MLN Connects for Thursday, February 27, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Date Genesis to Revelation Friday, January 01, 2021 Genesis 1-3
Date Genesis to Revelation Friday, January 01, 2021 Genesis 1-3 Saturday, January 02, 2021 Genesis 4-7 Sunday, January 03, 2021 Genesis 8-11 Monday, January 04, 2021 Genesis 12-15 Tuesday, January 05, 2021 Genesis 16-18 Wednesday, January 06, 2021 Genesis 19-21 Thursday, January 07, 2021 Genesis 22-24 Friday, January 08, 2021 Genesis 25-26 Saturday, January 09, 2021 Genesis 27-29 Sunday, January 10, 2021 Genesis 30-31 Monday, January 11, 2021 Genesis 32-34 Tuesday, January 12, 2021 Genesis 35-37 Wednesday, January 13, 2021 Genesis 38-40 Thursday, January 14, 2021 Genesis 41-42 Friday, January 15, 2021 Genesis 43-45 Saturday, January 16, 2021 Genesis 46-47 Sunday, January 17, 2021 Genesis 48-50 Monday, January 18, 2021 Exodus 1-3 Tuesday, January 19, 2021 Exodus 4-6 Wednesday, January 20, 2021 Exodus 7-9 Thursday, January 21, 2021 Exodus 10-12 Friday, January 22, 2021 Exodus 13-15 Saturday, January 23, 2021 Exodus 16-18 Sunday, January 24, 2021 Exodus 19-21 Monday, January 25, 2021 Exodus 22-24 Tuesday, January 26, 2021 Exodus 25-27 Wednesday, January 27, 2021 Exodus 28-29 Thursday, January 28, 2021 Exodus 30-32 Friday, January 29, 2021 Exodus 33-35 Saturday, January 30, 2021 Exodus 36-38 Sunday, January 31, 2021 Exodus 39-40 Monday, February 01, 2021 Leviticus 1-4 Tuesday, February 02, 2021 Leviticus 5-7 Wednesday, February 03, 2021 Leviticus 8-10 Thursday, February 04, 2021 Leviticus 11-13 Friday, February 05, 2021 Leviticus 14-15 Saturday, February 06, 2021 Leviticus 16-18 Sunday, February 07, 2021 Leviticus 19-21 Monday, February 08, -

Minutes 2/27/2021
Minutes of the New Marlborough Historical Commission held on February 27, 2021. Conference Call Meeting. Meeting was called to order at 8:3AM by Dr. John Schreiber, other members on the call: Ms. Deanna Mummert, Mrs. Claudette Callahan, Mrs. Fiona Kerr, Mr. Joe Poindexter, chair of the Historical Society, & Ms. Tara White. Meeting minutes of November 14, 2020 were accepted as amended. Southfield Historic District Update: Mrs. Callahan mentioned that she submitted the report in December, 2020, and was waiting to hear form her contact person whom she had been working with. Mrs. Callahan stated that she finally heard from the Director of the State Historical Commission, and the Director recommended to Mrs. Callahan different directions on how to proceed which included the hiring of a consultant. Mrs. Callahan said she’ll continue to work on the update, and suggested a consultant be hired to review the report she has completed. Mrs. Callahan also mentioned that the report has to go to State Historical Commission first and be accepted then the report will be submitted to the National Historical Commission. Dr. Schreiber mentioned that he has already submitted the budget for FY22, but he agrees that hiring a consultant would be helpful. After a brief discussion Ms. Mummert made a motion to amend the FY22 budget in the amount of $500.00 to hire a consultant, motion was seconded by Mrs. Kerr, motion passed unanimously. Demolition Delay Bylaw Review of Planning Board Comments: Dr. Schreiber mentioned that the commission members should consider what bylaw that they would like to work on and get approved. -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -
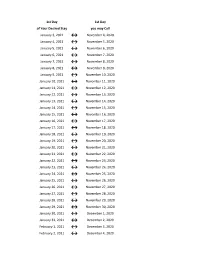
Flex Dates.Xlsx
1st Day 1st Day of Your Desired Stay you may Call January 3, 2021 ↔ November 4, 2020 January 4, 2021 ↔ November 5, 2020 January 5, 2021 ↔ November 6, 2020 January 6, 2021 ↔ November 7, 2020 January 7, 2021 ↔ November 8, 2020 January 8, 2021 ↔ November 9, 2020 January 9, 2021 ↔ November 10, 2020 January 10, 2021 ↔ November 11, 2020 January 11, 2021 ↔ November 12, 2020 January 12, 2021 ↔ November 13, 2020 January 13, 2021 ↔ November 14, 2020 January 14, 2021 ↔ November 15, 2020 January 15, 2021 ↔ November 16, 2020 January 16, 2021 ↔ November 17, 2020 January 17, 2021 ↔ November 18, 2020 January 18, 2021 ↔ November 19, 2020 January 19, 2021 ↔ November 20, 2020 January 20, 2021 ↔ November 21, 2020 January 21, 2021 ↔ November 22, 2020 January 22, 2021 ↔ November 23, 2020 January 23, 2021 ↔ November 24, 2020 January 24, 2021 ↔ November 25, 2020 January 25, 2021 ↔ November 26, 2020 January 26, 2021 ↔ November 27, 2020 January 27, 2021 ↔ November 28, 2020 January 28, 2021 ↔ November 29, 2020 January 29, 2021 ↔ November 30, 2020 January 30, 2021 ↔ December 1, 2020 January 31, 2021 ↔ December 2, 2020 February 1, 2021 ↔ December 3, 2020 February 2, 2021 ↔ December 4, 2020 1st Day 1st Day of Your Desired Stay you may Call February 3, 2021 ↔ December 5, 2020 February 4, 2021 ↔ December 6, 2020 February 5, 2021 ↔ December 7, 2020 February 6, 2021 ↔ December 8, 2020 February 7, 2021 ↔ December 9, 2020 February 8, 2021 ↔ December 10, 2020 February 9, 2021 ↔ December 11, 2020 February 10, 2021 ↔ December 12, 2020 February 11, 2021 ↔ December 13, 2020 -

Policy Subcommittee Cameron Middle School - Library 215 Elm St, Framingham February 27, 2020 Open Meeting Minutes
Policy Subcommittee Cameron Middle School - Library 215 Elm St, Framingham February 27, 2020 Open Meeting Minutes PRESENT: Tiffanie Maskell (Chair), Jessica Barnhill, Beverly Hugo, Geoff Epstein ABSENT: None OTHERS PRESENT: Superintendent Dr. Tremblay, Executive Assistant to the Superintendent Amy Kane, Executive Assistant to the School Committee Joanna Hastry ____________________________________________________ Call to Order The Chair called the meeting to order at 4:35 p.m. Public Comment No public comment. Discussion/Vote of Open Policies From Last Term Ms. Maskell suggested that the policies that were referred from the Racial Equity Subcommittee be tabled until after the equity audit to be looked at. There was discussion about having the reason why policies are being referred be required, as some of the still open policy referrals did not, and what process should be in future. Dr. Tremblay said he would like to vet policy change suggestions through all lenses; contractual, students, staff, etc, prior to bringing them to the Policy Subcommittee. Agreement to move the top priority policies to the top of the working policy spreadsheet, and to create a folder for each policy being discussed, as well as have a document on why it has been referred. Dr. Tremblay to share a list of what they think the policies they are prioritizing internally. No action taken on the outstanding policies. Discussion/Vote on MASC Full Policy Review Dr. Tremblay would like to make one of his goals for next year to review all of Framingham Public School’s policies with MASC. Motion: To agree that the MASC full policy review will be beneficial to the school district and committee, and to support adding the MASC full policy review for $10,500 to the School Committee budget. -

Pay Date Calendar
Pay Date Information Select the pay period start date that coincides with your first day of employment. Pay Period Pay Period Begins (Sunday) Pay Period Ends (Saturday) Official Pay Date (Thursday)* 1 January 10, 2016 January 23, 2016 February 4, 2016 2 January 24, 2016 February 6, 2016 February 18, 2016 3 February 7, 2016 February 20, 2016 March 3, 2016 4 February 21, 2016 March 5, 2016 March 17, 2016 5 March 6, 2016 March 19, 2016 March 31, 2016 6 March 20, 2016 April 2, 2016 April 14, 2016 7 April 3, 2016 April 16, 2016 April 28, 2016 8 April 17, 2016 April 30, 2016 May 12, 2016 9 May 1, 2016 May 14, 2016 May 26, 2016 10 May 15, 2016 May 28, 2016 June 9, 2016 11 May 29, 2016 June 11, 2016 June 23, 2016 12 June 12, 2016 June 25, 2016 July 7, 2016 13 June 26, 2016 July 9, 2016 July 21, 2016 14 July 10, 2016 July 23, 2016 August 4, 2016 15 July 24, 2016 August 6, 2016 August 18, 2016 16 August 7, 2016 August 20, 2016 September 1, 2016 17 August 21, 2016 September 3, 2016 September 15, 2016 18 September 4, 2016 September 17, 2016 September 29, 2016 19 September 18, 2016 October 1, 2016 October 13, 2016 20 October 2, 2016 October 15, 2016 October 27, 2016 21 October 16, 2016 October 29, 2016 November 10, 2016 22 October 30, 2016 November 12, 2016 November 24, 2016 23 November 13, 2016 November 26, 2016 December 8, 2016 24 November 27, 2016 December 10, 2016 December 22, 2016 25 December 11, 2016 December 24, 2016 January 5, 2017 26 December 25, 2016 January 7, 2017 January 19, 2017 1 January 8, 2017 January 21, 2017 February 2, 2017 2 January -

Due Date Chart 201803281304173331.Xlsx
Special Event Permit Application Due Date Chart for Events from January 1, 2019 - June 30, 2020 If due date lands on a Saturday or Sunday, the due date is moved to the next business day Event Date 30 Calendar days 90 Calendar Days Tuesday, January 01, 2019 Sunday, December 02, 2018 Wednesday, October 03, 2018 Wednesday, January 02, 2019 Monday, December 03, 2018 Thursday, October 04, 2018 Thursday, January 03, 2019 Tuesday, December 04, 2018 Friday, October 05, 2018 Friday, January 04, 2019 Wednesday, December 05, 2018 Saturday, October 06, 2018 Saturday, January 05, 2019 Thursday, December 06, 2018 Sunday, October 07, 2018 Sunday, January 06, 2019 Friday, December 07, 2018 Monday, October 08, 2018 Monday, January 07, 2019 Saturday, December 08, 2018 Tuesday, October 09, 2018 Tuesday, January 08, 2019 Sunday, December 09, 2018 Wednesday, October 10, 2018 Wednesday, January 09, 2019 Monday, December 10, 2018 Thursday, October 11, 2018 Thursday, January 10, 2019 Tuesday, December 11, 2018 Friday, October 12, 2018 Friday, January 11, 2019 Wednesday, December 12, 2018 Saturday, October 13, 2018 Saturday, January 12, 2019 Thursday, December 13, 2018 Sunday, October 14, 2018 Sunday, January 13, 2019 Friday, December 14, 2018 Monday, October 15, 2018 Monday, January 14, 2019 Saturday, December 15, 2018 Tuesday, October 16, 2018 2019 Tuesday, January 15, 2019 Sunday, December 16, 2018 Wednesday, October 17, 2018 Wednesday, January 16, 2019 Monday, December 17, 2018 Thursday, October 18, 2018 Thursday, January 17, 2019 Tuesday, December 18, 2018 -

COVID-19 in Ontario: Focus on March 21, 2021 to March 27, 2021
Weekly Epidemiologic Summary COVID-19 in Ontario: Focus on March 21, 2021 to March 27, 2021 This report includes the most current information available from CCM as of March 30, 2021. Please visit the interactive Ontario COVID-19 Data Tool to explore recent COVID-19 data by public health unit, age group, sex, and trends over time. A daily summary is available and provides an epidemiologic summary of recent COVID-19 activity in Ontario. This weekly report provides an epidemiologic summary of COVID-19 activity in Ontario over time. Highlights There are a total of 344,436 confirmed cases of COVID-19 in Ontario with a public health unit reported date up to March 27, 2021. For the period with a public health unit reported date between March 21 to 27, 2021 (week 12): A total of 14,360 cases were reported to public health compared to 11,014 cases the previous week (March 14 to 20, 2021). There is a 30.4% increase in reported cases in Ontario this week (n=14,360) compared to the previous week (n=11,014). The last time the week-to-week percentage increase was this large was the week of December 29th, 2020. In week 12, the most ethnically diverse neighbourhoods in Ontario had COVID-19 rates that were 3.8 times higher than the least diverse neighbourhoods. This is the largest rate ratio reported since week 8 (February 21 to 27, 2021). The term public health unit reported date in this document refers to the date local public health units were first notified of the case. -

Date of Close Contact Exposure
Date of Close Contact Exposure 7 days 10 days 14 days Monday, November 16, 2020 Tuesday, November 24, 2020 Friday, November 27, 2020 Tuesday, December 1, 2020 Tuesday, November 17, 2020 Wednesday, November 25, 2020 Saturday, November 28, 2020 Wednesday, December 2, 2020 Wednesday, November 18, 2020 Thursday, November 26, 2020 Sunday, November 29, 2020 Thursday, December 3, 2020 Thursday, November 19, 2020 Friday, November 27, 2020 Monday, November 30, 2020 Friday, December 4, 2020 Friday, November 20, 2020 Saturday, November 28, 2020 Tuesday, December 1, 2020 Saturday, December 5, 2020 Saturday, November 21, 2020 Sunday, November 29, 2020 Wednesday, December 2, 2020 Sunday, December 6, 2020 Sunday, November 22, 2020 Monday, November 30, 2020 Thursday, December 3, 2020 Monday, December 7, 2020 Monday, November 23, 2020 Tuesday, December 1, 2020 Friday, December 4, 2020 Tuesday, December 8, 2020 Tuesday, November 24, 2020 Wednesday, December 2, 2020 Saturday, December 5, 2020 Wednesday, December 9, 2020 Wednesday, November 25, 2020 Thursday, December 3, 2020 Sunday, December 6, 2020 Thursday, December 10, 2020 Thursday, November 26, 2020 Friday, December 4, 2020 Monday, December 7, 2020 Friday, December 11, 2020 Friday, November 27, 2020 Saturday, December 5, 2020 Tuesday, December 8, 2020 Saturday, December 12, 2020 Saturday, November 28, 2020 Sunday, December 6, 2020 Wednesday, December 9, 2020 Sunday, December 13, 2020 Sunday, November 29, 2020 Monday, December 7, 2020 Thursday, December 10, 2020 Monday, December 14, 2020 Monday, November -

ALG Minutes, February 27, 7:30 AM EOC Facility, 371 Main Street
ALG Minutes, February 27, 7:30 AM EOC facility, 371 Main Street Present: Bart Wendell, facilitator; Joan Gardner and Jon Benson, BoS; Christi Andersen and Roland Bourdon, FC; Diane Baume, SC; John Mangiaratti, Steve Barrett and Marie Altieri, staff. Absent: Amy Krishnamurthy, SC; Peter Light, staff. Audience: Mark Hald, Asst. Town Manager; Brian Mc Mullen, Asst. Assessor & Finance Director; Dave Verdolino, ABRSD finance director; and Charlie Kadlec. Additional information/documents: Agenda; Feb. 5th ALG Minutes; Town of Acton Multi-year financial model and Schedule of meetings and events for 2020 ATM and election. I. Regular Business 1. Minutes were accepted with corrections on the statement about full-day kindergarten. II. New/Special Business 2. FY20 Update John: not much has changed. We still have 40% of the snow and ice budget so we may be OK. The state gave us $100K for surplus CPC funds which have been incorporated into this year’s programs. We are working hard to get a 2% turn-back. Early voting seems to be going well, so far about 800 people have voted early. Marie: FY20 school budget has a revenue surplus of about $300-$400K. We have some big unanticipated expenses for SPED in the range of $600K. We have the circuit breaker as a back-up but it’s something we are watching closely. For bonding, we are also going out for the $7.5M in capital. The rating call is on Tuesday 03/03 and we expect a rate around 2% or a little higher. The school committee will vote on Thursday to accept the rate. -

2021 Working Day Calendar-5 Day-Alternative Format
2021 Working Days Calendar – 5 day The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 Non-working Day Saturday, January 2, 2021 Non-working Day Sunday, January 3, 2021 Non-working Day Monday, January 4, 2021 938 Tuesday, January 5, 2021 939 Wednesday, January 6, 2021 940 Thursday, January 7, 2021 941 Friday, January 8, 2021 942 Saturday, January 9, 2021 Non-working Day Sunday, January 10, 2021 Non-working Day Monday, January 11, 2021 943 Tuesday, January 12, 2021 944 Wednesday, January 13, 2021 945 Thursday, January 14, 2021 946 Friday, January 15, 2021 947 Saturday, January 16, 2021 Non-working Day Sunday, January 17, 2021 Non-working Day Monday, January 18, 2021 Non-working Day Tuesday, January 19, 2021 948 Wednesday, January 20, 2021 949 Thursday, January 21, 2021 950 Friday, January 22, 2021 951 Saturday, January 23, 2021 Non-working Day Sunday, January 24, 2021 Non-working Day Monday, January 25, 2021 952 Tuesday, January 26, 2021 953 Wednesday, January 27, 2021 954 Thursday, January 28, 2021 955 Friday, January 29, 2021 956 Saturday, January 30, 2021 Non-working Day Sunday, January 31, 2021 Non-working Day Monday, February 1, 2021 957 Tuesday, February 2, 2021 958 Wednesday, February 3, -

Date of Pascha (New Calendar)
Date of Pascha (New Calendar) Pub&Pharisee Meatfare Cheesefare First Day of Lent Pascha Ascenion Pentecost 2007 January 28, 2007 February 11, 2007 February 18, 2007 February 19, 2007 April 8, 2007 May 17, 2007 May 27, 2007 2008 January 13, 2008 January 27, 2008 February 3, 2008 February 4, 2008 March 23, 2008 May 1, 2008 May 11, 2008 2009 February 1, 2009 February 15, 2009 February 22, 2009 February 23, 2009 April 12, 2009 May 21, 2009 May 31, 2009 2010 January 24, 2010 February 7, 2010 February 14, 2010 February 15, 2010 April 4, 2010 May 13, 2010 May 23, 2010 2011 February 13, 2011 February 27, 2011 March 6, 2011 March 7, 2011 April 24, 2011 June 2, 2011 June 12, 2011 2012 January 29, 2012 February 12, 2012 February 19, 2012 February 20, 2012 April 8, 2012 May 17, 2012 May 27, 2012 2013 January 20, 2013 February 3, 2013 February 10, 2013 February 11, 2013 March 31, 2013 May 9, 2013 May 19, 2013 2014 February 9, 2014 February 23, 2014 March 2, 2014 March 3, 2014 April 20, 2014 May 29, 2014 June 8, 2014 2015 January 25, 2015 February 8, 2015 February 15, 2015 February 16, 2015 April 5, 2015 May 14, 2015 May 24, 2015 2016 January 17, 2016 January 31, 2016 February 7, 2016 February 8, 2016 March 27, 2016 May 5, 2016 May 15, 2016 2017 February 5, 2017 February 19, 2017 February 26, 2017 February 27, 2017 April 16, 2017 May 25, 2017 June 4, 2017 2018 January 21, 2018 February 4, 2018 February 11, 2018 February 12, 2018 April 1, 2018 May 10, 2018 May 20, 2018 2019 February 10, 2019 February 24, 2019 March 3, 2019 March 4, 2019 April 21, 2019