Chapter 1. Urinalysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(UPCR) Levels in Diabetic Nephropathy Patients
Journal of Personalized Medicine Article Gender Differences in Genetic Associations of RAB38 with Urinary Protein-to-Creatinine Ratio (UPCR) Levels in Diabetic Nephropathy Patients 1, 2,3,4, 1 1 Zhi-Lei Yu y, Chung-Shun Wong y , Yi Ting Lai , Wan-Hsuan Chou , Imaniar Noor Faridah 1,5, Chih-Chin Kao 6,7 , Yuh-Feng Lin 2,7,8,* and Wei-Chiao Chang 1,9,10,11,* 1 Department of Clinical Pharmacy, School of Pharmacy, Taipei Medical University, Taipei 110301, Taiwan; [email protected] (Z.-L.Y.); [email protected] (Y.T.L.); [email protected] (W.-H.C.); [email protected] (I.N.F.) 2 Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei 110301, Taiwan; [email protected] 3 Department of Emergency Medicine, Taipei Medical University-Shuang Ho Hospital, New Taipei City 235041, Taiwan 4 Department of Emergency Medicine, School of Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan 5 Faculty of Pharmacy, Ahmad Dahlan University, Yogyakarta 55164, Indonesia 6 Division of Nephrology, Department of Internal Medicine, Taipei Medical University Hospital, Taipei 110301, Taiwan; [email protected] 7 Division of Nephrology, Department of Internal Medicine, School of Medicine, College of Medicine, Taipei Medical University, Taipei 110301, Taiwan 8 Division of Nephrology, Department of Internal Medicine, Shuang Ho Hospital, Taipei Medical University, New Taipei City 235041, Taiwan 9 Master Program for Clinical Pharmacogenomics and Pharmacoproteomics, School of Pharmacy, Taipei Medical University, Taipei 110301, Taiwan 10 Integrative Research Center for Critical Care, Wan Fang Hospital, Taipei Medical University, Taipei 110301, Taiwan 11 Department of Medical Research, Shuang Ho Hospital, Taipei Medical University, New Taipei City 235041, Taiwan * Correspondence: [email protected] (Y.-F.L.); [email protected] (W.-C.C.) Z.-L.Y. -

The Treatment of Chyluria Secondary to Advanced Carcinoma of the Prostate
Prostate Cancer and Prostatic Diseases (2008) 11, 102–105 & 2008 Nature Publishing Group All rights reserved 1365-7852/08 $30.00 www.nature.com/pcan CASE REPORT The treatment of chyluria secondary to advanced carcinoma of the prostate SA Cluskey, A Myatt and MA Ferro Department of Urology, Huddersfield Royal Infirmary, Huddersfield, UK Chyluria has not been previously reported as being associated with carcinoma of the prostate. The most common cause is lymphatic filariasis, a parasitic disease. Non-parasitic chyluria is rare. We describe a case of chyluria associated with carcinoma of the prostate. We describe our successful management in this case and highlight how urologists may overcome problematic chyluria in patients with advanced carcinoma of the prostate. Prostate Cancer and Prostatic Diseases (2008) 11, 102–105; doi:10.1038/sj.pcan.4500994; published online 31 July 2007 Keywords: chyluria; androgen blockade; TURP Introduction 3-week history of back pain. He had not opened his bowels for 3 days but reported passage of flatus. He Chyluria occurs as a result of abnormal communication was referred to the acute surgical team for further in- between lymphatics and the urinary tract. It may be vestigation. associated with flank pain, fever, dysuria, haematuria At the time of admission, his symptoms included and chylous clot retention.1–3 Worldwide, the most general malaise, back pain and poor mobility. He was common cause is lymphatic filariasis, a mosquito-borne indeed bed bound. He reported no difficulty in passing parasitic disease endemic to tropical and subtropical urine, although he had been treated for a suspected areas. -
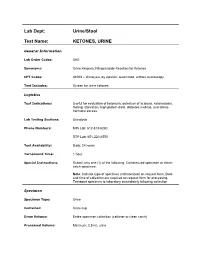
Ketones, Urine
Lab Dept: Urine/Stool Test Name: KETONES, URINE General Information Lab Order Codes: UKE Synonyms: Urine Ketones; Nitroprusside Reaction for Ketones CPT Codes: 81003 – Urinalysis, by dipstick; automated, without microscopy Test Includes: Screen for urine ketones. Logistics Test Indications: Useful for evaluation of ketonuria, detection of acidosis, ketoacidosis, fasting, starvation, high protein diets, diabetes mellitus, and stress- hormone excess. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 hour Special Instructions: Submit only one (1) of the following: Catheterized specimen or clean- catch specimen. Note: Indicate type of specimen (catheterized) on request form. Date and time of collection are required on request form for processing. Transport specimen to laboratory immediately following collection Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire specimen collection (catheter or clean catch) Processed Volume: Minimum: 0.5 mL urine Collection: A specimen collected by catheterization is optimal; however, a clean- catch or mid-stream specimen is also acceptable. Random, voided specimens will be accepted, but are the least desirable and are not recommended if a urine culture is also being requested. Special Processing: N/A Patient Preparation: None Sample Rejection: Less than 0.5 mL urine submitted; mislabeled or unlabeled specimen Interpretive Reference Range: Negative Critical Values: N/A Limitations: Specimens containing -

Chyluria in Pregnancy-A Decade of Experience in a Single Tertiary Care Hospital
Nephro Urol Mon. 2015 March; 7(2): e26309. DOI: 10.5812/numonthly.26309 Research Article Published online 2015 March 1. Chyluria in Pregnancy-A Decade of Experience in a Single Tertiary Care Hospital 1 1,* 1 1 2 Khalid Mahmood ; Ahsan Ahmad ; Kaushal Kumar ; Mahendra Singh ; Sangeeta Pankaj ; 2 Kalpana Singh 1Department of Urology, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India 2Department of Gynaecology, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India *Corresponding author : Ahsan Ahmad, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India. Tel: +91-9431457764, E-mail: [email protected] Received: ; Revised: ; Accepted: December 29, 2014 January 4, 2015 January 22, 2015 Background: Chyluria i.e. passage of chyle in urine, giving it milky appearance, is common in many parts of India but rare in west. Very few case of chyluria in pregnant female has been reported in literature. Persistence of this condition may have deleterious effects on health of child and mother. In the present study 43 cases of chyluria during pregnancy and their management seen over a period more than 10 years have been presented. Objectives: The study aims to present our experience of managing 43 cases with chyluria during pregnancy over a period of ten years from July 2003 to June 2014. Patients and Methods: Forty three pregnant patients with chyluria, who presented between July 2003 to June 2014 to the department of Urology, Indira Gandhi Institute of Medical Sciences, Patna were included. Patients underwent conservative management and/or sclerotherapy after evaluation. Follow-up of all patients was done by observation of urine color, routine examination of urine and test for post prandial chyle in urine up to 3 months after delivery. -
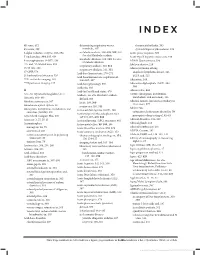
Basic Skills in Interpreting Laboratory Data
INDEX 4K score, 612 determining respiratory versus rheumatoid arthritis, 505 4Ts score, 399 metabolic, 307 systemic lupus erythematosus, 509 5-alpha reductase enzyme, 593–594 metabolic acidosis, 308–309, 309, 310. Acute phase response, 500 See also Metabolic acidosis 5' nucleotidase, 334, 335, 636 Acute type B hepatitis (minicase), 349 metabolic alkalosis, 309, 310. See also 6-mercaptopurine (6-MP), 138 ADAM Questionnaire, 596 Metabolic alkalosis 13C- and 14C-labeled urea, 353 Addison disease, 219 respiratory acidosis, 310, 311 15/15 rule, 208 Adenocarcinoma of lung respiratory alkalosis, 311, 311 17-OHP, 578 anaplastic lymphoma kinase, 526 Acid-base homeostasis, 270–271 21-hydroxylase deficiency, 526 EGFR and, 525 Acid-base homeostasis, regulation of, 99m Tc-sestamibi imaging, 165 306–307, 307 Adenosine, 164 201 TI perfusion imaging, 165 Acid-base physiology, 306 Adenosine diphosphate (ADP), 394, Acidemia, 303 394 A Acid-fast bacilli and stains, 470 Adenoviridae, 456 A1c. See Glycated hemoglobin (A1c) Acidosis. See also Metabolic acidosis ADME (absorption, distribution, metabolism, and excretion), 136 Abacavir, 468–469 defined, 303 Adnexal tumors, hirsutism secondary to Absolute neutropenia, 387 lactic, 308, 309 (minicase), 577 Absorbance optical system, 28 respiratory, 310, 311 Adolescents Absorption, distribution, metabolism, and Activated clotting time (ACT), 408 excretion (ADME), 136 categories of substances abused by, 70 Activated partial thromboplastin time prerequisite drug testing of, 82–83 Accu Check Compact Plus, 200 (aPTT), -

Diagnostic Accuracy of Spot Urine Protein-To-Creatinine Ratio For
O RIGINAL ARTICLE Diagnostic accuracy of spot urine protein-to- creatinine ratio for proteinuria and its association with adverse pregnancy outcomes in Chinese pregnant patients with pre-eclampsia HC Cheung *, KY Leung, CH Choi ABSTRACT diagnosing proteinuria in Chinese pregnant patients (33 mg/mmol) was similar to that stated in the International guidelines have Introduction: international literature (30 mg/mmol). A cut-off of endorsed spot urine protein-to-creatinine ratio of 20 mg/mmol provided a 100% sensitivity, and 52 >30 mg protein/mmol creatinine as an alternative mg/mmol provided a 100% specificity. There was to a 24-hour urine sample to represent significant no significant difference in spot urine protein-to- proteinuria. This study aimed to determine the creatinine ratio between cases with and without accuracy of spot urine protein-to-creatinine ratio adverse pregnancy outcome. in predicting significant proteinuria and adverse pregnancy outcome. Conclusions: Spot urine protein-to-creatinine ratio had a positive and significant correlation with 24-hour This case series was conducted in a Methods: urine results in Chinese pre-eclamptic women when regional obstetric unit in Hong Kong. A total of the ratio was <200 mg/mmol. Nonetheless, this ratio 120 Chinese pregnant patients with pre-eclampsia was not predictive of adverse pregnancy outcome. delivered at Queen Elizabeth Hospital from January 2011 to December 2013 were included. Relationship of spot urine protein-to-creatinine ratio and 24-hour Hong Kong Med J 2016;22:249–55 proteinuria; accuracy of the ratio against 24-hour DOI: 10.12809/hkmj154659 urine protein at different cut-offs; and relationship 1 HC Cheung *, MB, BS, MRCOG of such ratio and adverse pregnancy outcome were 1 KY Leung, FRCOG, FHKAM (Obstetrics and Gynaecology) studied. -

Bilirubin (Urine) Interpretive Summary
Bilirubin (Urine) Interpretive Summary Description: Bilirubinuria is an indicator of conjugated bilirubin in the urine. Excessive bilirubinuria in a dog or any bilirubinuria in a cat is an indication to evaluate serum bilirubin concentrations. Decreased Bilirubin Common Causes Normal Artifact o Exposure to UV light or room air o Delayed analysis o Centrifugation of urine prior to analysis o Ascorbic acid (Vitamin C) Increased Bilirubin Common Causes Normal dogs (especially males with concentrated urine) Liver disease, bile duct obstruction RBC destruction (hemolysis) o Immune-mediated hemolytic anemia o Zinc or onion toxicity o RBC parasites Uncommon Causes Hemoglobinuria Fever Prolonged anorexia False positive reactions due to medications o Phenothiazines (e.g., chlorpromazine) o Etodolac Related Findings Liver disease, biliary obstruction o Increased serum bilirubin, ALT, ALP, GGT, AST o Increased serum bile acids o Decreased albumin, cholesterol, BUN and glucose in severe cases o Abnormalities in liver and/or biliary tract on abdominal ultrasound RBC destruction o Decreased hematocrit, RBC, hemoglobin o Increased reticulocytes, increased MCV and decreased MCHC, polychromasia o Increased serum bilirubin o Spherocytosis (in dogs), autoagglutination o Hemoglobinuria o Positive Coombs or saline agglutination test may or may not be present with IMHA Generated by VetConnect® PLUS: Bilirubin (Urine) Page 1 of 2 Additional Information Physiology Conjugated bilirubin passes freely through the glomerular filtration barrier and is excreted in urine. Unconjugated bilirubin is bound to albumin and does not normally pass through the glomerular filtration barrier. Therefore, it is not detectable in urine (unless albuminuria or glomerular disease is present). Bilirubinuria usually precedes hyperbilirubinemia and icterus Dogs: Clinically normal dogs (especially males) may have detectable bilirubinuria in concentrated urine due to a low renal threshold for bilirubin. -

Leukocyte Esterase Activity in Vaginal Fluid of Pregnant and Non-Pregnant Women with Vaginitis/Vaginosis and in Controls
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Infect Dis Obstet Gynecol 2003;11:19–26 Leukocyte esterase activity in vaginal fluid of pregnant and non-pregnant women with vaginitis/vaginosis and in controls Per-Anders Mårdh 1, Natalia Novikova 1, Ola Niklasson 1, Zoltan Bekassy 1 and Lennart Skude 2 1Department of Obstetrics and Gynecology, University Hospital, Lund and 2Department of Clinical Chemistry, County Hospital, Halmstad, Sweden Objectives: Todeterminethe leukocyteesterase (LE) activity invaginal lavage fluid ofwomen with acuteand recurrentvulvovaginal candidosis (VVC and RVVC respectively), bacterial vaginosis(BV), and in pregnant and non-pregnantwomen without evidenceof the threeconditions. Also tocompare the resultof LEtestsin women consultingat differentweeks inthe cycle andtrimesters of pregnancy.The LEactivity was correlatedto vaginal pH, numberof inflammatory cells instained vaginal smears,type of predominatingvaginal bacteria andpresence of yeast morphotypes. Methods: Onehundred and thirteen women with ahistoryof RVVC,i.e. with at least fourattacks of the conditionduring the previousyear and who had consultedwith anassumed new attack ofthe condition,were studied.Furthermore, we studied16 women with VVC,15 women with BV,and 27 women attendingfor control of cytological abnormalities, who all presentedwithout evidenceof either vaginitisor vaginosis. Finally, 73 pregnantwomen wereinvestigated. The LEactivity invaginal fluid duringdifferent weeks inthe cycle of 53 of the women was measured. Results: Inthe non-pregnantwomen, anincreased LE activity was foundin 96, 88, 73 and56% of those with RVVC,VVC and BV andin the non-VVC/BVcases,respectively. In 73% of pregnantwomen inthe second trimester,and 76% of thosein the third,the LEtestwas positive.In all groupsof non-pregnantwomen tested, the LEactivity correlatedwith the numberof leukocytesin vaginal smears,but it didnot in those who were pregnant.There was nocorrelation between LE activity andweek incycle. -

Surgeons, Columbia University, New York City) (Received for Publication August 9, 1932)
THE ADDIS SEDIMENT COUNT IN NORMAL CHILDREN By JOHN D. LYTTLE (From the Babies Hospit and the Department of Pediatrics, Colege of Physicians and Surgeons, Columbia University, New York City) (Received for publication August 9, 1932) THE METHOD In 1925 Addis (1) described a method by which, in a concentrated acid urine, the rate of excretion of protein, casts and red and white cells could be determined. His method, with certain modifications, has been followed here. All of the counts were made on the 12 hour night specimen from 7 or 8 P.M. to 7 or 8 A.M. Addis recommended that fluids be restricted during, and for 12 hours preceding the collection, since in dilute and alkaline urine hyaline casts dissolve and red cells may be completely lysed. With children this rigid restriction of fluid proved impossible. Withholding fluid during the afternoon and night except for 200 cc. at the evening meal, gave urines of such concentration and acidity that they were suitable for a count. Most children had an early supper and col- lections were started at 7 or 8 P.M. Under these conditions, the urinary pH was between 5.0 and 6.0 and the specific gravity usually well above 1.020. The specimens were treated as described by Addis: "the con- centrated night urine is thoroughly mixed by repeated inversion of the rubber-stoppered bottle and a 10 cc. sample is transferred to a special graduated tube, and centrifugalized for five minutes at 1,800 revolutions per minute. The supernatant urine is decanted and pipetted down to a known volume which varies with the amount of sediment as judged by direct observation. -

Different Response of Body Weight Change According to Ketonuria After Fasting in the Healthy Obese
ORIGINAL ARTICLE Endocrinology, Nutrition & Metabolism http://dx.doi.org/10.3346/jkms.2012.27.3.250 • J Korean Med Sci 2012; 27: 250-254 Different Response of Body Weight Change According to Ketonuria after Fasting in the Healthy Obese Hyeon-Jeong Kim1, Nam-Seok Joo1, The relationship between obesity and ketonuria is not well-established. We conducted a Kwang-Min Kim1, Duck-Joo Lee1, retrospective observational study to evaluate whether their body weight reduction response and Sang-Man Kim2 differed by the presence of ketonuria after fasting in the healthy obese. We used the data of 42 subjects, who had medical records of initial urinalysis at routine health check-up and 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon; follow-up urinalysis in the out-patient clinic, one week later. All subjects in the initial 2Department of Family Medicine, CHA Biomedical urinalysis showed no ketonuria. However, according to the follow-up urinalysis after three Center, CHA University College of Medicine, Seoul, subsequent meals fasts, the patients were divided into a non-ketonuria group and Korea ketonuria group. We compared the data of conventional low-calorie diet programs for ± Received: 20 August 2011 3 months for both groups. Significantly greater reduction of body weight (-8.6 3.6 kg vs 2 2 Accepted: 17 January 2012 -1.1 ± 2.2 kg, P < 0.001), body mass index (-3.16 ± 1.25 kg/m vs -0.43 ± 0.86 kg/m , P < 0.001) and waist circumference (-6.92 ± 1.22 vs -2.32 ± 1.01, P < 0.001) was Address for Correspondence: observed in the ketonuria group compared to the non-ketonuria group. -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

Ileal Neobladder: an Important Cause of Non-Anion Gap Metabolic Acidosis
The Journal of Emergency Medicine, Vol. 52, No. 5, pp. e179–e182, 2017 Ó 2017 Elsevier Inc. All rights reserved. 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2016.12.036 Clinical Communications: Adult ILEAL NEOBLADDER: AN IMPORTANT CAUSE OF NON-ANION GAP METABOLIC ACIDOSIS Jesse W. St. Clair, MD and Matthew L. Wong, MD, MPH Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts and Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts Reprint Address: Matthew L. Wong, MD, MPH, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Rosenberg Building, 2nd Floor, 1 Deaconess Road, Boston, MA 02446 , Abstract—Background: The differential diagnosis for a disease, or medications such as acetazolamide. non-anion gap metabolic acidosis is probably less well Commonly used mnemonics to remember the differential known than the differential diagnosis for an anion gap for the non-anion gap metabolic acidosis include metabolic acidosis. One etiology of a non-anion gap acidosis ‘‘ABCD’’ for ‘‘Addison’s, Bicarbonate loss, Chloride is the consequence of ileal neobladder urinary diversion (administration), and Drugs,’’ as well as ‘‘HARDUP’’ for the treatment of bladder cancer. Case Report: We pre- for ‘‘Hyperchloremia, Acetazolamide and Addison’s, sent a case of a patient with an ileal neobladder with a severe non-anion gap metabolic acidosis caused by a Renal Tubular Acidosis, Diarrhea, Ureteroenterostomies, urinary tract infection and ureteroenterostomy. Why and Pancreaticoenterostomies’’ (Table 1) (1). Should an Emergency Physician Be Aware of This?: Part Ureteroenterostomies are when the ureter has an of the ileal neobladder surgery includes ureteroenteros- abnormal connection with a segment of intestine.