1 Chemical Approaches to Modulating Complement-Mediated
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MASP-1, a Promiscuous Complement Protease: Structure of Its Catalytic Region Reveals the Basis of Its Broad Specificity 1
MASP-1, a promiscuous complement protease: structure of its catalytic region reveals the basis of its broad specificity 1 József Dobó 2,3* , Veronika Harmat 3† , László Beinrohr *, Edina Sebestyén *, Péter Závodszky *, Péter Gál 2* * Institute of Enzymology, Biological Research Center, Hungarian Academy of Sciences, Karolina út 29, H-1113, Budapest, Hungary † Protein Modeling Group, Hungarian Academy of Sciences, and Laboratory of Structural Chemistry and Biology, Institute of Chemistry, Eötvös Loránd University , Pázmány Péter sétány 1A, H-1117, Budapest, Hungary Running title: Structure of MASP-1 CCP1-CCP2-SP Keywords (not in the title): lectin pathway; innate immunity; modular serine protease; mannan-binding lectin; MBL-associated serine protease; MASP-2; C1r; C1s; thrombin; trypsin; factor D 1 Abstract Mannose-binding lectin (MBL)-associated serine protease-1 (MASP-1) is an abundant component of the lectin pathway of complement. The related enzyme, MASP-2 is capable of activating the complement cascade alone. Though the concentration of MASP-1 far exceeds that of MASP-2 only a supporting role of MASP-1 has been identified regarding lectin pathway activation. Several non-complement substrates, like fibrinogen and factor XIII, have also been reported. MASP-1 belongs to the C1r/C1s/MASP family of modular serine proteases, however its serine protease domain is evolutionary different. We have determined the crystal structure of the catalytic region of active MASP-1 and refined it to 2.55 Å resolution. Unusual features of the structure are: an internal salt bridge (similar to one in factor D) between the S1 Asp189 and Arg224, and a very long 60-loop. -

How Macrophages Deal with Death
REVIEWS CELL DEATH AND IMMUNITY How macrophages deal with death Greg Lemke Abstract | Tissue macrophages rapidly recognize and engulf apoptotic cells. These events require the display of so- called eat-me signals on the apoptotic cell surface, the most fundamental of which is phosphatidylserine (PtdSer). Externalization of this phospholipid is catalysed by scramblase enzymes, several of which are activated by caspase cleavage. PtdSer is detected both by macrophage receptors that bind to this phospholipid directly and by receptors that bind to a soluble bridging protein that is independently bound to PtdSer. Prominent among the latter receptors are the MER and AXL receptor tyrosine kinases. Eat-me signals also trigger macrophages to engulf virus- infected or metabolically traumatized, but still living, cells, and this ‘murder by phagocytosis’ may be a common phenomenon. Finally , the localized presentation of PtdSer and other eat- me signals on delimited cell surface domains may enable the phagocytic pruning of these ‘locally dead’ domains by macrophages, most notably by microglia of the central nervous system. In long- lived organisms, abundant cell types are often process. Efferocytosis is a remarkably efficient business: short- lived. In the human body, for example, the macrophages can engulf apoptotic cells in less than lifespan of many white blood cells — including neutro- 10 minutes, and it is therefore difficult experimentally to phils, eosinophils and platelets — is less than 2 weeks. detect free apoptotic cells in vivo, even in tissues where For normal healthy humans, a direct consequence of large numbers are generated7. Many of the molecules this turnover is the routine generation of more than that macrophages and other phagocytes use to recognize 100 billion dead cells each and every day of life1,2. -

Complement Component 3 (C3) Concentrations in Cancer Patients: a Systematic Review and Meta-Analysis
Complement Component 3 (C3) Concentrations in Cancer Patients: A Systematic Review and Meta-Analysis Zipeng Yang South China Agricultural University Zi-Guo Yuan ( [email protected] ) Anqun Yang Dapeng New District Nan'ao Peolple's Hospital of Shenzhen, Guangdong Province, China Xiu-Xiang Zhang South China Agricultural University College of Agriculture Xiaohu Wang Guangdong Academy of Agricultural Sciences, Guangzhou, Guangdong Province Miao Yu Dongfeng Xiyuan District, Stomatological Hospital Aliated to Guangzhou Medical University, Guangzhou Yasser S.Mahmmod Zagazig University Jorge A Hernandez University of Florida Zhaowen Ren South China Agricultural University Xirui Zhang South China Agricultural University Wei Cong Shandong University Research article Keywords: Complement Component 3, Cancer Patients, Meta-Analysis Posted Date: March 26th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-18256/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/17 Abstract Background The aim of this study was to investigate the association between the serum complement component 3 “C3” level and the patients with different types of cancer. Our study nding would ultimately provide reliable scientic conclusions to guide clinical practice. Methods PubMed, Embase, The Chorane Library and Google Scholar were systematically searched to identify all studies on serum C3 concentrations in cancer patients published as of September 2019. Additionally, we conducted a clinical study on serum C3 in lung cancer patients and healthy people. The levels of serum complement C3 in 84 lung cancer patients and 30 healthy people were examined by ELISA. We used standardized mean differences (SMD) to report the pooled estimation, and I² statistics were calculated to examine the heterogeneity. -

Complement Peptide C3a Receptor 1 Promotes Optic Nerve Degeneration in DBA/2J Mice Jeffrey M
Harder et al. Journal of Neuroinflammation (2020) 17:336 https://doi.org/10.1186/s12974-020-02011-z RESEARCH Open Access Complement peptide C3a receptor 1 promotes optic nerve degeneration in DBA/2J mice Jeffrey M. Harder1, Pete A. Williams1,2 , Catherine E. Braine1,3, Hongtian S. Yang1, Jocelyn M. Thomas1, Nicole E. Foxworth1, Simon W. M. John1,4,5* and Gareth R. Howell1,6,7* Abstract Background: The risk of glaucoma increases significantly with age and exposure to elevated intraocular pressure, two factors linked with neuroinflammation. The complement cascade is a complex immune process with many bioactive end-products, including mediators of inflammation. Complement cascade activation has been shown in glaucoma patients and models of glaucoma. However, the function of complement-mediated inflammation in glaucoma is largely untested. Here, the complement peptide C3a receptor 1 was genetically disrupted in DBA/2J mice, an ocular hypertensive model of glaucoma, to test its contribution to neurodegeneration. Methods: A null allele of C3ar1 was backcrossed into DBA/2J mice. Development of iris disease, ocular hypertension, optic nerve degeneration, retinal ganglion cell activity, loss of RGCs, and myeloid cell infiltration in C3ar1-deficient and sufficient DBA/2J mice were compared across multiple ages. RNA sequencing was performed on microglia from primary culture to determine global effects of C3ar1 on microglia gene expression. Results: Deficiency in C3ar1 lowered the risk of degeneration in ocular hypertensive mice without affecting intraocular pressure elevation at 10.5 months of age. Differences were found in the percentage of mice affected, but not in individual characteristics of disease progression. -

WO 2016/147053 Al 22 September 2016 (22.09.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/147053 Al 22 September 2016 (22.09.2016) P O P C T (51) International Patent Classification: (71) Applicant: RESVERLOGIX CORP. [CA/CA]; 300, A61K 31/551 (2006.01) A61P 37/02 (2006.01) 4820 Richard Road Sw, Calgary, AB, T3E 6L1 (CA). A61K 31/517 (2006.01) C07D 239/91 (2006.01) (72) Inventors: WASIAK, Sylwia; 431 Whispering Water (21) International Application Number: Trail, Calgary, AB, T3Z 3V1 (CA). KULIKOWSKI, PCT/IB20 16/000443 Ewelina, B.; 31100 Swift Creek Terrace, Calgary, AB, T3Z 0B7 (CA). HALLIDAY, Christopher, R.A.; 403 (22) International Filing Date: 138-18th Avenue SE, Calgary, AB, T2G 5P9 (CA). GIL- 10 March 2016 (10.03.2016) HAM, Dean; 249 Scenic View Close NW, Calgary, AB, (25) Filing Language: English T3L 1Y5 (CA). (26) Publication Language: English (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, (30) Priority Data: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, 62/132,572 13 March 2015 (13.03.2015) US BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, 62/264,768 8 December 2015 (08. 12.2015) US DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, [Continued on nextpage] (54) Title: COMPOSITIONS AND THERAPEUTIC METHODS FOR THE TREATMENT OF COMPLEMENT-ASSOCIATED DISEASES (57) Abstract: The invention comprises methods of modulating the complement cascade in a mammal and for treating and/or preventing diseases and disorders as sociated with the complement pathway by administering a compound of Formula I or Formula II, such as, for example, 2-(4-(2-hydroxyethoxy)-3,5-dimethylphenyl)- 5,7-dimethoxyquinazolin-4(3H)-one or a pharmaceutically acceptable salt thereof. -
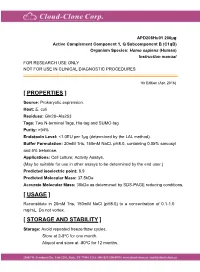
Active Complement Component 1, Q
APD208Hu01 200µg Active Complement Component 1, Q Subcomponent B (C1qB) Organism Species: Homo sapiens (Human) Instruction manual FOR RESEARCH USE ONLY NOT FOR USE IN CLINICAL DIAGNOSTIC PROCEDURES 1th Edition (Apr, 2016) [ PROPERTIES ] Source: Prokaryotic expression. Host: E. coli Residues: Gln28~Ala253 Tags: Two N-terminal Tags, His-tag and SUMO-tag Purity: >94% Endotoxin Level: <1.0EU per 1μg (determined by the LAL method). Buffer Formulation: 20mM Tris, 150mM NaCl, pH8.0, containing 0.05% sarcosyl and 5% trehalose. Applications: Cell culture; Activity Assays. (May be suitable for use in other assays to be determined by the end user.) Predicted isoelectric point: 8.9 Predicted Molecular Mass: 37.5kDa Accurate Molecular Mass: 38kDa as determined by SDS-PAGE reducing conditions. [ USAGE ] Reconstitute in 20mM Tris, 150mM NaCl (pH8.0) to a concentration of 0.1-1.0 mg/mL. Do not vortex. [ STORAGE AND STABILITY ] Storage: Avoid repeated freeze/thaw cycles. Store at 2-8oC for one month. Aliquot and store at -80oC for 12 months. Stability Test: The thermal stability is described by the loss rate. The loss rate was determined by accelerated thermal degradation test, that is, incubate the protein at 37oC for 48h, and no obvious degradation and precipitation were observed. The loss rate is less than 5% within the expiration date under appropriate storage condition. [ SEQUENCE ] [ ACTIVITY ] The complement component 1q (or simply C1q) is a protein complex involved in the complement system, which is part of the innate immune system. C1q together with C1r and C1s form the C1 complex. Antibodies of the adaptive immune system can bind antigen, forming an antigen-antibody complex. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

The Dual Role of Myeloperoxidase in Immune Response
International Journal of Molecular Sciences Review The Dual Role of Myeloperoxidase in Immune Response Jürgen Arnhold Institute of Medical Physics and Biophysics, Medical Faculty, Leipzig University, 04 107 Leipzig, Germany; [email protected] Received: 5 October 2020; Accepted: 28 October 2020; Published: 29 October 2020 Abstract: The heme protein myeloperoxidase (MPO) is a major constituent of neutrophils. As a key mediator of the innate immune system, neutrophils are rapidly recruited to inflammatory sites, where they recognize, phagocytose, and inactivate foreign microorganisms. In the newly formed phagosomes, MPO is involved in the creation and maintenance of an alkaline milieu, which is optimal in combatting microbes. Myeloperoxidase is also a key component in neutrophil extracellular traps. These helpful properties are contrasted by the release of MPO and other neutrophil constituents from necrotic cells or as a result of frustrated phagocytosis. Although MPO is inactivated by the plasma protein ceruloplasmin, it can interact with negatively charged components of serum and the extracellular matrix. In cardiovascular diseases and many other disease scenarios, active MPO and MPO-modified targets are present in atherosclerotic lesions and other disease-specific locations. This implies an involvement of neutrophils, MPO, and other neutrophil products in pathogenesis mechanisms. This review critically reflects on the beneficial and harmful functions of MPO against the background of immune response. Keywords: myeloperoxidase; neutrophils; immune response; phagosomes; cardiovascular diseases; chronic inflammation 1. Immune Response and Tissue Destruction In humans and higher animals, protection against different threats that affect the homeostasis of host’s tissues is ensured by a coordinated action of the immune system in close association with activation of components of the acute phase, complement, coagulation, and contact systems [1,2]. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Complement Component 4 Genes Contribute Sex-Specific Vulnerability in Diverse Illnesses
bioRxiv preprint doi: https://doi.org/10.1101/761718; this version posted September 9, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Complement component 4 genes contribute sex-specific vulnerability in diverse illnesses Nolan Kamitaki1,2, Aswin Sekar1,2, Robert E. Handsaker1,2, Heather de Rivera1,2, Katherine Tooley1,2, David L. Morris3, Kimberly E. Taylor4, Christopher W. Whelan1,2, Philip Tombleson3, Loes M. Olde Loohuis5,6, Schizophrenia Working Group of the Psychiatric Genomics Consortium7, Michael Boehnke8, Robert P. Kimberly9, Kenneth M. Kaufman10, John B. Harley10, Carl D. Langefeld11, Christine E. Seidman1,12,13, Michele T. Pato14, Carlos N. Pato14, Roel A. Ophoff5,6, Robert R. Graham15, Lindsey A. Criswell4, Timothy J. Vyse3, Steven A. McCarroll1,2 1 Department of Genetics, Harvard Medical School, Boston, Massachusetts 02115, USA 2 Stanley Center for Psychiatric Research, Broad Institute of MIT and Harvard, Cambridge, Massachusetts 02142, USA 3 Department of Medical and Molecular Genetics, King’s College London, London WC2R 2LS, UK 4 Rosalind Russell / Ephraim P Engleman Rheumatology Research Center, Division of Rheumatology, UCSF School of Medicine, San Francisco, California 94143, USA 5 Department of Human Genetics, David Geffen School of Medicine, University of California, Los Angeles, California 90095, USA 6 Center for Neurobehavioral Genetics, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, California 90095, USA 7 A full list of collaborators is in Supplementary Information. -

Assembly of an Integrated Human Lung Cell Atlas Reveals That
medRxiv preprint doi: https://doi.org/10.1101/2020.06.02.20120634; this version posted June 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Assembly of an integrated human lung cell atlas reveals that SARS-CoV-2 receptor is co-expressed with key elements of the kinin-kallikrein, renin-angiotensin and coagulation systems in alveolar cells Davi Sidarta-Oliveira1,2, Carlos Poblete Jara1,3, Adriano J. Ferruzzi4, Munir S. Skaf4, William H. Velander5, Eliana P. Araujo1,3, Licio A. Velloso1 1Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Brazil 2 Physician-Scientist Graduate Program, School of Medical Sciences, University of Campinas, Brazil 3Nursing School, University of Campinas, Brazil 4Institute of Chemistry and Center for Computing in Engineering and Sciences University of Campinas, Brazil 5Department of Chemical and Biomolecular Engineering, University of Nebraska, Lincoln, USA Correspondence: Licio A. Velloso Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Campinas, Brazil Address: Rua Carl Von Lineaus s/n, Instituto de Biologia - Bloco Z. Campus Universitário Zeferino Vaz - Barão Geraldo, Campinas - SP, 13083-864 Phone: +55 19 3521-0025 E-mail: [email protected] Abstract SARS-CoV-2, the pathogenic agent of COVID-19, employs angiotensin converting enzyme-2 (ACE2) as its cell entry receptor. Clinical data reveal that in severe COVID- 19, SARS-CoV-2 infects the lung, leading to a frequently lethal triad of respiratory insufficiency, acute cardiovascular failure, and coagulopathy. -

The CXCR4 Antagonist AMD3100 Impairs Survival of Human AML Cells and Induces Their Differentiation
Leukemia (2008) 22, 2151–2158 & 2008 Macmillan Publishers Limited All rights reserved 0887-6924/08 $32.00 www.nature.com/leu ORIGINAL ARTICLE The CXCR4 antagonist AMD3100 impairs survival of human AML cells and induces their differentiation S Tavor1, M Eisenbach1, J Jacob-Hirsch2, T Golan1, I Petit1, K BenZion1, S Kay1, S Baron1, N Amariglio2, V Deutsch1, E Naparstek1 and G Rechavi2 1Institute of Hematology and Bone Marrow Transplantation, Sourasky Medical Center, Tel Aviv, Israel and 2Cancer Research Center, Sheba Medical Center, Tel-Hashomer, and Sackler School of Medicine, Tel Aviv University, Tel Aviv, Israel The chemokine stromal cell-derived factor-1 (SDF-1) and its NOD/SCID mice, homing and subsequent engraftment of human receptor, CXCR4, participate in the retention of acute myelo- normal or AML stem cells are dependent on the expression of cell blastic leukemia (AML) cells within the bone marrow micro- 9–12 environment and their release into the circulation. AML cells surface CXCR4 and SDF-1 produced within the murine. In also constitutively express SDF-1-dependent elastase, which addition to controlling cell motility, SDF-1 regulates cell regulates their migration and proliferation. To study the proliferation, induces cell cycle progression and acts as a survival molecular events and genes regulated by the SDF-1/CXCR4 factor for normal human stem cells and AML cells.13–16 axis and elastase in AML cells, we examined gene expression CXCR4 blockage in AML cells, using the polypeptide profiles of the AML cell line, U937, under treatment with a RCP168, enhanced chemotherapy-induced apoptosis in vitro.17 neutralizing anti-CXCR4 antibody or elastase inhibitor, as compared with non-treated cells, using DNA microarray Most importantly, high CXCR4 expression level in leukemic technology.