Dissertation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inositol Safety: Clinical Evidences
European Review for Medical and Pharmacological Sciences 2011; 15: 931-936 Inositol safety: clinical evidences G. CARLOMAGNO, V. UNFER AGUNCO Obstetrics & Gynecology Center, Rome (Italy) Abstract. – Myo-inositol is a six carbon ent required by the human cells for the growth cyclitol that contains five equatorial and one axi- and survival in the culture. In humans and other al hydroxyl groups. Myo-inositol has been classi- species, Myo-inositol can be converted to either fied as an insulin sensitizing agent and it is L- or D-chiro-inositol by epimerases. Early stud- commonly used in the treatment of the Polycys- tic Ovary Syndrome (PCOS). However, despite ies showed that inositol urinary clearance was al- its wide clinical use, there is still scarce informa- tered in type 2 diabetes patients, the next step tion on the myo-inositol safety and/or side ef- was to link impaired inositol clearance with in- fects. The aim of the present review was to sum- sulin resistance (for a review see1). Because of marize and discuss available data on the myo-in- these properties, inositol have been classified as ositol safety both in non-clinical and clinical set- “insulin sensitizing agent”2. tings. The main outcome was that only the highest In the recent years, inositol has found more dose of myo-inositol (12 g/day) induced mild and more space in the reproductive clinical prac- gastrointestinal side effects such as nausea, fla- tice3-6. Indeed, since the main therapy for Poly- tus and diarrhea. The severity of side effects did cystic Ovary Syndrome (PCOS) is the use of in- not increase with the dosage. -

Steroid Recognition and Regulation of Hormone Action: Crystal
Research Article 799 Steroid recognition and regulation of hormone action: crystal structure of testosterone and NADP+ bound to 3a-hydroxysteroid/ dihydrodiol dehydrogenase Melanie J Bennett1†, Ross H Albert1, Joseph M Jez1, Haiching Ma2, Trevor M Penning2 and Mitchell Lewis1* Background: Mammalian 3a-hydroxysteroid dehydrogenases (3a-HSDs) Addresses: 1Department of Biochemistry and modulate the activities of steroid hormones by reversibly reducing their C3 Biophysics, The Johnson Research Foundation, 37th and Hamilton Walk, Philadelphia, PA 19104- ketone groups. In steroid target tissues, 3a-HSDs act on 5a-dihydrotestosterone, 6059, USA and 2Department of Pharmacology, a potent male sex hormone (androgen) implicated in benign prostate hyperplasia University of Pennsylvania School of Medicine, 37th and prostate cancer. Rat liver 3a-HSD belongs to the aldo-keto reductase (AKR) and Hamilton Walk, Philadelphia, PA 19104-6084, superfamily and provides a model for mammalian 3a-, 17b- and 20a-HSDs, USA. which share > 65% sequence identity. The determination of the structure of 3a- †Present address: Division of Biology, California + HSD in complex with NADP and testosterone (a competitive inhibitor) will help Institute of Technology, 1200 E California Blvd., to further our understanding of steroid recognition and hormone regulation by Pasadena, CA 91125, USA. mammalian HSDs. *Corresponding author. E-mail: [email protected] Results: We have determined the 2.5 Å resolution crystal structure of recombinant rat liver 3a-HSD complexed with NADP+ and testosterone. The Key words: aldo-keto reductase, crystal structure, structure provides the first picture of an HSD ternary complex in the AKR 3a-hydroxysteroid/dihydrodiol dehydrogenase, superfamily, and is the only structure to date of testosterone bound to a protein. -
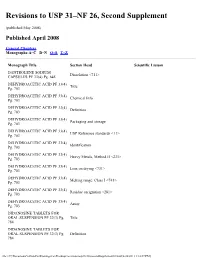
Revisions to USP 31–NF 26, Second Supplement
Revisions to USP 31–NF 26, Second Supplement (published May 2008) Published April 2008 General Chapters Monographs:A–C D–N O–S T–Z Monograph Title Section Head Scientific Liaison DANTROLENE SODIUM Dissolution <711> CAPSULES PF 33(4) Pg. 645 DEHYDROACETIC ACID PF 33(4) Title Pg. 703 DEHYDROACETIC ACID PF 33(4) Chemical Info Pg. 703 DEHYDROACETIC ACID PF 33(4) Definition Pg. 703 DEHYDROACETIC ACID PF 33(4) Packaging and storage Pg. 703 DEHYDROACETIC ACID PF 33(4) USP Reference standards <11> Pg. 703 DEHYDROACETIC ACID PF 33(4) Identification Pg. 703 DEHYDROACETIC ACID PF 33(4) Heavy Metals, Method II <231> Pg. 703 DEHYDROACETIC ACID PF 33(4) Loss on drying <731> Pg. 703 DEHYDROACETIC ACID PF 33(4) Melting range, Class I <741> Pg. 703 DEHYDROACETIC ACID PF 33(4) Residue on ignition <281> Pg. 703 DEHYDROACETIC ACID PF 33(4) Assay Pg. 703 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Title 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Definition 784 file:///C|/Documents%20and%20Settings/rwt/Desktop/revisions/usp31nf26secondSupplement03.html[4/26/2011 1:18:07 PM] DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Packaging and storage 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Labeling 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. USP Reference stadards 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Identification 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Uniformity of dosage units 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. Loss on drying 784 DIDANOSINE TABLETS FOR ORAL SUSPENSION PF 32(3) Pg. -

Yeast DNA Polymerase Zeta ()Is Essential for Error-Free Replication Past Thymine Glycol
Downloaded from genesdev.cshlp.org on September 24, 2021 - Published by Cold Spring Harbor Laboratory Press Yeast DNA polymerase zeta ()is essential for error-free replication past thymine glycol Robert E. Johnson, Sung-Lim Yu, Satya Prakash, and Louise Prakash1 Sealy Center for Molecular Science, University of Texas Medical Branch at Galveston, Galveston, Texas 77555-1061, USA DNA polymerase zeta (Pol) promotes the mutagenic bypass of DNA lesions in eukaryotes. Genetic studies in Saccharomyces cerevisiae have indicated that relative to the contribution of other pathways, Pol makes only a modest contribution to lesion bypass. Intriguingly, however, disruption of the REV3 gene, which encodes the catalytic subunit of Pol, causes early embryonic lethality in mice. Here, we present genetic and biochemical evidence for the requirement of yeast Pol for predominantly error-free replication past thymine glycol (Tg), a DNA lesion formed frequently by free radical attack. These results raise the possibility that, as in yeast, in higher eukaryotes also, Pol makes a major contribution to the replicative bypass of Tgs as well as other lesions that block synthesis by replicative DNA polymerases. Such a preeminent role of Pol in lesion bypass would ensure that rapid cell divisions continue unabated during early embryonic development, thereby minimizing the generation of DNA strand breaks, chromosome aberrations, and the ensuing apoptotic response. [Keywords: DNApolymerase ; thymine glycol; translesion DNAsynthesis; Pol as an extender; error-free translesion DNAsynthesis by Pol ; yeast] Received October 4, 2002; revised version accepted October 31, 2002. Genetic studies in the yeast Saccharomyces cerevisiae et al. 2000b; Washington et al. 2000). Genetic studies in have indicated the requirement of Rad6–Rad18-depen- yeast have additionally indicated a role for Pol in the dent processes in promoting replication of damaged error-free bypass of cyclobutane pyrimidine dimers DNA. -

A Genome-Wide Association Study Lystra P
Hayden et al. Respiratory Research (2018) 19:209 https://doi.org/10.1186/s12931-018-0890-0 RESEARCH Open Access Childhood asthma is associated with COPD and known asthma variants in COPDGene: a genome-wide association study Lystra P. Hayden1,2* , Michael H. Cho2,3, Benjamin A. Raby1,2,3, Terri H. Beaty4, Edwin K. Silverman2,3, Craig P. Hersh2,3 and on behalf of the COPDGene Investigators Abstract Background: Childhood asthma is strongly influenced by genetics and is a risk factor for reduced lung function and chronic obstructive pulmonary disease (COPD) in adults. This study investigates self-reported childhood asthma in adult smokers from the COPDGene Study. We hypothesize that childhood asthma is associated with decreased lung function, increased risk for COPD, and that a genome-wide association study (GWAS) will show association with established asthma variants. Methods: We evaluated current and former smokers ages 45–80 of non-Hispanic white (NHW) or African American (AA) race. Childhood asthma was defined by self-report of asthma, diagnosed by a medical professional, with onset at < 16 years or during childhood. Subjects with a history of childhood asthma were compared to those who never had asthma based on lung function, development of COPD, and genetic variation. GWAS was performed in NHW and AA populations, and combined in meta-analysis. Two sets of established asthma SNPs from published literature were examined for association with childhood asthma. Results: Among 10,199 adult smokers, 730 (7%) reported childhood asthma and 7493 (73%) reported no history of asthma. Childhood asthmatics had reduced lung function and increased risk for COPD (OR 3.42, 95% CI 2.81–4.18). -

The Smooth Muscle-Selective Rhogap GRAF3 Is a Critical Regulator of Vascular Tone and Hypertension
ARTICLE Received 9 Jun 2013 | Accepted 11 Nov 2013 | Published 13 Dec 2013 DOI: 10.1038/ncomms3910 The smooth muscle-selective RhoGAP GRAF3 is a critical regulator of vascular tone and hypertension Xue Bai1, Kaitlin C. Lenhart1, Kim E. Bird1, Alisa A. Suen1, Mauricio Rojas2, Masao Kakoki1, Feng Li1, Oliver Smithies1,2, Christopher P. Mack1,2 & Joan M. Taylor1,2 Although hypertension is a worldwide health issue, an incomplete understanding of its aetiology has hindered our ability to treat this complex disease. Here we identify arhgap42 (also known as GRAF3) as a Rho-specific GAP expressed specifically in smooth muscle cells (SMCs) in mice and humans. We show that GRAF3-deficient mice exhibit significant hypertension and increased pressor responses to angiotensin II and endothelin-1; these effects are prevented by treatment with the Rho-kinase inhibitor, Y27632. RhoA activity and myosin light chain phosphorylation are elevated in GRAF3-depleted SMCs in vitro and in vivo, and isolated vessel segments from GRAF3-deficient mice show increased contractility. Taken together, our data indicate that GRAF3-mediated inhibition of RhoA activity in vascular SMCs is necessary for maintaining normal blood pressure homoeostasis. Moreover, these findings provide a potential mechanism for a hypertensive locus recently identified within arhgap42 and provide a foundation for the future development of innovative hypertension therapies. 1 Department of Pathology and Lab Medicine, University of North Carolina, 501 Brinkhous-Bullitt Building CB 7525, Chapel Hill, North Carolina 27599, USA. 2 McAllister Heart Institute, University of North Carolina, Chapel Hill, North Carolina 27599, USA. Correspondence and requests for materials shouldbe addressed to J.M.T. -

Identification and Characterization of TPRKB Dependency in TP53 Deficient Cancers
Identification and Characterization of TPRKB Dependency in TP53 Deficient Cancers. by Kelly Kennaley A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Molecular and Cellular Pathology) in the University of Michigan 2019 Doctoral Committee: Associate Professor Zaneta Nikolovska-Coleska, Co-Chair Adjunct Associate Professor Scott A. Tomlins, Co-Chair Associate Professor Eric R. Fearon Associate Professor Alexey I. Nesvizhskii Kelly R. Kennaley [email protected] ORCID iD: 0000-0003-2439-9020 © Kelly R. Kennaley 2019 Acknowledgements I have immeasurable gratitude for the unwavering support and guidance I received throughout my dissertation. First and foremost, I would like to thank my thesis advisor and mentor Dr. Scott Tomlins for entrusting me with a challenging, interesting, and impactful project. He taught me how to drive a project forward through set-backs, ask the important questions, and always consider the impact of my work. I’m truly appreciative for his commitment to ensuring that I would get the most from my graduate education. I am also grateful to the many members of the Tomlins lab that made it the supportive, collaborative, and educational environment that it was. I would like to give special thanks to those I’ve worked closely with on this project, particularly Dr. Moloy Goswami for his mentorship, Lei Lucy Wang, Dr. Sumin Han, and undergraduate students Bhavneet Singh, Travis Weiss, and Myles Barlow. I am also grateful for the support of my thesis committee, Dr. Eric Fearon, Dr. Alexey Nesvizhskii, and my co-mentor Dr. Zaneta Nikolovska-Coleska, who have offered guidance and critical evaluation since project inception. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Cdc42 and Rac1 Activity Is Reduced in Human Pheochromocytoma and Correlates with FARP1 and ARHGEF1 Expression
234 P Croisé et al. Rho-GTPase activity in human 23:4 281–293 Research pheochromocytoma Cdc42 and Rac1 activity is reduced in human pheochromocytoma and correlates with FARP1 and ARHGEF1 expression Pauline Croisé1, Sébastien Houy1, Mathieu Gand1, Joël Lanoix2, Valérie Calco1, Petra Tóth1, Laurent Brunaud3, Sandra Lomazzi4, Eustache Paramithiotis2, Daniel Chelsky2, Stéphane Ory1,* and Stéphane Gasman1,* Correspondence 1Institut des Neurosciences Cellulaires et Intégratives (INCI), CNRS UPR 3212, Strasbourg, France should be addressed 2Caprion Proteome, Inc., Montréal, Québec, Canada to S Ory or S Gasman 3Service de Chirurgie Digestive, Hépato-bilaire et Endocrinienne, CHRU Nancy, Hôpitaux de Brabois, Email Vandoeuvre les Nancy, France [email protected] or 4Centre de Ressources Biologiques (CRB), CHRU Nancy, Hôpitaux de Brabois, Vandoeuvres les Nancy, France [email protected] *(S Ory and S Gasman contributed equally to this work) Abstract Among small GTPases from the Rho family, Cdc42, Rac, and Rho are well known to mediate Key Words a large variety of cellular processes linked with cancer biology through their ability to cycle f Rho-GTPases between an inactive (GDP-bound) and an active (GTP-bound) state. Guanine nucleotide f pheochromocytoma exchange factors (GEFs) stimulate the exchange of GDP for GTP to generate the activated f mass spectrometry form, whereas the GTPase-activating proteins (GAPs) catalyze GTP hydrolysis, leading to f Rho-GEF Endocrine-Related Cancer Endocrine-Related the inactivated form. Modulation of Rho GTPase activity following altered expression of Rho-GEFs and/or Rho-GAPs has already been reported in various human tumors. However, nothing is known about the Rho GTPase activity or the expression of their regulators in human pheochromocytomas, a neuroendocrine tumor (NET) arising from chromaffin cells of the adrenal medulla. -

Natural Products As Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors
Reviews Natural Products as Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors Author ABSTRACT Wolfgang Blaschek Glucose homeostasis is maintained by antagonistic hormones such as insulin and glucagon as well as by regulation of glu- Affiliation cose absorption, gluconeogenesis, biosynthesis and mobiliza- Formerly: Institute of Pharmacy, Department of Pharmaceu- tion of glycogen, glucose consumption in all tissues and glo- tical Biology, Christian-Albrechts-University of Kiel, Kiel, merular filtration, and reabsorption of glucose in the kidneys. Germany Glucose enters or leaves cells mainly with the help of two membrane integrated transporters belonging either to the Key words family of facilitative glucose transporters (GLUTs) or to the Malus domestica, Rosaceae, Phlorizin, flavonoids, family of sodium glucose cotransporters (SGLTs). The intesti- ‑ SGLT inhibitors, gliflozins, diabetes nal glucose absorption by endothelial cells is managed by SGLT1, the transfer from them to the blood by GLUT2. In the received February 9, 2017 kidney SGLT2 and SGLT1 are responsible for reabsorption of revised March 3, 2017 filtered glucose from the primary urine, and GLUT2 and accepted March 6, 2017 GLUT1 enable the transport of glucose from epithelial cells Bibliography back into the blood stream. DOI http://dx.doi.org/10.1055/s-0043-106050 The flavonoid phlorizin was isolated from the bark of apple Published online April 10, 2017 | Planta Med 2017; 83: 985– trees and shown to cause glucosuria. Phlorizin is an inhibitor 993 © Georg Thieme Verlag KG Stuttgart · New York | of SGLT1 and SGLT2. With phlorizin as lead compound, specif- ISSN 0032‑0943 ic inhibitors of SGLT2 were developed in the last decade and some of them have been approved for treatment mainly of Correspondence type 2 diabetes. -

Myricetin Antagonizes Semen-Derived Enhancer of Viral Infection (SEVI
Ren et al. Retrovirology (2018) 15:49 https://doi.org/10.1186/s12977-018-0432-3 Retrovirology RESEARCH Open Access Myricetin antagonizes semen‑derived enhancer of viral infection (SEVI) formation and infuences its infection‑enhancing activity Ruxia Ren1,2†, Shuwen Yin1†, Baolong Lai2, Lingzhen Ma1, Jiayong Wen1, Xuanxuan Zhang1, Fangyuan Lai1, Shuwen Liu1* and Lin Li1* Abstract Background: Semen is a critical vector for human immunodefciency virus (HIV) sexual transmission and harbors seminal amyloid fbrils that can markedly enhance HIV infection. Semen-derived enhancer of viral infection (SEVI) is one of the best-characterized seminal amyloid fbrils. Due to their highly cationic properties, SEVI fbrils can capture HIV virions, increase viral attachment to target cells, and augment viral fusion. Some studies have reported that myri- cetin antagonizes amyloid β-protein (Aβ) formation; myricetin also displays strong anti-HIV activity in vitro. Results: Here, we report that myricetin inhibits the formation of SEVI fbrils by binding to the amyloidogenic region of the SEVI precursor peptide (PAP248–286) and disrupting PAP248–286 oligomerization. In addition, myricetin was found to remodel preformed SEVI fbrils and to infuence the activity of SEVI in promoting HIV-1 infection. Moreover, myricetin showed synergistic efects against HIV-1 infection in combination with other antiretroviral drugs in semen. Conclusions: Incorporation of myricetin into a combination bifunctional microbicide with both anti-SEVI and anti- HIV activities is a highly promising approach to preventing sexual transmission of HIV. Keywords: HIV, Myricetin, Amyloid fbrils, SEVI, Synergistic antiviral efects Background in vivo because they facilitate virus attachment and inter- Since the frst cases of acquired immune defciency nalization into cells [4]. -

IL21R Expressing CD14+CD16+ Monocytes Expand in Multiple
Plasma Cell Disorders SUPPLEMENTARY APPENDIX IL21R expressing CD14 +CD16 + monocytes expand in multiple myeloma patients leading to increased osteoclasts Marina Bolzoni, 1 Domenica Ronchetti, 2,3 Paola Storti, 1,4 Gaetano Donofrio, 5 Valentina Marchica, 1,4 Federica Costa, 1 Luca Agnelli, 2,3 Denise Toscani, 1 Rosanna Vescovini, 1 Katia Todoerti, 6 Sabrina Bonomini, 7 Gabriella Sammarelli, 1,7 Andrea Vecchi, 8 Daniela Guasco, 1 Fabrizio Accardi, 1,7 Benedetta Dalla Palma, 1,7 Barbara Gamberi, 9 Carlo Ferrari, 8 Antonino Neri, 2,3 Franco Aversa 1,4,7 and Nicola Giuliani 1,4,7 1Myeloma Unit, Dept. of Medicine and Surgery, University of Parma; 2Dept. of Oncology and Hemato-Oncology, University of Milan; 3Hematology Unit, “Fondazione IRCCS Ca’ Granda”, Ospedale Maggiore Policlinico, Milan; 4CoreLab, University Hospital of Parma; 5Dept. of Medical-Veterinary Science, University of Parma; 6Laboratory of Pre-clinical and Translational Research, IRCCS-CROB, Referral Cancer Center of Basilicata, Rionero in Vulture; 7Hematology and BMT Center, University Hospital of Parma; 8Infectious Disease Unit, University Hospital of Parma and 9“Dip. Oncologico e Tecnologie Avanzate”, IRCCS Arcispedale Santa Maria Nuova, Reggio Emilia, Italy ©2017 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2016.153841 Received: August 5, 2016. Accepted: December 23, 2016. Pre-published: January 5, 2017. Correspondence: [email protected] SUPPLEMENTAL METHODS Immunophenotype of BM CD14+ in patients with monoclonal gammopathies. Briefly, 100 μl of total BM aspirate was incubated in the dark with anti-human HLA-DR-PE (clone L243; BD), anti-human CD14-PerCP-Cy 5.5, anti-human CD16-PE-Cy7 (clone B73.1; BD) and anti-human CD45-APC-H 7 (clone 2D1; BD) for 20 min.