Revisiting the Transverse Cervical Artery and Vein for Complex Head and Neck Reconstruction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch
411 Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch John Holder1 Five cases are reported of left subclavian steal syndrome associated with anomalous Eugene F. Binet2 origin of the left vertebral artery from the aortic arch. In all five instances blood flow at Bernard Thompson3 the origin of the left vertebral artery was in an antegrade direction contrary to that usually reported in this condition. The distal subclavian artery was supplied via an extensive collateral network of vessels connecting the vertebral artery to the thyro cervical trunk. If a significant stenosis or occlusion is present within the left subc lavi an artery proximal to the origin of the left vertebral artery, the direction of the bl ood fl ow within the vertebral artery will reverse toward the parent vessel (retrograde flow). This phenomenon occurs when a negative pressure gradient of 20-40 torr exists between the vertebral-basilar artery junction and th e vertebral-subc lavian artery junction [1-3]. We describe five cases of subclavian steal confirmed by angiography where a significant stenosis or occlusion of the left subclavian artery was demonstrated in association with anomalous origin of th e left vertebral artery directly from the aortic arch. In all five cases blood flow at the origin of the left vertebral artery was in an antegrade direction contrary to that more commonly reported in the subclavian steal syndrome. Materials and Methods The five patients were all 44- 58-year-old men. Three sought medical attention for symptoms specificall y related to th e left arm . -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

The Variations of the Subclavian Artery and Its Branches Ahmet H
Okajimas Folia Anat. Jpn., 76(5): 255-262, December, 1999 The Variations of the Subclavian Artery and Its Branches By Ahmet H. YUCEL, Emine KIZILKANAT and CengizO. OZDEMIR Department of Anatomy, Faculty of Medicine, Cukurova University, 01330 Balcali, Adana Turkey -Received for Publication, June 19,1999- Key Words: Subclavian artery, Vertebral artery, Arterial variation Summary: This study reports important variations in branches of the subclavian artery in a singular cadaver. The origin of the left vertebral artery was from the aortic arch. On the right side, no thyrocervical trunk was found. The two branches which normally originate from the thyrocervical trunk had a different origin. The transverse cervical artery arose directly from the subclavian artery and suprascapular artery originated from the internal thoracic artery. This variation provides a short route for posterior scapular anastomoses. An awareness of this rare variation is important because this area is used for diagnostic and surgical procedures. The subclavian artery, the main artery of the The variations of the subclavian artery and its upper extremity, also gives off the branches which branches have a great importance both in blood supply the neck region. The right subclavian arises vessels surgery and in angiographic investigations. from the brachiocephalic trunk, the left from the aortic arch. Because of this, the first part of the right and left subclavian arteries differs both in the Subjects origin and length. The branches of the subclavian artery are vertebral artery, internal thoracic artery, This work is based on a dissection carried out in thyrocervical trunk, costocervical trunk and dorsal the Department of Anatomy in the Faculty of scapular artery. -
The Vertebral Artery in the Vascular Lab: What Does It Mean?
The Vertebral Artery in the Vascular Lab: What Does It Mean? Caron Rockman MD Frances and Joseph Ritroto Professor of Surgery Program Director, Vascular Surgery New York University Langone Medical Center Disclosures •None Division of Vascular and Endovascular Surgery Subclavian Steal Occlusion of proximal Subclavian Art Vertebral artery supplies retrograde flow Posterior brain receives decreased flow 55 years + Men > Women more than 2:1 LSA affected 3x more than RSA Division of Vascular and Endovascular Surgery Subclavian Steal Causes: - Arteriosclerosis of subclavian artery (>95% cases) - Embolism - Takayasu’s Arteritis -Dissecting Aneurysm Risk Factors: (similar to CAD) -Smoking -Hypertension -Hyperlipidemia -Hypertension Division of Vascular and Endovascular Surgery Symptoms of Subclavian Steal Vertebrobasilar Insufficiency (posterior circulation symptoms) Light headedness or dizziness Ataxia or Vertigo Visual Disturbance Headache Syncope Confusion Division of Vascular and Endovascular Surgery Symptoms of Subclavian Steal Subclavian Insufficiency Arm weakness, coldness Numbness or “tingling” Arm Claudication with exercise Symptoms can be exacerbated with: Vigorous exercise Sudden turning of head to affected side Division of Vascular and Endovascular Surgery Signs of Subclavian Steal Diminished pulses (radial/ulnar) Discrepant blood pressures in upper extremities (>20mmHg) (Pitfall with bilateral disease) Subclavian Bruit 7 Division of Vascular and Endovascular Surgery Subclavian steal on Duplex Exam Incomplete steal •Striking deceleration of velocity in mid or late systole •High grade stenosis of subclavian rather than occlusion Complete Steal •Complete reversal of flow within the vertebral artery Division of Vascular and Endovascular Surgery Vertebral Retrograde Flow • Reversal of flow in the vertebral artery is a common finding identified on cerebrovascular duplex ultrasound. • The clinical significance and natural history of patients presenting with this finding, however, is poorly understood. -

Spontaneous Arteriovenous Malformations in the Cervical Area
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.33.3.303 on 1 June 1970. Downloaded from J. Neurol. Neurosurg. Psychiat., 1970, 33, 303-309 Spontaneous arteriovenous malformations in the cervical area J. GREENBERG, M.D. From the Department of Neurology, Episcopal Hospital, Philadelphia, Pennsylvania 19125, U.S.A. SUMMARY Four patients with spontaneous arteriovenous malformations of cervical vessels have been presented. The embryology of these vessels has been discussed in order to suggest an ex- planation for the apparent difference in the incidence of arteriovenous malformations involving the internal carotid artery and those involving either the vertebral or the external carotid arteries. A fifth case (S.T.) is presented as a probable iatrogenic arteriovenous fistula and is to be added to the steadily growing reports of this phenomenon. Trauma is the most common cause of arteriovenous had sustained a minor injury to the posterior aspect communications between the blood vessels in of the right ear. Routine skull films at the time did not the cervical area (Aronson, 1961). Iatrogenic reveal a fracture, and there was no evidence of local Protected by copyright. deep tissue injury noted. fistulae occurring after carotid or vertebral angio- On the present admission, a slight prominence of the graphy are being reported with regularity in the right retroauricular region was noted and a thrill and recent literature (Sutton, 1962). Spontaneous mal- bruit were present. The bruit could be obliterated by formations in this area also occur. Thus far, eight local pressure. cases have been reported involving the vertebral The neurological examination was within normal vessels (Norman, Schmidt, and Grow, 1950; limits. -

A Very Rare Origin of the Left Vertebral Artery and Its Clinical Implications
ARC Journal of Cardiology Volume 5, Issue 2, 2019, PP 14-18 ISSN No. (Online): 2455-5991 DOI: http://dx.doi.org/10.20431/2455-5991.0502003 www.arcjournals.org A Very Rare Origin of the Left Vertebral Artery and its Clinical Implications Olutayo Ariyo* Dept. of Anatomy Pathology and Cell Biology, SKMC at Thomas Jefferson University, Philadelphia, USA *Corresponding Author: Olutayo Ariyo, Dept. of Anatomy Pathology and Cell Biology, SKMC at Thomas Jefferson University, Philadelphia, USA, E-mail: [email protected] Abstract: Most variants of the left vertebral artery tend to occursupra-aortic, usually between the left common carotid and the left subclavian arteries. We report a rare variant of the left vertebral artery arising as the most distal and inferior branch off the aortic arch in a 69 year- old male cadaver. Arising postero- inferiorly from the arch, the variant coursed superiorly and medial -ward, posterior to the left subclavian artery, enteringthe transverse cervical foramina at C5 level to run more cranially cervical foramina C5-C2. The variant artery was an observed with some tortuosity just proximal to entry into C5 foramina. The normally arising left or right vertebral artery plays a vital role in the Subclavian Steal Syndrome, a retrograde flow in the ipsilateral vertebral artery in an occlusion proximal origin of its ipsilateral subclavian artery. In our reported variant, modelled with a possible occlusion in the proximal segment of the left subclavian artery, despite an hypothesized retrograde flow in the left vertebral artery will not be helpful in delivering blood into the subclavian-axillary continuum, as such retrograde flow will dump into the aortic arch directly and unhelpful to the occluded left subclavian artery. -
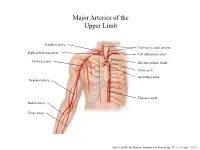
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

Ascending and Descending Thoracic Vertebral Arteries
CLINICAL REPORT EXTRACRANIAL VASCULAR Ascending and Descending Thoracic Vertebral Arteries X P. Gailloud, X L. Gregg, X M.S. Pearl, and X D. San Millan ABSTRACT SUMMARY: Thoracic vertebral arteries are anastomotic chains similar to cervical vertebral arteries but found at the thoracic level. Descending thoracic vertebral arteries originate from the pretransverse segment of the cervical vertebral artery and curve caudally to pass into the last transverse foramen or the first costotransverse space. Ascending thoracic vertebral arteries originate from the aorta, pass through at least 1 costotransverse space, and continue cranially as the cervical vertebral artery. This report describes the angiographic anatomy and clinical significance of 9 cases of descending and 2 cases of ascending thoracic vertebral arteries. Being located within the upper costotransverse spaces, ascending and descending thoracic vertebral arteries can have important implications during spine inter- ventional or surgical procedures. Because they frequently provide radiculomedullary or bronchial branches, they can also be involved in spinal cord ischemia, supply vascular malformations, or be an elusive source of hemoptysis. ABBREVIATIONS: ISA ϭ intersegmental artery; SIA ϭ supreme intercostal artery; VA ϭ vertebral artery he cervical portion of the vertebral artery (VA) is formed by a bral arteria lusoria8-13 or persistent left seventh cervical ISA of Tseries of anastomoses established between the first 6 cervical aortic origin.14 intersegmental arteries (ISAs) and one of the carotid-vertebral This report discusses 9 angiographic observations of descend- anastomoses, the proatlantal artery.1-3 The VA is labeled a “post- ing thoracic VAs and 2 cases of ascending thoracic VAs. costal” anastomotic chain (ie, located behind the costal process of cervical vertebrae or dorsal to the rib itself at the thoracic level) to CASE SERIES emphasize its location within the transverse foramina. -

The Rare Origin of the Suprascapular Artery Arising Off The
eISSN 1308-4038 International Journal of Anatomical Variations (2011) 4: 182–184 Case Report The rare origin of the suprascapular artery arising off the internal thoracic artery in the presence of the thyrocervical trunk: clinical and surgical implications Published online December 2nd, 2011 © http://www.ijav.org Stavros ATSAS ABSTRACT Jacob N. FOX During routine dissection of the subclavian artery and its branches, the suprascapular artery was found arising from H. Wayne LAMBERT the proximal end of the internal thoracic artery in only the left side of a 68-year-old Caucasian male, despite the presence of the thyrocervical trunk on the ipsilateral side. The suprascapular artery ran deep to the proximal one- third of the clavicle then continued its usual course, running parallel to the suprascapular nerve and passing over the superior transverse scapular ligament distally. Knowledge of this variant origin of the suprascapular artery is clinically Department of Neurobiology and Anatomy, West Virginia University School of Medicine, important because the internal thoracic artery is utilized for a majority of the 800,000 coronary artery bypass surgeries Robert C. Byrd Health Sciences Center, Morgantown, West Virginia, USA. performed worldwide each year. Its course deep to the clavicle is also significant due to clavicular fractures accounting for approximately 5-15% of adult bone fractures. © IJAV. 2011; 4: 182–184. Dr. H. Wayne Lambert, PhD Associate Professor West Virginia University School of Medicine Robert C. Byrd Health Sciences Center Department of Neurobiology and Anatomy HSN 4052; P.O. Box 9128 Morgantown, WV, 26506-9128, USA. +1 304 293-0610 [email protected] Key words [anatomical variant] [suprascapular artery] [internal thoracic artery] [branches of subclavian artery] [thyrocervical trunk] [coronary bypass Received June 21st, 2011; accepted October 12th, 2011 surgery] [radical and modified neck dissections] Introduction In 2005, Weiglein et al. -

An Unusual Origin and Course of the Thyroidea Ima Artery, with Absence of Inferior Thyroid Artery Bilaterally
Surgical and Radiologic Anatomy (2019) 41:235–237 https://doi.org/10.1007/s00276-018-2122-1 ANATOMIC VARIATIONS An unusual origin and course of the thyroidea ima artery, with absence of inferior thyroid artery bilaterally Doris George Yohannan1 · Rajeev Rajan1 · Akhil Bhuvanendran Chandran1 · Renuka Krishnapillai1 Received: 31 May 2018 / Accepted: 21 October 2018 / Published online: 25 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract We report an unusual origin and course of the thyroidea ima artery in a male cadaver. The ima artery originated from the right subclavian artery very close to origin of the right vertebral artery. The artery coursed anteriorly between the common carotid artery medially and internal jugular vein laterally. It then coursed obliquely, from below upwards, from lateral to medial superficial to common carotid artery, to reach the inferior pole of the right lobe of thyroid and branched repeatedly to supply the anteroinferior and posteroinferior aspects of both the thyroid lobes and isthmus. The superior thyroid arteries were normal. Both the inferior thyroid arteries were absent. The unusual feature of this thyroidea ima artery is its origin from the subclavian artery close to vertebral artery origin, the location being remarkably far-off from the usual near midline position, and the oblique and relatively superficial course. This report is a caveat to neck surgeons to consider such a superficially running vessel to be a thyroidea ima artery. Keywords Thyroid vascular anatomy · Thyroidea ima artery · Artery of Neubauer · Blood supply of thyroid · Variations Introduction (1.1%), transverse scapular (1.1%), or pericardiophrenic or thyrocervical trunk [8, 10]. -

SAY: Welcome to Module 1: Anatomy & Physiology of the Brain. This
12/19/2018 11:00 AM FOUNDATIONAL LEARNING SYSTEM 092892-181219 © Johnson & Johnson Servicesv Inc. 2018 All rights reserved. 1 SAY: Welcome to Module 1: Anatomy & Physiology of the Brain. This module will strengthen your understanding of basic neuroanatomy, neurovasculature, and functional roles of specific brain regions. 1 12/19/2018 11:00 AM Lesson 1: Introduction to the Brain The brain is a dense organ with various functional units. Understanding the anatomy of the brain can be aided by looking at it from different organizational layers. In this lesson, we’ll discuss the principle brain regions, layers of the brain, and lobes of the brain, as well as common terms used to orient neuroanatomical discussions. 2 SAY: The brain is a dense organ with various functional units. Understanding the anatomy of the brain can be aided by looking at it from different organizational layers. (Purves 2012/p717/para1) In this lesson, we’ll explore these organizational layers by discussing the principle brain regions, layers of the brain, and lobes of the brain. We’ll also discuss the terms used by scientists and healthcare providers to orient neuroanatomical discussions. 2 12/19/2018 11:00 AM Lesson 1: Learning Objectives • Define terms used to specify neuroanatomical locations • Recall the 4 principle regions of the brain • Identify the 3 layers of the brain and their relative location • Match each of the 4 lobes of the brain with their respective functions 3 SAY: Please take a moment to review the learning objectives for this lesson. 3 12/19/2018 11:00 AM Directional Terms Used in Anatomy 4 SAY: Specific directional terms are used when specifying the location of a structure or area of the brain. -

The 0Ccipital-Vertebral Anastomosis
The 0ccipital-Vertebral Anastomosis MANNIE M. SCHECIITER,M.D. Section of Neuroradiology, Department of Radiology, Albert Einstein College of Medicine, New York, New York HE presence and significance of collat- artery. In the past this was, in fact, the basis eral circulation between the various for techniques of indirect vertebral angiog- T branches of the intracranial circulation raphy in which the right carotid artery was and branches of the intracranial and extra- compressed distal to the site of the puncture cranial circulation have been described in the during angiography.4,5 Similarly retrograde literature. With the current interest and em- carotid catheterization may also be used to phasis in the medical and surgical treatment demonstrate the vertebral artery and its of cerebrovascular disease and with improve- branches).1~ ments in diagnostic procedures, a clearer When filling of the vertebral artery occurs demonstration of these collateral channels is during the injection of contrast medium into now more frequently sought and recognized. the carotid artery or vice versa, the occipital- Most of these potential collateral channels vertebral anastomosis may be demonstrated become obvious only when occlusive vascular by including the cervical course of the verte- disease interrupts the normal pathways, and bral artery in the film. Absence of contrast the channels dilate to form alternate routes medium in the proximal portion of the com- for the passage of blood to vital areas. A mon carotid artery and vertebral artery will temporary differential in the hydrodynamics be recognized readily, excluding this as the of two opposing systems may also reverse the possible course of flow (Figs.