ICS/IUGA 2010 Sunday 22Nd August 2010 Scientific Programme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Laparoscopic Organopexy with Non-Mesh Genital (LONG)
www.nature.com/scientificreports OPEN Laparoscopic Organopexy with Non-mesh Genital (LONG) Suspension: A Novel Uterine Received: 14 November 2017 Accepted: 19 February 2018 Preservation Procedure for the Published: xx xx xxxx Treatment of Apical Prolapse Cheng-Yu Long1,2,3, Chiu-Lin Wang2,3, Chin-Ru Ker1, Yung-Shun Juan4, Eing-Mei Tsai1,3 & Kun-Ling Lin 1,3 To assess whether our novel uterus-sparing procedure- laparoscopic organopexy with non-mesh genital(LONG) suspension is an efective, safe, and timesaving surgery for the treatment of apical prolapse. Forty consecutive women with main uterine prolapse stage II or greater defned by the POP quantifcation(POP-Q) staging system were referred for LONG procedures at our hospitals. Clinical evaluations before and 6 months after surgery included pelvic examination, urodynamic study, and a personal interview to evaluate urinary and sexual symptoms with overactive bladder symptom score(OABSS), the short forms of Urogenital Distress Inventory(UDI-6) and Incontinence Impact Questionnaire(IIQ-7), and the Female Sexual Function Index(FSFI). After follow-up time of 12 to 30 months, anatomical cure rate was 85%(34/40), and the success rates for apical, anterior, and posterior vaginal prolapse were 95%(38/40), 85%(34/40), and 97.5%(39/40), respectively. Six recurrences of anterior vaginal wall all sufered from signifcant cystocele (stage3; Ba>+1) preoperatively. The average operative time was 73.1 ± 30.8 minutes. One bladder injury occurred and was recognized during surgery. The dyspareunia domain and total FSFI scores of the twelve sexually-active premenopausal women improved postoperatively in a signifcant manner (P < 0.05). -

Chapter 14 – Female Reproductive Organs
Chapter 14 – Female reproductive organs The fee allowance for a hysteroscopy procedure includes an amount for dilation and curettage (D&C) and the insertion of a Mirena coil so we will not reimburse additional fees charged for these procedures. Similarly, where a therapeutic hysteroscopy is carried out, we will not pay any additional fees charged for a diagnostic hysteroscopy. The fee allowance for a hysterectomy procedure for ovarian malignancy includes an amount for the removal of the omentum and so this should not be charged as an additional procedure. A cystoscopy should not be charged as an additional procedure alongside any suspension/uro-gynaecological procedure. The insertion of a suprapubic catheter is considered part and parcel of procedures such as a suprapubic sling or the retropubic suspension of the bladder neck and so we will not pay any additional fees charged for this procedure. The fee allowance for a colposcopy procedure includes an amount for a punch biopsy. The fee allowance for a therapeutic laparoscopy includes an amount for a diagnostic laparoscopy. The code for the insertion of a prosthesis into the ureter is intended for use by urologists inserting a stent and not for circumstances where the ureter is being identified during hysterectomy. However, we recognise this does involve some additional work and consider a small uplift in the fee to be reasonable. Many pathological processes result in the formation of adhesions so ‘adhesiolysis’ is considered to be a normal part and parcel of these procedures. Therefore, we do not have a specific code for the division of adhesions. -

To Repair Uterine Prolapse
IP 372/2 [IPGXXX] NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE INTERVENTIONAL PROCEDURES PROGRAMME Interventional procedure overview of uterine suspension using mesh (including sacrohysteropexy) to repair uterine prolapse Uterine prolapse happens when the womb (uterus) slips down from its usual position into the vagina. Uterine suspension using mesh involves attaching 1 end of the mesh to the lower part of the uterus or cervix. The other end is attached to a bone at the base of the spine or to a ligament in the pelvis. The procedure can be done through open abdominal surgery or laparoscopy (keyhole surgery). The aim is to support the womb. Introduction The National Institute for Health and Care Excellence (NICE) has prepared this interventional procedure (IP) overview to help members of the interventional procedures advisory committee (IPAC) make recommendations about the safety and efficacy of an interventional procedure. It is based on a rapid review of the medical literature and specialist opinion. It should not be regarded as a definitive assessment of the procedure. Date prepared This IP overview was prepared in January 2016. Procedure name Uterine suspension using mesh (including sacrohysteropexy) to repair uterine prolapse. Specialist societies Royal College of Obstetricians and Gynaecologists (RCOG) British Society of Urogynaecology (BSUG) British Association of Urological Surgeons (BAUS). IP overview: Uterine suspension using mesh (including sacrohysteropexy) to repair uterine prolapse. Page 1 of 75 IP 372/2 [IPGXXX] Description Indications and current treatment Uterine prolapse is when the uterus descends from its usual position, into and sometimes through, the vagina. It can affect quality of life by causing symptoms of pressure and discomfort, and by its effects on urinary, bowel and sexual function. -

Sl.No CGHS Treatment Procedure/Investigation List Rates for Non NABH Rates for NABH CGHS Bengaluru Rate List
CGHS Bengaluru Rate List Sl.No CGHS Treatment Procedure/Investigation Rates for Non Rates for List NABH NABH 1 Consultation OPD 135 135 2 Consultation- for Inpatients 270 270 3 Dressings of wounds 45 52 4 Suturing of wounds with local anesthesia 108 124 5 Aspiration Plural Effusion - Diagnostic 120 138 6 Aspiration Plural Effusion - Therapeutic 174 200 7 Abdominal Aspiration - Diagnostic 330 380 8 Abdominal Aspiration - Therapeutic 414 476 9 Pericardial Aspiration 342 393 10 Joints Aspiration 285 329 11 Biopsy Skin 207 239 12 Removal of Stitches 36 41 13 Venesection 124 143 14 Phimosis Under LA 1180 1357 15 Sternal puncture 173 199 16 Injection for Haemorrhoids 373 428 17 Injection for Varicose Veins 315 363 18 Catheterisation 425 500 19 Dilatation of Urethra 450 518 20 Incision & Drainage 378 435 21 Intercostal Drainage 125 144 22 Peritoneal Dialysis 1319 1517 TREATMENT PROCEDURE SKIN 23 Excision of Moles 311 357 24 Excision of Warts 279 321 25 Excision of Molluscum contagiosum 117 135 26 Excision of Veneral Warts 144 166 27 Excision of Corns 126 145 28 I/D Injection Keloid 97 112 29 Chemical Cautery (s) 99 114 TREATMENT PROCEDURE OPTHALMOLOGY 30 66 76 eyes Subconjunctival/subtenon’s injections in one 31 132 152 eyes 32 PterygiumSubconjunctival/subtenon’s Surgery injections in both 5550 6325 33 Conjunctival Peritomy 58 67 34 Conjunctival wound repair or exploration 3300 3795 following blunt trauma 35 Removal of corneal foreign body 115 132 36 Cauterization of ulcer/subconjunctival injection 69 79 in one eye 37 Cauterization of ulcer/subconjunctival -

Abdominal Sacrohysteropexy Versus Vaginal Hysterectomy for Pelvic Organ Prolapse in Young Women
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Bhalerao AV et al. Int J Reprod Contracept Obstet Gynecol. 2020 Apr;9(4):1434-1441 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20201201 Original Research Article Abdominal sacrohysteropexy versus vaginal hysterectomy for pelvic organ prolapse in young women Anuja V. Bhalerao, Vaidehi A. Duddalwar* Department of Obstetrics and Gynecology, N. K. P. Salve Institute of Medical Sciences, Nagpur, Maharashtra, India Received: 11 February 2020 Accepted: 03 March 2020 *Correspondence: Dr. Vaidehi A. Duddalwar, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Pelvic organ prolapse (POP) is the descent of the pelvic organs beyond their anatomical confines. The definitive treatment of symptomatic prolapse is surgery but its management in young is unique due to various considerations. Aim of this study was to evaluate anatomical and functional outcome after abdominal sacrohysteropexy and vaginal hysterectomy for pelvic organ prolapse in young women. Methods: A total 27 women less than 35 years of age with pelvic organ prolapse underwent either abdominal sacrohysteropexy or vaginal hysterectomy with repair. In all women, pre-op and post-op POP-Q was done for evaluation of anatomical defect and a validated questionnaire was given for subjective outcome. Results: Anatomical outcome was significant in both groups as per POP-Q grading but the symptomatic outcome was better for sacrohysteropexy with regard to surgical time, bleeding, ovarian conservation, urinary symptoms, sexual function. -
General User Charges in AIIMS Raipur
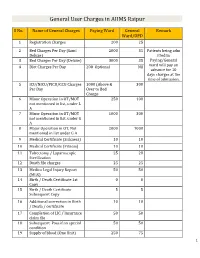
General User Charges in AIIMS Raipur S No. Name of General Charges Paying Ward General Remark Ward/OPD 1 Registration Charges 200 25 2 Bed Charges Per Day (Sami 2000 35 Patients being adm Deluxe) itted in 3 Bed Charges Per Day (Deluxe) 3000 35 Paying/General 4 Diet Charges Per Day 200 Optional Nil ward will pay an advance for 10 days charges at the time of admission. 5 ICU/NICU/PICU/CCU Charges 1000 (Above & 300 Per Day Over to Bed Charge 6 Minor Operation in OT/MOT 250 100 not mentioned in list, under L A 7 Minor Operation in OT/MOT 1000 300 not mentioned in list, under G A 8 Major Operation in OT, Not 2000 1000 mentioned in list under G A 9 Medical Certificate (Sickness) 10 10 10 Medical Certificate (Fitness) 10 10 11 Tubectomy / Laparoscopic 25 20 Sterilization 12 Death file charges 25 25 13 Medico Legal Injury Report 50 50 (MLR) 14 Birth / Death Certificate 1st 0 0 Copy 15 Birth / Death Certificate 5 5 Subsequent Copy 16 Additional correction in Birth 10 10 / Death / certificate 17 Completion of LIC / Insurance 50 50 claim file 18 Subsequent Pass if on special 50 50 condition 19 Supply of blood (One Unit) 250 75 1 20 Medical Board Certificate 500 500 On Special Case User Charges for Investigations in AIIMS Raipur S No. Name of Investigations Paying General Remark Ward Ward/OPD Anaesthsia 1 ABG 75 50 2 ABG ALONGWITH 150 100 ELECTROLYTES(NA+,K+)(Na,K) 3 ONLY ELECTROLYTES(Na+,K+,Cl,Ca+) 75 50 4 ONLY CALCIUM 50 25 5 GLUCOSE 25 20 6 LACTATE 25 20 7 UREA. -

Sacrohysteropexy for Uterine Prolapse (Womb Prolapse)
Sacrohysteropexy for Uterine Prolapse (Womb Prolapse) Patient Information Leaflet About this leaflet You should use the information provided in this leaflet as a guide. The way each gynaecologist does this procedure may vary slightly as will care in the hospital after your procedure and the advice given to you when you get home. You should ask your gynaecologist about any concerns that you may have. You should take your time to read this leaflet. A page is provided at the end of the leaflet for you to write down any questions you may have. It is your right to know about your planned operation or procedure, why it has been recommended, what the alternatives are and what the risks and benefits are. These should be covered in this leaflet. You may also want to ask about your gynaecologist’s experience and results of treating your condition. Benefits and risks There are not many studies about the success and the risks of most of the procedures carried out to treat prolapse and incontinence, so it is often difficult to state them clearly. In this leaflet, we may refer to risks as common, rare and so on, or we may give an approximate level of risk. You can find more information about risk in a leaflet ‘Understanding how risk is discussed in healthcare’ published by the Royal College of Obstetricians and Gynaecologists. https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pi- understanding-risk.pdf The following table is taken from that leaflet British Society of Urogynaecology (BSUG) database To understand the success and risks of surgery for prolapse and incontinence the British Society of Urogynaecology has set up a national database. -

Shirodkar's Extended Manchester Repair
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 10, Issue 2, 2014 pp 263-266 Shirodkar’s Extended Manchester Repair: A Conservative Vaginal Surgery for Genital Prolapse in Young Women and Reinforcement of Weak Uterosacral Ligaments with Merselene Tape: Retrospective and Prospective Study Roohi Shaikh 1, Suman Sardesai 2* 1Assistant Professor, Department of OBGY, Indian Institute of Medical Science and Research, Warudi, Badnapur, Jalna Maharashtra INDIA. 2Professor and HOD, Department of OBGY, Dr. V. M. Medical College, Solapur, INDIA. *Corresponding Address: *[email protected], #[email protected] Research Article Abstract: The aim of this study was to evaluate the results of ligaments to the anterior aspect of what remains of the Shirodkar Extended Manchester Repair operation for uterine cervix, an anterior colporrphaphy and perineorhhapy is prolapse in young women interested in retaining future done. This time honoured technique has various childbearing and menstrual function. Materials and Methods: 30 patients with II or III degree utero-vaginal prolapse with or without shortcomings i.e. cervical stenosis, infertility, cervical cystoenterorectocoele and with normal uterocervical length (i.e. no incompetence, cervical dystocia during labour, cervical elongation) in child-bearing age group (i.e. less than 35 dyspareunia and recurrence of prolapse after pregnancy or years) interested in preserving future fertility or menstrual function otherwise was also reported to the extent of 20-25% were operated and followed-up. In patients with weak uterosacral (Shaw 1933).An ideal conservative method should ligament, reinforcement with merselene tape was done. Results: In preserve menstruation, restore the fertility and should not this study, 79% of the patients were below the age of 30 years. -

UNMH Obstetrics and Gynecology Clinical Privileges Name
UNMH Obstetrics and Gynecology Clinical Privileges Name:____________________________ Effective Dates: From __________ To ___________ All new applicants must meet the following requirements as approved by the UNMH Board of Trustees, effective April 28, 2017: Initial Privileges (initial appointment) Renewal of Privileges (reappointment) Expansion of Privileges (modification) INSTRUCTIONS: Applicant: Check off the “requested” box for each privilege requested. Applicants have the burden of producing information deemed adequate by the Hospital for a proper evaluation of current competence, current clinical activity, and other qualifications and for resolving any doubts related to qualifications for requested privileges. Department Chair: Check the appropriate box for recommendation on the last page of this form. If recommended with conditions or not recommended, provide condition or explanation. OTHER REQUIREMENTS: 1. Note that privileges granted may only be exercised at UNM Hospitals and clinics that have the appropriate equipment, license, beds, staff, and other support required to provide the services defined in this document. Site-specific services may be defined in hospital or department policy. 2. This document defines qualifications to exercise clinical privileges. The applicant must also adhere to any additional organizational, regulatory, or accreditation requirements that the organization is obligated to meet. --------------------------------------------------------------------------------------------------------------------------------------- -

SCHEDULE of CHARGES -2018 (Eff Ective from 01.04.2018 to 31.03.2020)
HOLY FAMILY HOSPITAL, NEW DELHI. SCHEDULE OF CHARGES -2018 (Eff ective from 01.04.2018 to 31.03.2020) HOLY FAMILY HOSPITAL HOLOKHLAY ROFAMILAD, NEWY DELHIHOSPIT - 110025AL HOLOKHLAY ROFAMILAD, NEWY DELHIHOSPIT - 110025AL OKHLA ROAD, NEW DELHI - 110025 HOLY FAMILY HOSPITAL OKHLASchedule ROAD, NEW of DELHICharges - 110025 ScheduleEffective 1of April, Charges 2018 ScheduleEffective 1of April, Charges 2018 Effective 1 April, 2018 Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 +91 11 2684 5900 to 2684 5909 Email : [email protected] Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 P hone Nos: Schedule +91+91 1111 Schedule 26842633 59002800 toto 26842633 of 59092809 ChargesofEmailF axCharges No : adimini: +91 11 [email protected] - 32252018 +91 11 Schedule2684 5900 to 2684 5909 ofEmail Charges : [email protected] Effective 1 April,st 2018 Eff Effectiveecti ve from 1 April, 1 April, 2018 2018 (Valid upto 31st March, 2020) Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 +91 11 2684 5900 to 2684 5909 Email : [email protected] +91 11 2684 5900 to 2684 5909 1 Email : [email protected] HOLY FAMILY HOSPITAL, NEW DELHI. SCHEDULE OF CHARGES -2018 (Effective from 01.04.2018 to 31.03.2020) INDEX S.No. CHARGING HEAD Page No. 1 General Information 3 In-Patient Schedule of Charges 2 Room / Bed and Board 5 3 CCU/ICU / Ped. ICU / Post Op. ICU and Board 5 4 Oxygen 5 5 Ventilator 5 6 NNU – Nursery, Photo Therapy, Incubator, Nursing Care 5 7 Hospital Doctor’s Fee :- Visits 6 8 :- Consultation 6 9 Surgery Fee : General Surgery 6 10 Surgery Fee : Laparoscopic General Surgery 9 11 Surgery Fee : Hernia Surgery 12 12 Surgery Fee : Breast Surgery 12 13 Surgery Fee : Rectal Surgery 13 14 Surgery Fee : O.B. -

ICD-9-CM Procedures (FY10)
2 PREFACE This sixth edition of the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) is being published by the United States Government in recognition of its responsibility to promulgate this classification throughout the United States for morbidity coding. The International Classification of Diseases, 9th Revision, published by the World Health Organization (WHO) is the foundation of the ICD-9-CM and continues to be the classification employed in cause-of-death coding in the United States. The ICD-9-CM is completely comparable with the ICD-9. The WHO Collaborating Center for Classification of Diseases in North America serves as liaison between the international obligations for comparable classifications and the national health data needs of the United States. The ICD-9-CM is recommended for use in all clinical settings but is required for reporting diagnoses and diseases to all U.S. Public Health Service and the Centers for Medicare & Medicaid Services (formerly the Health Care Financing Administration) programs. Guidance in the use of this classification can be found in the section "Guidance in the Use of ICD-9-CM." ICD-9-CM extensions, interpretations, modifications, addenda, or errata other than those approved by the U.S. Public Health Service and the Centers for Medicare & Medicaid Services are not to be considered official and should not be utilized. Continuous maintenance of the ICD-9- CM is the responsibility of the Federal Government. However, because the ICD-9-CM represents the best in contemporary thinking of clinicians, nosologists, epidemiologists, and statisticians from both public and private sectors, no future modifications will be considered without extensive advice from the appropriate representatives of all major users. -

Sacrohysteropexy for Uterine Prolapse
INFORMATION FOR PATIENTS Sacrohysteropexy for uterine prolapse We advise you to take your time to read If you have had a hysterectomy then the this leaflet. If you have any questions term ‘vault' is used to describe the area please write them down on the sheet where your womb would have been provided (towards the back) and we can attached to the top of the vagina. discuss them with you at our next meeting. It is your right to know about the Figure 1: A diagram, sideways on, operations being proposed, why they are showing the normal anatomy (dotted line) being proposed, what alternatives there and a prolapsing vaginal apex(continuous are and what the risks are. These should line). be covered in this leaflet. This leaflet describes what an apical vaginal prolapse is, what alternatives are available within our Trust, the risks involved in surgery and what operation we can offer. What is prolapse of the uterus/vaginal apex? A prolapse is where the vaginal tissue is weak and bulges downwards into the vagina itself. It is often accompanied by a posterior vaginal wall prolapse, either a high In severe cases it can even protrude posterior vaginal wall prolapse called an outside the vagina. Apical vaginal enterocele, or a low posterior vaginal Wall prolapse is a prolapse arising from the prolapse called a rectocele, or sometimes top of the vagina. The apex is the both. deepest part of the vagina (top of it/ roof) where the uterus (womb) usually is The pelvic floor muscles are a series of located.