Secondary Analysis of Patients with Low LDL Cholesterol Levels and in Those Already Receiving a Maximal-Potency Statin in a Randomized Clinical Trial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lipid-Lowering Therapy and Low-Density Lipoprotein Cholesterol
Kristensen et al. BMC Cardiovascular Disorders (2020) 20:336 https://doi.org/10.1186/s12872-020-01616-9 RESEARCH ARTICLE Open Access Lipid-lowering therapy and low-density lipoprotein cholesterol goal attainment after acute coronary syndrome: a Danish population-based cohort study Marie Skov Kristensen1, Anders Green2,3, Mads Nybo4, Simone Møller Hede2, Kristian Handberg Mikkelsen5, Gunnar Gislason1,6,7,8, Mogens Lytken Larsen9 and Annette Kjær Ersbøll1* Abstract Background: Patients with acute coronary syndrome (ACS) are at high risk of recurrent cardiovascular (CV) event. The European guidelines recommend low-density lipoprotein cholesterol (LDL-C) levels < 1.8 mmol/L and early initiation of intensive lipid-lowering therapy (LLT) to reduce CV risk. In order to reduce the risk of further cardiac events, the study aimed to evaluate LDL-C goal attainment and LLT intensity in an incident ACS population. Methods: A cohort study of patients with residency at Funen in Denmark at a first-ever ACS event registered within the period 2010–2015. Information on LLT use and LDL-C levels was extracted from national population registers and a Laboratory database at Odense University Hospital. Treatments and lipid patterns were evaluated during index hospitalization, at 6-month and 12-month follow-up. Results: Among 3040 patients with an LDL-C measurement during index hospitalization, 40.7 and 39.0% attained the recommended LDL-C target value (< 1.8 mmol/L) within 6- and 12-month follow-up, respectively. During 6- and 12-month follow-up, a total of 89.2% (20.2%) and 88.4% (29.7%) used LLT (intensive LLT). -

Repatha) Reference Number: PA.CP.PHAR.123 Effective Date: 01/18 Last Review Date: 01/19 Revision Log
Clinical Policy: Evolocumab (Repatha) Reference Number: PA.CP.PHAR.123 Effective Date: 01/18 Last Review Date: 01/19 Revision Log Description Evolocumab (RepathaTM) is a proprotein convertase subtilisin kexin type 9 (PCSK9) inhibitor antibody. FDA Approved Indication(s) Repatha is indicated: • To reduce the risk of myocardial infarction, stroke, and coronary revascularization in adults with established cardiovascular disease • As an adjunct to diet, alone, or in combination with other lipid-lowering therapies (e.g., statins, ezetimibe), for treatment of adults with primary hyperlipidemia (including heterozygous familial hypercholesterolemia) to reduce low-density lipoprotein cholesterol (LDL-C) • As an adjunct to diet and other LDL-lowering therapies (e.g., statins, ezetimibe, LDL apheresis) in patients with homozygous familial hypercholesterolemia (HoFH) who require additional lowering of LDL-C Policy/Criteria Provider must submit documentation (which may include office chart notes and lab results) supporting that member has met all approval criteria It is the policy of health plans affiliated with Pennsylvania Health and Wellness that Repatha is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Heterozygous Familial Hypercholesterolemia and Atherosclerotic Cardiovascular Disease (must meet all): 1. Diagnosis of one of the following (a or b): a. HeFH as defined by one of the following (i or ii): i. World Health Organization (WHO)/Dutch Lipid Network familial hypercholesterolemia diagnostic criteria score of > 8 as determined by requesting provider; ii. Definite diagnosis per Simon Broome criteria); b. Atherosclerotic cardiovascular disease (ASCVD) as evidenced by a history of any one of the following conditions (i-vii): i. Acute coronary syndromes; ii. -

Clinical Policy: Evolocumab (Repatha) Reference Number: CP.CPA.269 Effective Date: 10.15 Last Review Date: 02.19 Line of Business: Commercial Revision Log
Clinical Policy: Evolocumab (Repatha) Reference Number: CP.CPA.269 Effective Date: 10.15 Last Review Date: 02.19 Line of Business: Commercial Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Evolocumab (Repatha®) is a proprotein convertase subtilisin kexin type 9 (PCSK9) inhibitor antibody. FDA Approved Indication(s) Repatha is indicated: • To reduce the risk of myocardial infarction, stroke, and coronary revascularization in adults with established cardiovascular disease • As an adjunct to diet, alone, or in combination with other lipid-lowering therapies (e.g., statins, ezetimibe), for treatment of adults with primary hyperlipidemia (including heterozygous familial hypercholesterolemia) to reduce low-density lipoprotein cholesterol (LDL-C) • As an adjunct to diet and other LDL-lowering therapies (e.g., statins, ezetimibe, LDL apheresis) in patients with homozygous familial hypercholesterolemia (HoFH) who require additional lowering of LDL-C Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Repatha is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Heterozygous Familial Hypercholesterolemia and Atherosclerotic Cardiovascular Disease (must meet all): 1. Diagnosis of one of the following (a or b): a. HeFH as defined by one of the following (i or ii): i. World Health Organization (WHO)/Dutch Lipid Network familial hypercholesterolemia diagnostic criteria score of > 8 as determined by requesting provider (see Appendix D); ii. Definite diagnosis per Simon Broome criteria (see Appendix D); b. -

PCSK9 Inhibitor Non-Response in a Patient with Preserved LDL Receptor
PCSK9 inhibitor non-response in a patient with preserved LDL receptor function: A case study Losh C, Underberg J Murray Hill Medical Group and New York University School of Medicine, New York, NY Background Results Conclusions PCSK9 inhibitors (PCSK9Is) are monoclonal LDL-C levels after three and seven weeks Absence of LDL receptor activity is not the antibodies that bind to serum PCSK9 and Response to Statin Therapy of therapy with alirocumab 75 mg were 235 only mechanism of PCSK9 inhibitor non- delay LDL receptor degradation. Two mg/dL and 239 mg/dL respectively. Three response. An alteration in the PCSK9 PCSK9Is are commercially available: and seven weeks after up-titration, LDL-C Intervention LDL-C (mg/dL) Change (%) evolocumab and alirocumab. FDA approved binding site for alirocumab and indications include LDL cholesterol (LDL-C) was 249 mg/dL and 292 mg/dL, evolocumab is proposed as a hypothetical lowering on maximally tolerated statin respectively. Total duration of alirocumab None 283 — mechanism for non-response in this therapy was 16 weeks. LDL-C was 253 therapy in patients with ASCVD and Familial patient. Other alternatives include Hypercholesterolemia (FH). Among patients mg/dL after 3 weeks of therapy with pitavastatin 2 mg 238 -15.9% immunogenicity, noncompliance, or faulty with LDL receptor mutations, those with evolocumab, at which time PCSK9 1 dose/week partial loss of function typically respond well inhibitor therapy was discontinued due to pitavastatin 2 mg injection techniqueReferences. 216 -23.7% to PCSK9 inhibition, while those with lack of clinical response. 2 doses/week Amgen Inc. (2015). Repatha: Highlights of homozygous receptor-negative mutations, pitavastatin 2 mg ie. -

Praluent (Alirocumab) Repatha (Evolocumab) Effective 12/1/2019
Praluent (alirocumab) Repatha (evolocumab) Effective 12/1/2019 ☒ MassHealth Plan ☒ ☒Commercial/Exchange Prior Authorization Program Type ☐ Quantity Limit ☒ Pharmacy Benefit Benefit ☐ Step Therapy ☐ Medical Benefit (NLX) Specialty N/A Limitations Specialty Medications All Plans Phone: 866-814-5506 Fax: 866-249-6155 Non-Specialty Medications Contact MassHealth Phone: 877-433-7643 Fax: 866-255-7569 Information Commercial Phone: 800-294-5979 Fax: 888-836-0730 Exchange Phone: 855-582-2022 Fax: 855-245-2134 Medical Specialty Medications (NLX) All Plans Phone: 844-345-2803 Fax: 844-851-0882 Exceptions N/A Overview Alirocumab (Praluent) and evolocumab (Repatha) are human monoclonal antibodies that bind to proprotein convertase subtilisin kexin type 9 (PCSK9). PCSK9 binds to LDL-receptors (LDLR) on the surface of hepatocytes to promote LDLR degradation in the liver. LDLR is the primary receptor that clears LDL; therefore, the decrease in LDLR levels by PCSK9 results in increased blood levels of LDL- C. By inhibiting PCSK9 binding to LDLR, these medications increase the number of LDLRs to lower LDL-C levels. Approvable Indications Alirocumab (Praluent) 1. Adjunct to diet and maximally tolerated statin therapy for the treatment of adults with Heterozygous Familial Hypercholesterolemia (HeFH) 2. Clinical atherosclerotic cardiovascular disease (ASCVD), who require additional lowering of low- density lipoprotein (LDL)-cholesterol (LDL-C). 3. To reduce the risk of serious cardiovascular events (e.g., MI, stroke and unstable angina) requiring hospitalization in adults with established cardiovascular disease. 4. Secondary prevention of cardiovascular events: To reduce the risk of MI, stroke, and unstable angina requiring hospitalization in adults with established cardiovascular disease Evolocumab (Repatha) 1. -

CAR-T and Gene Therapies: Hope Is on the Horizon
Magellan Rx Report Fall 2017 Opioid-Induced Osteoporosis in the Star Ratings and Variable Fee Schedule Constipation: Managed Care Setting: Quality Improvement: Reimbursement: Associated Costs of A Rising Challenge with Forecasted Measures Impact on Antiemetic Care and Length of Growing Treatment for 2019 and Program Utilization and Hospitalization Opportunities Successes Quality of Care Magellan Rx Report MEDICAL AND PHARMACY BENEFIT MANAGEMENT Fall 2017 CAR-T and Gene Therapies: Hope Is on the Horizon magellanrx.com See for yourself what it’s like in virtual reality Download the free app at InMyEyesApp.com. Doctor-recommended screening, diagnosis, and potential treatment are important for your members with Wet AMD, Macular Edema following RVO, DME, and DR in Patients with DME.* Otherwise, these members may be facing serious risk of vision loss, which may require ongoing resources.1-3 THERE’S EYLEA—A treatment option that can fit your plan • EYLEA has proven outcomes as demonstrated in phase 3 clinical trials in patients with Wet AMD, Macular Edema following RVO, DME, and DR in Patients with DME4 • With monthly and every-other-month dosing,† EYLEA offers exible dosing options to help meet the needs of your providers and your members4 INDICATIONS AND IMPORTANT SAFETY INFORMATION INDICATIONS • EYLEA® (aflibercept) Injection is indicated for the treatment • There is a potential risk of arterial thromboembolic events of patients with Neovascular (Wet) Age-related Macular (ATEs) following intravitreal use of VEGF inhibitors, including Degeneration (AMD), Macular Edema following Retinal Vein EYLEA. ATEs are defined as nonfatal stroke, nonfatal myocardial Occlusion (RVO), Diabetic Macular Edema (DME), and infarction, or vascular death (including deaths of unknown Diabetic Retinopathy (DR) in Patients with DME. -

Evolocumab (REPATHA®) National Drug Monograph December 2015 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives
Insert Generic Drug Name Here Monograph Evolocumab (REPATHA®) National Drug Monograph December 2015 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information1 Description/Mechanism of Action Evolocumab (REPATHA®) is a humanized monoclonal antibody targeting proprotein convertase subtilisin/kexin type 9 (PCSK9). Proprotein convertase subtilisin/ kexin type 9 binds to LDL receptors on the surface of hepatocytes and promotes degradation of the LDL receptor in the liver. Inhibition of PCSK9 by evolocumab leads to reduced degradation of the LDL receptor resulting in a greater number of LDL receptors available to clear LDL and subsequently, lower circulating LDL. Indication(s) Under Review in Evolocumab was approved by the FDA as an adjunct to diet and: this document (may include 1) Maximally tolerated statin therapy for the treatment of adults with off label) heterozygous familial hypercholesterolemia (HeFH) or clinical atherosclerotic cardiovascular disease (ASCVD), who require additional lowering of low-density lipoprotein cholesterol (LDL-C). 2) Other LDL lowering therapies (e.g., statins, ezetimibe, LDL apheresis) in patients with homozygous familial hypercholesterolemia (HoFH) who require additional LDL lowering. *The effect of evolocumab on cardiovascular morbidity or mortality has not yet been determined. Dosage Form(s) Under For patients with HeFH or those with established ASCVD who require Review additional LDL lowering, the initial dose of evolocumab is 140 mg given subcutaneously (SQ) every 2 weeks OR 420 mg once a month. -

Bempedoic Acid, Bempedoic Acid/Ezetimibe (Nexletol™, Nexlizet™) EOCCO POLICY Policy Type: PA/SP Pharmacy Coverage Policy: EOCCO182
bempedoic acid, bempedoic acid/ezetimibe (Nexletol™, Nexlizet™) EOCCO POLICY Policy Type: PA/SP Pharmacy Coverage Policy: EOCCO182 Description Bempedoic acid, bempedoic acid/ezetimibe (Nexletol, Nexlizet) is an orally administered adenosine triphosphate-citrate lyase inhibitor, and ezetimibe is an intestinal cholesterol absorption inhibitor . Length of Authorization Initial: six months Renewal: 12 months Quantity Limits Product Name Dosage Form Indication Quantity Limit As an adjunct to diet and bempedoic acid maximally tolerated statin 180 mg tablets 30 tablets/30 days (Nexletol) therapy for the treatment of adults with heterozygous familial hypercholesterolemia or bempedoic established atherosclerotic 180 mg/10 mg tablets acid/ezetimibe cardiovascular disease who 30 tablets/30 days (Nexlizet) require additional lowering of LDL-C Initial Evaluation I. Bempedoic acid, bempedoic acid/ezetimibe (Nexletol, Nexlizet) may be considered medically necessary when the following criteria below are met: A. Member is 18 years of age or older; AND B. Therapy is prescribed by, or in consultation with, a provider specializing in lipid management (e.g. cardiology, lipidology, endocrinology); AND C. Therapy with a maximally tolerated statin for at least an 8-week duration has been ineffective; AND 1. The member continues to have an LDL-cholesterol level greater than or equal to 70 mg/dL while on maximally tolerated statin therapy; AND 2. The member will continue maximally tolerated statin therapy in combination with bempedoic acid, bempedoic acid/ezetimibe (Nexletol, Nexlizet); AND 1 bempedoic acid, bempedoic acid/ezetimibe (Nexletol™, Nexlizet™) EOCCO POLICY 3. The member will not use bempedoic acid, bempedoic acid/ezetimibe (Nexletol, Nexlizet) in combination with simvastatin (Zocor) >20 mg or pravastatin (Pravachol) >40 mg; OR i. -
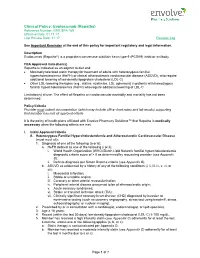
Evolocumab (Repatha) Reference Number: ERX.SPA.169 Effective Date: 01.11.17 Last Review Date: 11.17 Revision Log
Clinical Policy: Evolocumab (Repatha) Reference Number: ERX.SPA.169 Effective Date: 01.11.17 Last Review Date: 11.17 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Evolocumab (Repatha®) is a proprotein convertase subtilisin kexin type 9 (PCSK9) inhibitor antibody. FDA Approved Indication(s) Repatha is indicated as an adjunct to diet and: Maximally tolerated statin therapy for treatment of adults with heterozygous familial hypercholesterolemia (HeFH) or clinical atherosclerotic cardiovascular disease (ASCVD), who require additional lowering of low density lipoprotein cholesterol (LDL-C) Other LDL-lowering therapies (e.g., statins, ezetimibe, LDL apheresis) in patients with homozygous familial hypercholesterolemia (HoFH) who require additional lowering of LDL-C Limitation(s) of use: The effect of Repatha on cardiovascular morbidity and mortality has not been determined. Policy/Criteria Provider must submit documentation (which may include office chart notes and lab results) supporting that member has met all approval criteria It is the policy of health plans affiliated with Envolve Pharmacy Solutions™ that Repatha is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Heterozygous Familial Hypercholesterolemia and Atherosclerotic Cardiovascular Disease (must meet all): 1. Diagnosis of one of the following (a or b): a. HeFH defined as one of the following (i or ii): i. World Health Organization (WHO)/Dutch Lipid Network familial hypercholesterolemia diagnostic criteria score of > 8 as determined by requesting provider (see Appendix B); ii. Definite diagnosis per Simon Broome criteria (see Appendix B); b. ASCVD as evidenced by a history of any of the following conditions (i, ii, iii, iv, v, vi, or vii): i. -

Enhancing the Value of PCSK9 Monoclonal Antibodies by Identifying Patients Most Likely to Benefit
Journal of Clinical Lipidology (2019) -, -–- Enhancing the value of PCSK9 monoclonal antibodies by identifying patients most likely to benefit Jennifer G. Robinson, MD, MPH*, Manju Bengularu Jayanna, MBBS, Alan S. Brown, MD, FACC, FNLA, Karen Aspry, MD, MS, FACC, FNLA, FAHA, Carl Orringer, MD, FNLA, Edward A. Gill, MD, FNLA, FASE, FACP, FACC, FAHA, Anne Goldberg, MD, FACP, FNLA, Laney K. Jones, PharmD, MPH, Kevin Maki, PhD, Dave L. Dixon, PharmD, Joseph J. Saseen, PharmD, FNLA, Daniel Soffer, MD, FNLA, FACP Division of Cardiology, Departments of Epidemiology and Internal Medicine, University of Iowa, Iowa City, IA, USA (Dr Robinson); Division of Cardiology, Departments of Epidemiology and Internal Medicine, University of Iowa, Iowa City, IA, USA (Dr Jayanna); Division of Cardiology, Advocate Heart Institute at Advocate Lutheran General Hospital, Park Ridge, IL, USA (Dr Brown); Brown University, Alpert Medical School, Lifespan Cardiovascular Institute, RI, USA (Dr Aspry); University of Miami Miller School of Medicine, Miami, FL, USA (Dr Orringer); Division of Cardiology, University of Colorado School of Medicine, Aurora, CO, USA (Dr Gill); Professor of Medicine, Washington University School of Medicine, St. Louis, MO, USA (Dr Goldberg); Genomic Medicine Institute, Danville, PA, USA (Dr Jones); Midwest Biomedical Research, Center for Metabolic and Cardiovascular Health, Wheaton, IL, USA (Dr Maki); Department of Pharmacotherapy & Outcomes Science, Virginia Commonwealth University, Richmond, VA, USA (Dr Dixon); University of Colorado Anschutz Medical Campus, Aurora, CO, USA (Dr Saseen); and Department of Internal Medicine, University of Pennsylvania Health System, Philadelphia, PA, USA (Dr Soffer) KEYWORDS: Abstract: Acquisition costs and cost-effectiveness have limited access and recommendations to use PCSK9 inhibitors; proprotein convertase subtilisin/kexin type 9 (PCSK9)–inhibiting monoclonal antibodies (mAbs). -

Effect of Evolocumab Or Ezetimibe Added to Moderate
Research Original Investigation Effect of Evolocumab or Ezetimibe Added to Moderate- or High-Intensity Statin Therapy on LDL-C Lowering in Patients With Hypercholesterolemia The LAPLACE-2 Randomized Clinical Trial Jennifer G. Robinson, MD, MPH; Bettina S. Nedergaard, MD, PhD; William J. Rogers, MD; Jonathan Fialkow, MD; Joel M. Neutel, MD; David Ramstad, MD, MPH; Ransi Somaratne, MD, MBA; Jason C. Legg, PhD; Patric Nelson, MPH, MBA; Rob Scott, MD; Scott M. Wasserman, MD; Robert Weiss, MD; for the LAPLACE-2 Investigators Supplemental content at IMPORTANCE In phase 2 studies, evolocumab, a fully human monoclonal antibody to PCSK9, jama.com reduced LDL-C levels in patients receiving statin therapy. OBJECTIVE To evaluate the efficacy and tolerability of evolocumab when used in combination with a moderate- vs high-intensity statin. DESIGN, SETTING, AND PATIENTS Phase 3, 12-week, randomized, double-blind, placebo- and ezetimibe-controlled study conducted between January and December of 2013 in patients with primary hypercholesterolemia and mixed dyslipidemia at 198 sites in 17 countries. INTERVENTIONS Patients (n = 2067) were randomized to 1 of 24 treatment groups in 2 steps. Patients were initially randomized to a daily, moderate-intensity (atorvastatin [10 mg], simvastatin [40 mg], or rosuvastatin [5 mg]) or high-intensity (atorvastatin [80 mg], rosuvastatin [40 mg]) statin. After a 4-week lipid-stabilization period, patients (n = 1899) were randomized to compare evolocumab (140 mg every 2 weeks or 420 mg monthly) with placebo (every 2 weeks or monthly) or ezetimibe (10 mg or placebo daily; atorvastatin patients only) when added to statin therapies. MAIN OUTCOMES AND MEASURES Percent change from baseline in low-density lipoprotein cholesterol (LDL-C) level at the mean of weeks 10 and 12 and at week 12. -

Anatomical Classification Guidelines V2020 EPHMRA ANATOMICAL
EPHMRA ANATOMICAL CLASSIFICATION GUIDELINES 2020 Anatomical Classification Guidelines V2020 "The Anatomical Classification of Pharmaceutical Products has been developed and maintained by the European Pharmaceutical Marketing Research Association (EphMRA) and is therefore the intellectual property of this Association. EphMRA's Classification Committee prepares the guidelines for this classification system and takes care for new entries, changes and improvements in consultation with the product's manufacturer. The contents of the Anatomical Classification of Pharmaceutical Products remain the copyright to EphMRA. Permission for use need not be sought and no fee is required. We would appreciate, however, the acknowledgement of EphMRA Copyright in publications etc. Users of this classification system should keep in mind that Pharmaceutical markets can be segmented according to numerous criteria." © EphMRA 2020 Anatomical Classification Guidelines V2020 CONTENTS PAGE INTRODUCTION A ALIMENTARY TRACT AND METABOLISM 1 B BLOOD AND BLOOD FORMING ORGANS 28 C CARDIOVASCULAR SYSTEM 35 D DERMATOLOGICALS 50 G GENITO-URINARY SYSTEM AND SEX HORMONES 57 H SYSTEMIC HORMONAL PREPARATIONS (EXCLUDING SEX HORMONES) 65 J GENERAL ANTI-INFECTIVES SYSTEMIC 69 K HOSPITAL SOLUTIONS 84 L ANTINEOPLASTIC AND IMMUNOMODULATING AGENTS 92 M MUSCULO-SKELETAL SYSTEM 102 N NERVOUS SYSTEM 107 P PARASITOLOGY 118 R RESPIRATORY SYSTEM 120 S SENSORY ORGANS 132 T DIAGNOSTIC AGENTS 139 V VARIOUS 141 Anatomical Classification Guidelines V2020 INTRODUCTION The Anatomical Classification was initiated in 1971 by EphMRA. It has been developed jointly by Intellus/PBIRG and EphMRA. It is a subjective method of grouping certain pharmaceutical products and does not represent any particular market, as would be the case with any other classification system.