About Autism Script
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hakuin on Kensho: the Four Ways of Knowing/Edited with Commentary by Albert Low.—1St Ed
ABOUT THE BOOK Kensho is the Zen experience of waking up to one’s own true nature—of understanding oneself to be not different from the Buddha-nature that pervades all existence. The Japanese Zen Master Hakuin (1689–1769) considered the experience to be essential. In his autobiography he says: “Anyone who would call himself a member of the Zen family must first achieve kensho- realization of the Buddha’s way. If a person who has not achieved kensho says he is a follower of Zen, he is an outrageous fraud. A swindler pure and simple.” Hakuin’s short text on kensho, “Four Ways of Knowing of an Awakened Person,” is a little-known Zen classic. The “four ways” he describes include the way of knowing of the Great Perfect Mirror, the way of knowing equality, the way of knowing by differentiation, and the way of the perfection of action. Rather than simply being methods for “checking” for enlightenment in oneself, these ways ultimately exemplify Zen practice. Albert Low has provided careful, line-by-line commentary for the text that illuminates its profound wisdom and makes it an inspiration for deeper spiritual practice. ALBERT LOW holds degrees in philosophy and psychology, and was for many years a management consultant, lecturing widely on organizational dynamics. He studied Zen under Roshi Philip Kapleau, author of The Three Pillars of Zen, receiving transmission as a teacher in 1986. He is currently director and guiding teacher of the Montreal Zen Centre. He is the author of several books, including Zen and Creative Management and The Iron Cow of Zen. -

Active Play: Simple Games and Activity Ideas
Active Play: Simple Games and Activity Ideas Children have different needs and abilities depending upon their age. Children need a safe environment that promotes and encourages their physical, intellectual, emotional and social growth. Keep the ages and needs of the children in your care in mind when planning games and activities. Younger children have shorter attention spans, and are just learning how to coordinator their bodies, while older children may get bored with not enough of a “challenge” in the game or activities. Read more about children’s developmental ages and stages: Growth and Development Child’s Development Ages & Stages Go, Go, Stop Pick a leader, and start and end spots. Have children line up at the start and the leader stand at the end with his back to the children. The object is to get to the end where the leader is. Have the leader yell go, go, go for a few seconds (i.e., 2 second, 10 seconds, etc.) and then yell stop. All children stop and freeze. If the leader turns around and sees any child moving, that child has to go back to the starting spot. The game ends when a child touches the leader. Follow the Leader To begin the game, you may want an adult to lead. Children line up behind the leader. The leader decides the actions for children to follow. The children mimic the leader's actions. Any players who fail to follow or do what the leader does are out of the game. Change leaders and give every child time to lead the others. -
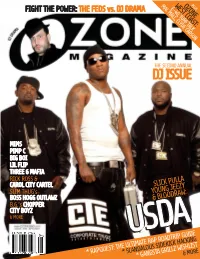
Dj Issue Can’T Explain Just What Attracts Me to This Dirty Game
MAC MALL,WEST CLYDEOZONE COAST:CARSONPLUS E-40, TURF TALK OZONE MAGAZINE MAGAZINE OZONE FIGHT THE POWER: THE FEDS vs. DJ DRAMA THE SECOND ANNUAL DJ ISSUE CAN’T EXPLAIN JUST WHAT ATTRACTS ME TO THIS DIRTY GAME ME TO ATTRACTS JUST WHAT MIMS PIMP C BIG BOI LIL FLIP THREE 6 MAFIA RICK ROSS & CAROL CITY CARTEL SLICK PULLA SLIM THUG’s YOUNG JEEZY BOSS HOGG OUTLAWZ & BLOODRAW: B.G.’s CHOPPER CITY BOYZ & MORE APRIL 2007 USDAUSDAUSDA * SCANDALOUS SIDEKICK HACKING * RAPQUEST: THE ULTIMATE* GANGSTA RAP GRILLZ ROADTRIP &WISHLIST MORE GUIDE MAC MALL,WEST CLYDEOZONE COAST:CARSONPLUS REAL, RAW, & UNCENSORED SOUTHERN RAP E-40, TURF TALK FIGHT THE POWER: THE FEDS vs. DJ DRAMA THE SECOND ANNUAL DJ ISSUE MIMS PIMP C LIL FLIP THREE 6 MAFIA & THE SLIM THUG’s BOSS HOGG OUTLAWZ BIG BOI & PURPLE RIBBON RICK ROSS B.G.’s CHOPPER CITY BOYZ YOUNG JEEZY’s USDA CAROL CITY & MORE CARTEL* RAPQUEST: THE* SCANDALOUS ULTIMATE RAP SIDEKICK ROADTRIP& HACKING MORE GUIDE * GANGSTA GRILLZ WISHLIST OZONE MAG // 11 PUBLISHER/EDITOR-IN-CHIEF // Julia Beverly CHIEF OPERATIONS OFFICER // N. Ali Early MUSIC EDITOR // Randy Roper FEATURES EDITOR // Eric Perrin ART DIRECTOR // Tene Gooden ADVERTISING SALES // Che’ Johnson PROMOTIONS DIRECTOR // Malik Abdul MARKETING DIRECTOR // David Muhammad LEGAL CONSULTANT // Kyle P. King, P.A. SUBSCRIPTIONS MANAGER // Destine Cajuste ADMINISTRATIVE // Cordice Gardner, Kisha Smith CONTRIBUTORS // Alexander Cannon, Bogan, Carlton Wade, Charlamagne the God, Chuck T, E-Feezy, Edward Hall, Felita Knight, Iisha Hillmon, Jacinta Howard, Jaro Vacek, Jessica INTERVIEWS Koslow, J Lash, Jason Cordes, Jo Jo, Joey Columbo, Johnny Louis, Kamikaze, Keadron Smith, Keith Kennedy, Kenneth Brewer, K.G. -

Whittaker, Jim RFK #1
Jim Whittaker Oral History Interview –RFK #1, 4/25/1969 Administrative Information Creator: Jim Whittaker Interviewer: Roberta W. Greene Date of Interview: April 25, 1969 Place of Interview: Hickory Hill, McLean, Virginia Length: 21 pp. Biographical Note Whittaker, Jim; Friend, associate, Robert F. Kennedy, 1965-1968; expedition leader, National Geographic climb, Mt. Kennedy, Yukon, Canada, 1965; campaign worker, Robert F. Kennedy for President, 1968. Whittaker discusses the climb he led up Mount Kennedy which included Senator Robert F. Kennedy [RFK], the formation of their relationship due to this trip, and his thoughts on RFK’s personality, among other issues. Access Restrictions No restrictions. Usage Restrictions According to the deed of gift signed January 8, 1991, copyright of these materials has been assigned to the United States Government. Users of these materials are advised to determine the copyright status of any document from which they wish to publish. Copyright The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be “used for any purpose other than private study, scholarship, or research.” If a user makes a request for, or later uses, a photocopy or reproduction for purposes in excesses of “fair use,” that user may be liable for copyright infringement. This institution reserves the right to refuse to accept a copying order if, in its judgment, fulfillment of the order would involve violation of copyright law. -

The Wonders of the Invisible World. Observations As Well Historical As Theological, Upon the Nature, the Number, and the Operations of the Devils (1693)
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Electronic Texts in American Studies Libraries at University of Nebraska-Lincoln 1693 The Wonders of the Invisible World. Observations as Well Historical as Theological, upon the Nature, the Number, and the Operations of the Devils (1693) Cotton Mather Second Church (Congregational), Boston Reiner Smolinski , Editor Georgia State University, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/etas Part of the American Studies Commons Mather, Cotton and Smolinski, Reiner , Editor, "The Wonders of the Invisible World. Observations as Well Historical as Theological, upon the Nature, the Number, and the Operations of the Devils (1693)" (1693). Electronic Texts in American Studies. 19. https://digitalcommons.unl.edu/etas/19 This Article is brought to you for free and open access by the Libraries at University of Nebraska-Lincoln at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Electronic Texts in American Studies by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. The Wonders of the Invisible World: COTTON MATHER (1662/3–1727/8). The eldest son of New England’s leading divine, Increase Mather and grand- Observations as Well Historical as Theological, son of the colony’s spiritual founders Richard Mather and John Cotton, Mather was born in Boston, educated at Har- upon the Nature, the Number, and the vard (B. A. 1678; M. A. 1681), and received an honorary Doctor of Divinity degree from Glasgow University (1710). Operations of the Devils As pastor of Boston’s Second Church (Congregational), he came into the political limelight during America’s version [1693] of the Glorious Revolution, when Bostonians deposed their royal governor, Sir Edmund Andros (April 1689). -

Idioms-And-Expressions.Pdf
Idioms and Expressions by David Holmes A method for learning and remembering idioms and expressions I wrote this model as a teaching device during the time I was working in Bangkok, Thai- land, as a legal editor and language consultant, with one of the Big Four Legal and Tax companies, KPMG (during my afternoon job) after teaching at the university. When I had no legal documents to edit and no individual advising to do (which was quite frequently) I would sit at my desk, (like some old character out of a Charles Dickens’ novel) and prepare language materials to be used for helping professionals who had learned English as a second language—for even up to fifteen years in school—but who were still unable to follow a movie in English, understand the World News on TV, or converse in a colloquial style, because they’d never had a chance to hear and learn com- mon, everyday expressions such as, “It’s a done deal!” or “Drop whatever you’re doing.” Because misunderstandings of such idioms and expressions frequently caused miscom- munication between our management teams and foreign clients, I was asked to try to as- sist. I am happy to be able to share the materials that follow, such as they are, in the hope that they may be of some use and benefit to others. The simple teaching device I used was three-fold: 1. Make a note of an idiom/expression 2. Define and explain it in understandable words (including synonyms.) 3. Give at least three sample sentences to illustrate how the expression is used in context. -

8123 Songs, 21 Days, 63.83 GB
Page 1 of 247 Music 8123 songs, 21 days, 63.83 GB Name Artist The A Team Ed Sheeran A-List (Radio Edit) XMIXR Sisqo feat. Waka Flocka Flame A.D.I.D.A.S. (Clean Edit) Killer Mike ft Big Boi Aaroma (Bonus Version) Pru About A Girl The Academy Is... About The Money (Radio Edit) XMIXR T.I. feat. Young Thug About The Money (Remix) (Radio Edit) XMIXR T.I. feat. Young Thug, Lil Wayne & Jeezy About Us [Pop Edit] Brooke Hogan ft. Paul Wall Absolute Zero (Radio Edit) XMIXR Stone Sour Absolutely (Story Of A Girl) Ninedays Absolution Calling (Radio Edit) XMIXR Incubus Acapella Karmin Acapella Kelis Acapella (Radio Edit) XMIXR Karmin Accidentally in Love Counting Crows According To You (Top 40 Edit) Orianthi Act Right (Promo Only Clean Edit) Yo Gotti Feat. Young Jeezy & YG Act Right (Radio Edit) XMIXR Yo Gotti ft Jeezy & YG Actin Crazy (Radio Edit) XMIXR Action Bronson Actin' Up (Clean) Wale & Meek Mill f./French Montana Actin' Up (Radio Edit) XMIXR Wale & Meek Mill ft French Montana Action Man Hafdís Huld Addicted Ace Young Addicted Enrique Iglsias Addicted Saving abel Addicted Simple Plan Addicted To Bass Puretone Addicted To Pain (Radio Edit) XMIXR Alter Bridge Addicted To You (Radio Edit) XMIXR Avicii Addiction Ryan Leslie Feat. Cassie & Fabolous Music Page 2 of 247 Name Artist Addresses (Radio Edit) XMIXR T.I. Adore You (Radio Edit) XMIXR Miley Cyrus Adorn Miguel Adorn Miguel Adorn (Radio Edit) XMIXR Miguel Adorn (Remix) Miguel f./Wiz Khalifa Adorn (Remix) (Radio Edit) XMIXR Miguel ft Wiz Khalifa Adrenaline (Radio Edit) XMIXR Shinedown Adrienne Calling, The Adult Swim (Radio Edit) XMIXR DJ Spinking feat. -

Mediamonkey Filelist
MediaMonkey Filelist Track # Artist Title Length Album Year Genre Rating Bitrate Media # Local 1 Kirk Franklin Just For Me 5:11 2019 Gospel 182 Disk Local 2 Kanye West I Love It (Clean) 2:11 2019 Rap 4 128 Disk Closer To My Local 3 Drake 5:14 2014 Rap 3 128 Dreams (Clean) Disk Nellie Tager Local 4 If I Back It Up 3:49 2018 Soul 3 172 Travis Disk Local 5 Ariana Grande The Way 3:56 The Way 1 2013 RnB 2 190 Disk Drop City Yacht Crickets (Remix Local 6 5:16 T.I. Remix (Intro 2013 Rap 128 Club Intro - Clean) Disk In The Lonely I'm Not the Only Local 7 Sam Smith 3:59 Hour (Deluxe 5 2014 Pop 190 One Disk Version) Block Brochure: In This Thang Local 8 E40 3:09 Welcome to the 16 2012 Rap 128 Breh Disk Soil 1, 2 & 3 They Don't Local 9 Rico Love 4:55 1 2014 Rap 182 Know Disk Return Of The Local 10 Mann 3:34 Buzzin' 2011 Rap 3 128 Macc (Remix) Disk Local 11 Trey Songz Unusal 4:00 Chapter V 2012 RnB 128 Disk Sensual Local 12 Snoop Dogg Seduction 5:07 BlissMix 7 2012 Rap 0 201 Disk (BlissMix) Same Damn Local 13 Future Time (Clean 4:49 Pluto 11 2012 Rap 128 Disk Remix) Sun Come Up Local 14 Glasses Malone 3:20 Beach Cruiser 2011 Rap 128 (Clean) Disk I'm On One We the Best Local 15 DJ Khaled 4:59 2 2011 Rap 5 128 (Clean) Forever Disk Local 16 Tessellated Searchin' 2:29 2017 Jazz 2 173 Disk Rahsaan 6 AM (Clean Local 17 3:29 Bleuphoria 2813 2011 RnB 128 Patterson Remix) Disk I Luh Ya Papi Local 18 Jennifer Lopez 2:57 1 2014 Rap 193 (Remix) Disk Local 19 Mary Mary Go Get It 2:24 Go Get It 1 2012 Gospel 4 128 Disk LOVE? [The Local 20 Jennifer Lopez On the -

Tales of a Fourth Grade Nothing Judy Blume
0 Tales of a Fourth Grade Nothing Judy Blume 1 For Larry, who is a combination of Peter and Fudge, and for Willie Mae, who told me about Dribble 2 Contents 1 The Big Winner 2 Mr. and Mrs. Juicy-O 3 The Family Dog 4 My Brother the Bird 5 The Birthday Bash 6 Fang Hits Town 7 The Flying Train Committee 8 The TV Star 9 Just Another Rainy Day 10 Dribble! 3 1 The Big Winner I won Dribble at Jimmy Fargo's birthday party. All the other guys got to take home goldfish in little plastic bags. I won him because I guessed there were three hundred and forty-eight jelly beans in Mrs. Fargo's jar. Really, there were four hundred and twenty-three, she told us later. Still, my guess was closest. "Peter Warren Hatcher is the big winner!" Mrs. Fargo announced. At first I felt bad that I didn't get a goldfish too. Then Jimmy handed me a glass bowl. Inside there was some water and three rocks. A tiny green turtle was sleeping on the biggest rock. All the other guys looked at their goldfish. I knew what they were thinking. They wished they could have tiny green turtles too. I named my turtle Dribble while I was walking home from Jimmy's party. I live at 25 West 68th Street. It's an old apartment building. But it's got one of the best elevators in New York City. There are mirrors all around. You can see yourself from every angle. -

De Turkey and De Law
Library of Congress De Turkey and de Law Title Page 7957 Oct. 29, 1930 I.C. DE TURKEY AND DE LAW A COMEDY IN THREE ACTS by ZORA HURSTON Cast CAST Jim Weston A young man and the town bully (A Methodist) Dave Carter The town's best hunter and fisherman (Baptist) Joe Clarke The Mayor, Postmaster, storekeeper Daisy Blunt The town vamp Lum Boger The Marshall Walter Thomas A villager (Methodist) Lige Moseley A villager (Methodist) De Turkey and de Law http://www.loc.gov/resource/mhurston.0102 Library of Congress Joe Lindsay A villager (Baptist) Della Lewis A villager (Baptist) Tod Hambo A villager (Baptist) Lucy Taylor A villager (Methodist) Rev. Singletary (Baptist) Rev. Simms (Methodist) Villagers, children, dogs. Act I ACT I SETTING: A Negro village in Florida in our own time. All action from viewpoint of an actor facing audience. PLACE: Joe Clarke's store porch in the village. A frame building with a false front. A low porch with two steps up. Door in center of porch. A window on each side of the door. A bench on each side of the porch. Axhandles, hoes and shovels, etc. are displayed leaning against the wall. Exits right and left. Street is unpaved. Grass and weeds growing all over. TIME: It is late afternoon on a Saturday in summer. Before the curtain rises the voices of children are heard, boisterous at play. Shouts and laughter. VOICE OF ONE BOY De Turkey and de Law http://www.loc.gov/resource/mhurston.0102 Library of Congress Naw, I don't want to play wringing no dish rag! We gointer play chick mah chick mah craney crow. -

FROM OUR OKLAHOMA CITY HEADQUARTERS: —The Joys of Airmarking — — Have You Had Your Apuepuelele? — — Help Give Hope Wings — America, You Look Better Than Ever
MARCH 1976 FROM OUR OKLAHOMA CITY HEADQUARTERS: —The Joys of Airmarking — — Have You Had Your Apuepuelele? — — Help Give Hope Wings — America, you look better than ever. Here’s an inspiring impression of the American Dream seen from a Beechcraft. President Pat’s Hi e SH i w i u s ACTion Line Have you taken your APT yet? I have — WOW! — was I rusty! Volume 3 Number 1 March 1976 That’s what happens when you fly a desk and don’t make it to the airport often enough. I really enjoyed it even though I was embarrassed to see how my proficiency had dropped. Remember — annual THE NINETY-NINES, INCORPORATED proficiency training is not a check ride — just a check-up to let you know you need to fly a little more often to keep ahead of the airplane. Congratulations are in order to all of you. Our ranks are swelling and International Headquarters Terminal Drive and Amelia Earhart Lane our membership is on the rise. Women pilots are not the exception any P.O. Box 59965 more, and more are learning to fly in spite of the fuel crisis claims. Let’s Will Rogers World Airport Oklahoma City, Oklahoma 73159 invite these women pilots to join us and become a part of our ACT. Return form 3579 to above address. And why don’t you all join me and ACT — GET APT — start the 2nd Class Postage paid at Oklahoma City, OK. Phone: (405)682-4425 year out right. No time like the present to call and set a time for your Annual Proficiency Training. -

SEQUOYA REVIEW UTC’S Annual Literary & Arts Magazine 2017
SEQUOYA REVIEW UTC’s Annual Literary & Arts Magazine 2017 Thanks to Sarah Einstein, this year's advisor ARTIST STATEMENT A Statement from the Cover Artist: Sarah Bowers “Travel is fatal to prejudice, bigotry, and narrow-mindedness, and many of our people need it sorely on these accounts. Broad, wholesome, charitable views of men and things cannot be acquired by vegetating in one little corner of the earth all one's lifetime.” -Mark Twain SEQUOYA REVIEW 3 FOREWORD Foreword To borrow from our own Olivette Petersen’s poem “Immortality,” I truly believe that in this journal you will find “a million memories . a thousand pictures . a piece of yourself” – one that you’re looking to share, and maybe some that you keep hidden. This journal is a stained-glass mosaic of stories true and imagined, and of artwork that speaks without words. These pages are inhabited by commonality, but also by an unfathomable number of totally unique experiences. They weave together in beautiful diversity. Making art is how we is how we explore what it means to live, and it’s how we live forever. Take a look. Tara McGlocklin Editor-in-Chief Sequoya Review 4 SEQUOYA REVIEW HISTORY Sequoya Review: A History It was a busy time in the United States in In 1975, this magazine was officially 1965: Martin Luther King Jr. marched renamed Sequoya Review, which would 25,000 people to the capital of Alabama; serve as the permanent title for at least the U.S. authorized its first ground the next forty years. It is doubtful that combat forces in Vietnam; Malcolm X the title will be changed in the future, was assassinated; The Who dropped their for it both honors an important Cherokee very first album; The Sound of Music was contributor to the publishing realm, and released in theaters; and the television because we have invested a fair amount of soap opera Days of Our Lives premiered.