Did Internet-Purchased Diet Pills Cause Serotonin Syndrome?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Pharmacology and Toxicology of Amphetamine and Related Designer Drugs
Pharmacology and Toxicology of Amphetamine and Related Designer Drugs U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol Drug Abuse and Mental Health Administration Pharmacology and Toxicology of Amphetamine and Related Designer Drugs Editors: Khursheed Asghar, Ph.D. Division of Preclinical Research National Institute on Drug Abuse Errol De Souza, Ph.D. Addiction Research Center National Institute on Drug Abuse NIDA Research Monograph 94 1989 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 Pharmacology and Toxicology of Amphetamine and Related Designer Drugs ACKNOWLEDGMENT This monograph is based upon papers and discussion from a technical review on pharmacology and toxicology of amphetamine and related designer drugs that took place on August 2 through 4, 1988, in Bethesda, MD. The review meeting was sponsored by the Biomedical Branch, Division of Preclinical Research, and the Addiction Research Center, National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other matieral in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. -

18 Chapter 1631
18 Gas chromatography S Dawling, S Jickells and A Negrusz Introduction . 469 Quantitative determinations . 505 Gas chromatography Optimising operation conditions to columns . 470 customise applications . 506 Inlet systems . 483 Specific applications. 508 Detector systems . 493 References . 510 Specimen preparation . 498 Further reading . 511 Introduction When a mixture of substances is injected at the inlet, each component partitions between the Gas chromatography (GC) is applicable to a wide stationary phase and the gas phase as it is swept range of compounds of interest to toxicologists, towards the detector. Molecules that have greater pharmaceutical and industrial chemists, envir- affinity for the stationary phase spend more time onmentalists and clinicians. Adsorption GC was in that phase and consequently take longer to developed by a German scientist, Fritz Prior, in reach the detector. The detector produces a the late 1940s. In the early 1950s Archer J. P. signal proportional to the amount of substance Martin and Richard L. M. Synge, two scientists that passes through it, and this signal is from the UK, invented partition chromatog- processed and fed to an integrator or some other raphy, for which they received the Nobel Prize in recording device. Each substance that elutes chemistry in 1952. This marks a true beginning from the column has a characteristic retention of GC as a broadly used analytical technique. If time, defined as the time interval from injection a compound has sufficient volatility for its mo- to peak detector response. Figure 18.1 shows a lecules to be in the gas or vapour phase at or schematic of a GC system. -

The Effects of Aminorex and Related Compounds on Brain Monoamines and Metabolites in CBA Mice
I p_._rmPharmac0l. 1997, 49:89-96 © 1997 J. Phann. Pharmacol. ._, A R_ce;vedMr.,' 29, 1996 AcceptedJuly 4, 1996 The Effects of Aminorex and Related Compounds on Brain Monoamines and Metabolites in CBA Mice YIWEN ZHENO, BRUCE RUSSELL, DAVID SCHMIERER* AND RICHARDLAVERTY Department of Pharmacology and *School of Pharmacy, University of Otago, P.O. Box 913, Dunedin, New Zealand Abstract Acute and long-term neurochemical effects of aminorex, an appetite-suppressing drug related to amphetamine in chemical structure, and stereoisomers of its analogues were examined and compared with those of 3,4- methylenedioxymethylamphetamine (MDMA) and fenfluramine. Aminorex and its analogues, with exception of 4S, 5S-dimethylaminorex, did not cause the long-term neurotransmitter depletion in either the dopaminergic or 5-HT-ergic systems that was observed after MDMA or fenfluramine in CBA mice. These results are discussed in terms of possible structurally related mechanisms of neurotoxicity. The acute neurochemical effects showed that aminorex and analogues all produced increases in 5- hydroxytryptamine (5-HT) levels, unlike fenfiuramine and MDMA in the present study or in published data. This suggests that inhibition of 5-HT metabolism, rather than direct 5-HT release, may be involved in their anorectic effect. The parallel study of acute doparnine and 3,4-dihydroxyphenylacetic acid (DOPAC) changes suggest that in CBA mice MDMA may he a better doparnine releaser and this may contribute to its dopaminergic neurotoxicity. However the ability to release doparnine or 5-HT, or both, may be important, but not the only factor involved in causing the long-term neurotoxicity observed with amphetamine derivatives. -

Annex 2B Tariff Schedule of the United States See General Notes to Annex 2B for Staging Explanation HTSUS No
Annex 2B Tariff Schedule of the United States See General Notes to Annex 2B for Staging Explanation HTSUS No. Description Base Rate Staging 0101 Live horses, asses, mules and hinnies: 0101.10.00 -Purebred breeding animals Free E 0101.90 -Other: 0101.90.10 --Horses Free E 0101.90.20 --Asses 6.8% B --Mules and hinnies: 0101.90.30 ---Imported for immediate slaughter Free E 0101.90.40 ---Other 4.5% A 0102 Live bovine animals: 0102.10.00 -Purebred breeding animals Free E 0102.90 -Other: 0102.90.20 --Cows imported specially for dairy purposes Free E 0102.90.40 --Other 1 cent/kg A 0103 Live swine: 0103.10.00 -Purebred breeding animals Free E -Other: 0103.91.00 --Weighing less than 50 kg each Free E 0103.92.00 --Weighing 50 kg or more each Free E 0104 Live sheep and goats: 0104.10.00 -Sheep Free E 0104.20.00 -Goats 68 cents/head A 0105 Live poultry of the following kinds: Chickens, ducks, geese, turkeys and guineas: -Weighing not more than 185 g: 0105.11.00 --Chickens 0.9 cents each A 0105.12.00 --Turkeys 0.9 cents each A 0105.19.00 --Other 0.9 cents each A -Other: 0105.92.00 --Chickens, weighing not more than 2,000 g 2 cents/kg A 0105.93.00 --Chickens, weighing more than 2,000 g 2 cents/kg A 0105.99.00 --Other 2 cents/kg A 0106 Other live animals: -Mammals: 0106.11.00 --Primates Free E 0106.12.00 --Whales, dolphins and porpoises (mammals of the order Cetacea); manatees and dugongs (mammals of the order Sirenia) Free E 0106.19 --Other: 2B-Schedule-1 HTSUS No. -

Pharmaceuticals Appendix
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ADAPALENE 106685-40-9 ABANOQUIL 90402-40-7 ADAPROLOL 101479-70-3 ABECARNIL 111841-85-1 ADEMETIONINE 17176-17-9 ABLUKAST 96566-25-5 ADENOSINE PHOSPHATE 61-19-8 ABUNIDAZOLE 91017-58-2 ADIBENDAN 100510-33-6 ACADESINE 2627-69-2 ADICILLIN 525-94-0 ACAMPROSATE 77337-76-9 ADIMOLOL 78459-19-5 ACAPRAZINE 55485-20-6 ADINAZOLAM 37115-32-5 ACARBOSE 56180-94-0 ADIPHENINE 64-95-9 ACEBROCHOL 514-50-1 ADIPIODONE 606-17-7 ACEBURIC ACID 26976-72-7 ADITEREN 56066-19-4 ACEBUTOLOL 37517-30-9 ADITOPRIME 56066-63-8 ACECAINIDE 32795-44-1 ADOSOPINE 88124-26-9 ACECARBROMAL 77-66-7 ADOZELESIN 110314-48-2 ACECLIDINE 827-61-2 ADRAFINIL 63547-13-7 ACECLOFENAC 89796-99-6 ADRENALONE 99-45-6 ACEDAPSONE 77-46-3 AFALANINE 2901-75-9 ACEDIASULFONE SODIUM 127-60-6 AFLOQUALONE 56287-74-2 ACEDOBEN 556-08-1 AFUROLOL 65776-67-2 ACEFLURANOL 80595-73-9 AGANODINE 86696-87-9 ACEFURTIAMINE 10072-48-7 AKLOMIDE 3011-89-0 ACEFYLLINE CLOFIBROL 70788-27-1 -
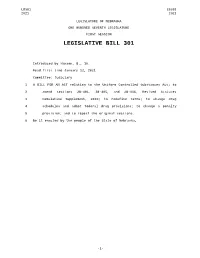
Introduced B.,Byhansen, 16
LB301 LB301 2021 2021 LEGISLATURE OF NEBRASKA ONE HUNDRED SEVENTH LEGISLATURE FIRST SESSION LEGISLATIVE BILL 301 Introduced by Hansen, B., 16. Read first time January 12, 2021 Committee: Judiciary 1 A BILL FOR AN ACT relating to the Uniform Controlled Substances Act; to 2 amend sections 28-401, 28-405, and 28-416, Revised Statutes 3 Cumulative Supplement, 2020; to redefine terms; to change drug 4 schedules and adopt federal drug provisions; to change a penalty 5 provision; and to repeal the original sections. 6 Be it enacted by the people of the State of Nebraska, -1- LB301 LB301 2021 2021 1 Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2 2020, is amended to read: 3 28-401 As used in the Uniform Controlled Substances Act, unless the 4 context otherwise requires: 5 (1) Administer means to directly apply a controlled substance by 6 injection, inhalation, ingestion, or any other means to the body of a 7 patient or research subject; 8 (2) Agent means an authorized person who acts on behalf of or at the 9 direction of another person but does not include a common or contract 10 carrier, public warehouse keeper, or employee of a carrier or warehouse 11 keeper; 12 (3) Administration means the Drug Enforcement Administration of the 13 United States Department of Justice; 14 (4) Controlled substance means a drug, biological, substance, or 15 immediate precursor in Schedules I through V of section 28-405. 16 Controlled substance does not include distilled spirits, wine, malt 17 beverages, tobacco, hemp, or any nonnarcotic substance if such substance 18 may, under the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. -
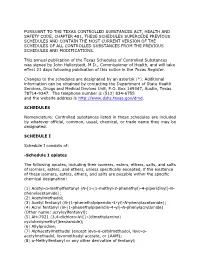
Schedules of Controlled Substances (.Pdf)
PURSUANT TO THE TEXAS CONTROLLED SUBSTANCES ACT, HEALTH AND SAFETY CODE, CHAPTER 481, THESE SCHEDULES SUPERCEDE PREVIOUS SCHEDULES AND CONTAIN THE MOST CURRENT VERSION OF THE SCHEDULES OF ALL CONTROLLED SUBSTANCES FROM THE PREVIOUS SCHEDULES AND MODIFICATIONS. This annual publication of the Texas Schedules of Controlled Substances was signed by John Hellerstedt, M.D., Commissioner of Health, and will take effect 21 days following publication of this notice in the Texas Register. Changes to the schedules are designated by an asterisk (*). Additional information can be obtained by contacting the Department of State Health Services, Drugs and Medical Devices Unit, P.O. Box 149347, Austin, Texas 78714-9347. The telephone number is (512) 834-6755 and the website address is http://www.dshs.texas.gov/dmd. SCHEDULES Nomenclature: Controlled substances listed in these schedules are included by whatever official, common, usual, chemical, or trade name they may be designated. SCHEDULE I Schedule I consists of: -Schedule I opiates The following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, unless specifically excepted, if the existence of these isomers, esters, ethers, and salts are possible within the specific chemical designation: (1) Acetyl-α-methylfentanyl (N-[1-(1-methyl-2-phenethyl)-4-piperidinyl]-N- phenylacetamide); (2) Acetylmethadol; (3) Acetyl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacetamide); (4) Acryl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacrylamide) (Other name: -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

Effect of Phenmetrazine, Aminorex and (+)P-Chloramphetamine on The
Br. J. Pharmac. (1971), 43, 570-579. Effect of phenmetrazine, aminorex and (+) p-chloramphetamine on the motor activity and turnover rate of brain catecholamines E. COSTA, K. M. NAIMZADA* AND A. REVUELTA Laboratory of Preclinical Pharmacology, National Institute of Mental Health, Saint Elizabeth's Hospital, Washington, DC 20032, USA Summary 1. The minimal doses (umol/kg i.v.) of phenmetrazine, (±)-p-chloramphet- amine, and aminorex which increase motor activity are 5 6, 3 5, and 1-5, respec- tively. We detected stereotype behaviour neither in rats receiving intravenous doses 3 times greater nor in animals injected intraperitoneally with 44, 62 and 112 tumol/kg of (±)-p-chloramphetamine, aminorex and phenmatrazine, respectively. 2. The latter doses of the three amphetamine congeners were tested for their action on tissue monoamine content. Only (± )-p-chloramphetamine decreased the concentration of tel-diencephalon 5-hydroxytryptamine (5-HT) and this decrease lasted longer than 24 hours. This and the other two amphetamine congeners failed to affect the concentration of noradrenaline (NA) in brain, heart and lung. 3. Aminorex (1P5 mol/kg i.v.) and (±)-p-chloramphetamine (35 ,umol/kg i.v.) decreased the turnover time of striatum dopamine (DM) but failed to change the turnover time of tel-diencephalon and brainstem NA. Phenmetrazine (5-6 tumol/kg i.v.) changed neither the turnover time of striatum DM nor that of NA in the two brain areas assayed. Introduction Release of neuronal noradrenaline (NA) mediates many actions of (+)-amphet- amine, including psychomotor stimulation (Trendelenburg, Muskus, Flemming & Alonso de la Sierra, 1962; Stein, 1964; Rech, 1964; Weissman, Koe & Tenen, 1966; Sulser, Owens, Norvich & Dingell, 1968; Rech & Stalk, 1970). -

Laws 2021, LB236, § 4
LB236 LB236 2021 2021 LEGISLATIVE BILL 236 Approved by the Governor May 26, 2021 Introduced by Brewer, 43; Clements, 2; Erdman, 47; Slama, 1; Lindstrom, 18; Murman, 38; Halloran, 33; Hansen, B., 16; McDonnell, 5; Briese, 41; Lowe, 37; Groene, 42; Sanders, 45; Bostelman, 23; Albrecht, 17; Dorn, 30; Linehan, 39; Friesen, 34; Aguilar, 35; Gragert, 40; Kolterman, 24; Williams, 36; Brandt, 32. A BILL FOR AN ACT relating to law; to amend sections 28-1202 and 69-2436, Reissue Revised Statutes of Nebraska, and sections 28-401 and 28-405, Revised Statutes Cumulative Supplement, 2020; to redefine terms, change drug schedules, and adopt federal drug provisions under the Uniform Controlled Substances Act; to provide an exception to the offense of carrying a concealed weapon as prescribed; to define a term; to change provisions relating to renewal of a permit to carry a concealed handgun; to provide a duty for the Nebraska State Patrol; to eliminate an obsolete provision; to harmonize provisions; and to repeal the original sections. Be it enacted by the people of the State of Nebraska, Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2020, is amended to read: 28-401 As used in the Uniform Controlled Substances Act, unless the context otherwise requires: (1) Administer means to directly apply a controlled substance by injection, inhalation, ingestion, or any other means to the body of a patient or research subject; (2) Agent means an authorized person who acts on behalf of or at the direction of another person but does not include a common or contract carrier, public warehouse keeper, or employee of a carrier or warehouse keeper; (3) Administration means the Drug Enforcement Administration of the United States Department of Justice; (4) Controlled substance means a drug, biological, substance, or immediate precursor in Schedules I through V of section 28-405. -

(12) United States Patent (10) Patent No.: US 8,101,661 B2 Mickle (45) Date of Patent: *Jan
USOO81 01661 B2 (12) United States Patent (10) Patent No.: US 8,101,661 B2 Mickle (45) Date of Patent: *Jan. 24, 2012 (54) POLAR HYDROPHILIC PRODRUGS AND W 388-39. 358. NON-STANDARDAMNO ACID CONUGATES OF AMPHETAMINE AND WO 2008/098151 8, 2008 OTHER STIMULANTS AND PROCESSES FOR OTHER PUBLICATIONS MAKING AND USING THE SAME European Patent Office, Communication dated Jun. 8, 2010, in EP Application No. 07869 098.9. (75) Inventor: Travis C. Mickle, Coralville, IA (US) Amy Sorter, Understanding ADHD Stimulant Abuse, Publication, Vitality Drug Free Work, 2002. (http://12.42.224.168/HealthyLiv (73) Assignee: KemPharm, Inc., North Libery, IA (US) ing family homeljan04 family homestimulantabuse.htm). International Preliminary Report on Patentability for PCT Interna (*) Notice: Subject to any disclaimer, the term of this tional Application No. PCT/US08/53363, dated Nov. 6, 2008. Davankova et al., “Synthesis and Pharmacological Properties of N patent is extended or adjusted under 35 Aminoacyl Derivatives of Beta Phenyl ISO Propylamine.” Pharma U.S.C. 154(b) by 0 days. ceutical Chemistry Journal, vol. 9, No. 3, 1975. G.C. Barrett, D.T. Elmore; Methods for Peptide Bonds Amino Acids This patent is Subject to a terminal dis and Peptides; 1st Edition, Cambridge University Press, UK, 1998, pp. claimer. 151-156. International Search Report and Written Opinion corresponding to (21) Appl. No.: 12/843,169 International Application Serial No. PCT/US08/53363, mailed Nov. 6, 2008, 19 pages. (22) Filed: Jul. 26, 2010 J. Jones; Amino Acid and Peptide Synthesis; 2nd Edition, Oxford University Press, UK, 2002, pp. 25-41.