras, France 4 Centre mémoire ressources et recherche, CHU Lille, LiCEND, Lille, France 5 Univ. Lille, CNRS, INSERM, CHU Lille, Institut Pasteur de Lille, U1019 - UMR 8204 - CIIL - Center for Infection and ImmunitY of Lille (CIIL), Lille, France. # and ƒ These authors contriButed equallY to this work. ‡ These authors directed this work *Correspondence to: [email protected] and [email protected] Short title: Covid-19: the hypothalamic hypothesis 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.06.08.139329; this version posted June 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

(51) International Patent Classification: EE, ES, FI, FR, GB, GR, HR, HU, IE
( (51) International Patent Classification: EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, Not classified MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, TR), OAPI (BF, BJ, CF, CG, Cl, CM, GA, GN, GQ, GW, (21) International Application Number: KM, ML, MR, NE, SN, TD, TG). PCT/IB20 19/00 1108 (22) International Filing Date: Declarations under Rule 4.17: 27 September 2019 (27.09.2019) — as to the applicant's entitlement to claim the priority of the earlier application (Rule 4.17(iii)) (25) Filing Language: English Published: (26) Publication Language: English — without international search report and to be republished (30) Priority Data: upon receipt of that report (Rule 48. 2(g)) 62/738,895 28 September 2018 (28.09.2018) US 62/847,830 14 May 2019 (14.05.2019) US (71) Applicant: IMMPACT-BIO LTD. [EVIL]; 2 Ilan Ramon St., P.O. Box 4044, 7403635 Ness Ziona (EL). (72) Inventors; and (71) Applicants: SAGI, Yael [IL/IL]; c/o ImmPACT-Bio Ltd., 2 Ilan Ramon St., P.O. Box 4044, 7403635 Ness Ziona (IL). SHARBI-YUNGER, Adi [IL/IL]; c/o ImmPACT-Bio Ltd., 2 Ilan Ramon St., P.O. Box 4044, 7403635 Ness Ziona (IL). (72) Inventors: GROSS, Gideon; III-1-5 Address M.P. Koraz- im, 1292200 Moshav Ahnagor (IL). GIBSON, William, J.; c/o ImmPACT-Bio Ltd., 2 Ilan Ramon St., P.O. Box 4044, 7403635 Ness Ziona (IL). DAHARY, Dvir; c/o Imm¬ PACT-Bio Ltd., 2 Ilan Ramon St, P.O. Box 4044, 7403635 Ness Ziona (IL). -

Association Between the Ionotropic Glutamate Receptor Kainate 3
Molecular Psychiatry (2002) 7, 416–418 2002 Nature Publishing Group All rights reserved 1359-4184/02 $25.00 www.nature.com/mp ORIGINAL RESEARCH ARTICLE Association between the ionotropic glutamate receptor kainate 3 (GRIK3) ser310ala polymorphism and schizophrenia S Begni1, M Popoli2, S Moraschi1, S Bignotti3, GB Tura3 and M Gennarelli1 1Genetics Unit, IRCCS ‘S Giovanni di Dio’, Fatebenefratelli, 25123 Brescia, Italy; 2Center of Neuropharmacology, Institute of Pharmacological Sciences, University of Milan, 20133 Milan, Italy; 3Psychiatric Rehabilitation Unit, IRCCS ‘S Giovanni di Dio’, Fatebenefratelli, 25123 Brescia, Italy Keywords: association study; cSNP; expression; kainate through ionotropic glutamate receptors influences the receptor; neuronal plasticity regulation of transcriptional, translational and post- Schizophrenia is a severe psychiatric illness character- translational processes fundamental for the function of ised by disturbance of thought, hallucination and brain cells.3 delusions.1 Several studies have suggested that dys- One of the hypotheses about the molecular mech- functions in the glutamatergic transmission are linked anisms leading to schizophrenia is the presence of an to the pathogenesis of schizophrenia, and in particular excessive activation of glutamate receptors. An an excessive activation of glutamate receptors seems to increase in the basic metabolic activity along the gluta- be related to the disruption of neuronal ionic gradients matergic axons has been demonstrated by PET scan leading to excitotoxicity.2–7